Back and lumbar injuries in tennis are among the most common injuries that occur in this sport. The lower back is the area most often injured by tennis players after the lower and upper extremities. If you play tennis, you have surely suffered from low back pain after a practice.
In this post we will show you the main back pathologies in tennis players. Follow with us and you will know what each one of them is about and what their main causes are. Let's start!
What are the most common types of back and lower back injuries when we play tennis?
There are several common back disorders in tennis and most of them are in the lumbar area. This racket sport involves repetitive rotational, hyperextension and flexion movements of the spine. Performing such movements intensively over and over again is considered a risk factor for these injuries.
It should be noted that some believe that playing tennis during the growth of young people plays a major role in the aetiology of these injuries. This does not raise many expectations when we consider that generally elite tennis players have practiced the sport since their youth.
Below, we show you the most common back and lumbar injuries in tennis players:
Lumbago
Low-back pain is nothing more than the pain produced in the lower back. It can vary from simple muscle pain to a stabbing or burning sensation, lasting a few days or weeks depending on the severity. Moreover, this ailment can worsen with movement (bending, walking, standing, among others) and extend to the leg.
It can be triggered by a sprain or deterioration of the spine. However, it is often attributed to a muscle contracture or overload. Tennis movements that involve the lower back when performed in excess or with poor technique can overload this area and cause low back pain.
Herniated disc
Between the vertebrae that form the column there are elastic discs that function as shock absorbers. These contain a soft material (nucleus pulposus) covered by a resistant elastic band (fibrous ring). When a disc loses its shape and appears to be swollen out of the spine without breaking, it is said to be bulging. On the other hand, a herniated disc is one whose membrane has been pierced or torn.
They are mainly of degenerative aetiology and one of the associated risk factors is forced back movements. A herniated or bulging disc can put pressure on or irritate an adjacent nerve. This causes pain, numbness and weakness in the area of the body associated with such a nerve. If the affected disc is in the neck you will feel these symptoms usually in the shoulder and arm. But if it is in the lower back the effects will be felt in the legs.
Lumbar sprain
It lies in the excessive stretching or rupture (partial or total) of the ligaments present in the lower back. It causes moderate or acute pain in this area that can extend to the buttocks and thighs. In addition, patients with this injury have problems standing, sitting or leaning forward.
It can originate from a fall, blow, accident or improper movement. Athletes and people in general who regularly exert too much stress on the spine are prone to this pathology. Among the sports disciplines with the highest incidence of this injury is tennis.
Lumbar strain
It consists of the partial or total tearing of the muscles and tendons belonging to the lower back. They generally result from forced movements such as lifting heavy objects or sudden twisting of the back. It is therefore very common in sports where this type of movement is performed, including tennis.
Generally this injury causes sudden low back pain that can be aggravated by bending, stretching, coughing and other movements. In addition, it can also cause tenderness, spasms and swelling in the affected area.
Stress fractures of the spine
A stress fracture of the spine occurs when one or more vertebrae suffer small cracks due to overuse. They are common in athletes because of the wear and tear associated with the effort they put into each game or practice. They manifest themselves as pain in the affected area of the back when practising sport or performing certain movements.
They usually occur in the lower back, especially in the lumbar vertebrae L4 and L5. The sacrum also often suffers from these small cracks. When the fracture occurs in the pars interarticularis of one of the vertebrae the injury is called spondylolysis.
Spondylolisthesis
It lies in the displacement of a vertebra from the lower one. It generally occurs in the L4 and L5 vertebrae in the lumbar zone. It can arise due to spondylolysis, trauma, diseases (rheumatological or degenerative) or infections.
One of the usual symptoms is lumbar pain radiating towards the buttocks. Often the spinal cord and nerve roots can be compressed. The latter causes pain, stiffness and weakness in the legs if the injury is located in the lumbar area.
Lumbar arthrosis
This degenerative disease involves the wearing away of the articular cartilage corresponding to the vertebrae in the lumbar area. It causes pain in the lower back, mainly when moving, which can radiate to the buttocks and thighs. In addition, it can also cause stiffness, limited mobility and compression of nerve roots.
Often there is no known direct cause for this condition, although it is known that older people are more prone to it. In addition to ageing, some associated risk factors are: obesity, repetitive use, significant mechanical stress, genetics and injury.
Best products for recovery from tennis back injuries
Bestseller
-
Acupressure Mat and Pillow (Black/Gray)
$49.95 -
Acupressure Mat and Pillow (Green/Navy)
$49.95 -
Acupressure Mat and Pillow (Pink/Bordeaux)
$49.95 -
Acupressure Pillow (Black/Gray)
$29.46 -
Acupressure Pillow (Green/Navy)
$29.46 -
Acupressure Pillow (Pink/Bordeaux)
$29.46 -
Back Support Belt (Black)
$34.95 -
Back Support Belt (Green)
$34.95 -
Back Support Belt (Pink)
$34.95 -
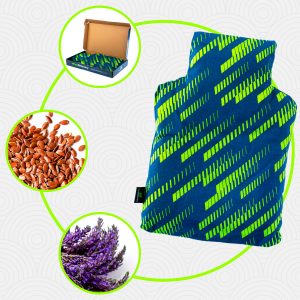
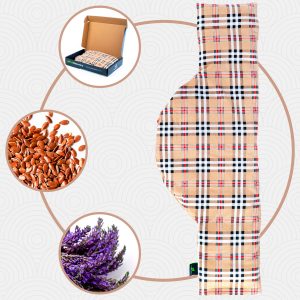
Heating Pad for Microwave Classic Bottle Shaped (Hearts)
$19.95 -
Heating Pad for Microwave Classic Bottle Shaped (Oxford)
$19.95 -
Heating Pad for Microwave Classic Bottle Shaped (Sport)
$19.95 -
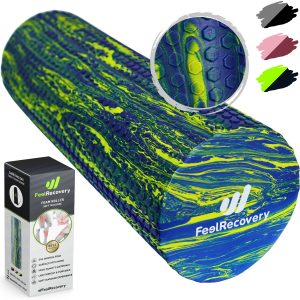
High Density Foam Roller for Muscle (Black/Gray)
$29.95 -
High Density Foam Roller for Muscle (Green/Navy)
$29.95 -
High Density Foam Roller for Muscle (Pink/Bordeaux)
$29.95 -
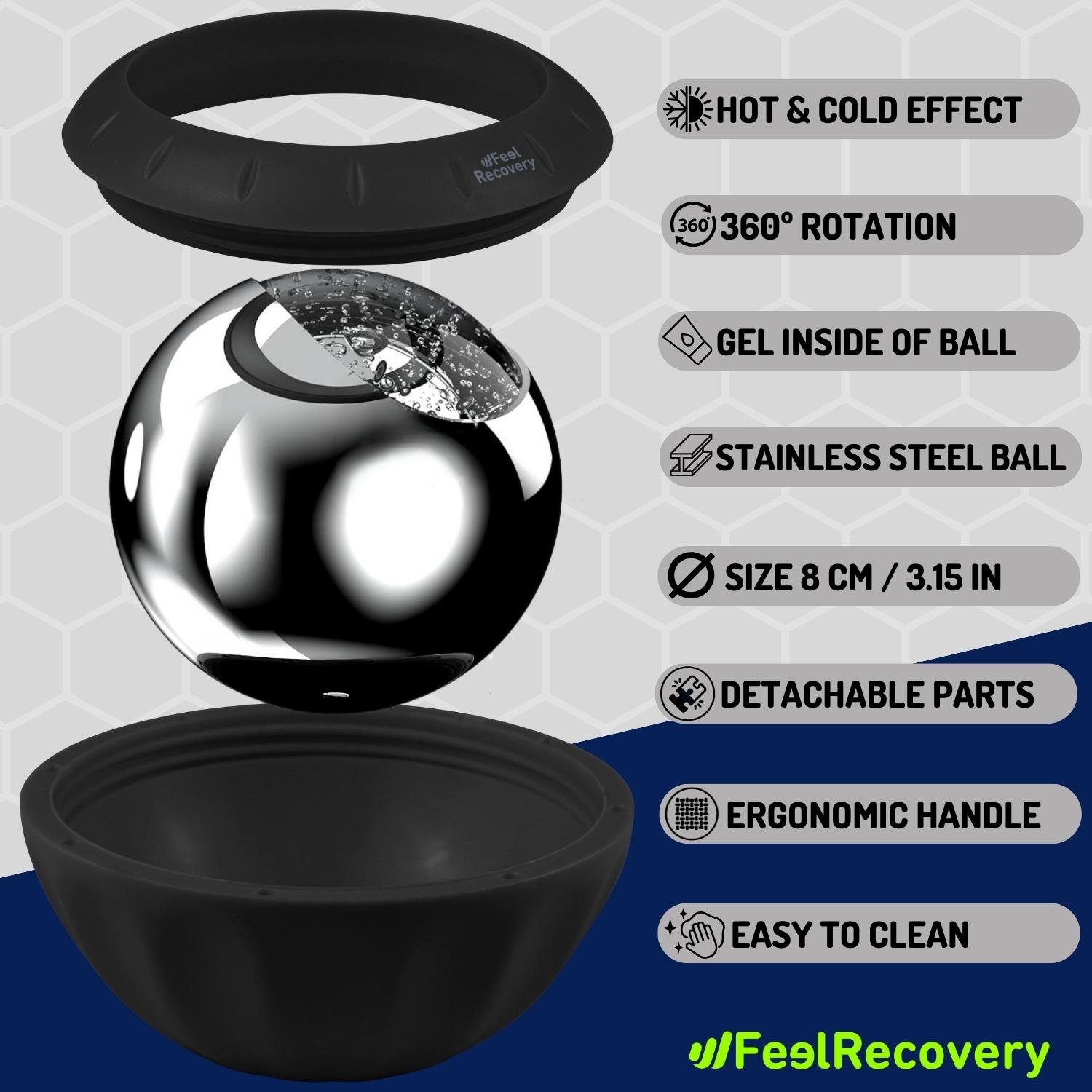
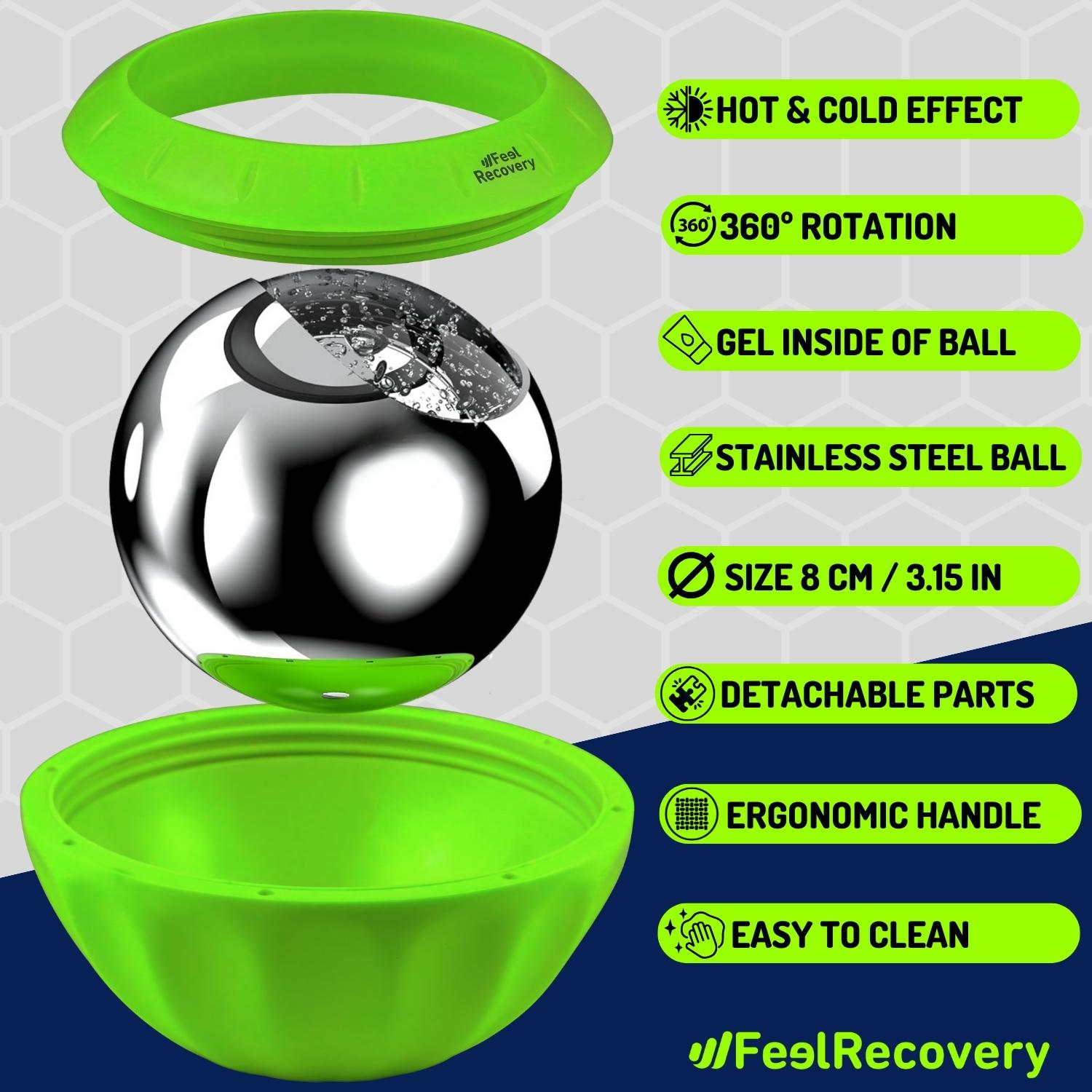
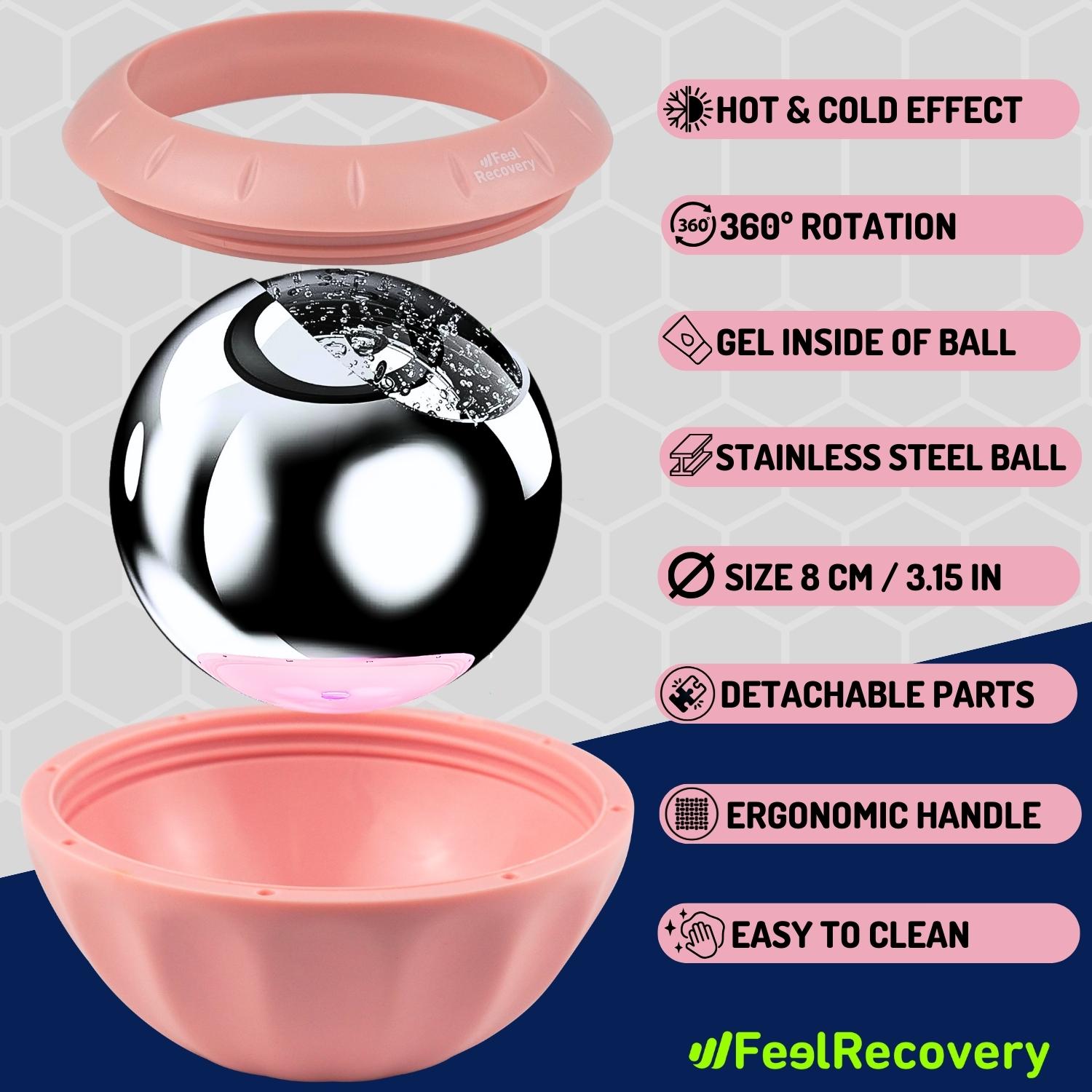
Ice Massage Roller Ball (Black)
$39.95 -
Ice Massage Roller Ball (Green)
$39.95 -
Ice Massage Roller Ball (Pink)
$39.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Hearts)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Oxford)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Sport)
$29.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Hearts)
$24.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Oxford)
$24.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Sport)
$24.95 -
Microwaveable Heating Pad for Pain Relief (Hearts)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Oxford)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Sport)
$19.95 -
Pack 2 In 1 Foam Roller High + Soft Density (Black/Gray)
$29.95 -
Pack 2 In 1 Foam Roller High + Soft Density (Green/Navy)
$29.95 -
Pack 2 In 1 Foam Roller High + Soft Density (Pink/Bordeaux)
$29.95 -
Soft Density Foam Roller for Recovery (Black)
$29.95 -
Soft Density Foam Roller for Recovery (Green)
$29.95 -
Soft Density Foam Roller for Recovery (Pink)
$29.95 -
Trigger Point Massage Stick (Black)
$14.95 -
Trigger Point Massage Stick (Green)
$14.95 -
Trigger Point Massage Stick (Pink)
$14.95
How to apply RICE therapy to treat back injuries in tennis players?
The RICE therapy is a protocol that we can apply to treat an injury. Each letter that makes up your name corresponds to the initials of the four steps of this methodology.
In addition to this method we can find others in the literature, such is the case of the PRICE therapy. This is really an update of the RICE protocol, as it takes all the steps of the latter and adds a new one: protection. However, the RICE therapy is the best known of the two.
Here we show you the steps of the PRICE protocol:
- Protection: This is the first step and consists of protecting the injured area. In this way, sporting activities and harmful movements are prohibited. The use of immobilisers such as braces or joint supports is essential in many scenarios.
- Rest: Next, the affected area must be given due rest (generally for 48 hours). It is important to make movements that do not harm the patient to avoid stiffness.
- Ice: In this step cryotherapy is applied to the lesion to take advantage of the anti-inflammatory and analgesic properties of the cold. You only have to place a cold compress at 10 or 20 °C over the lesion. Each session should last 20 minutes maximum as too cold could be harmful. You can do between 6 and 8 sessions a day.
- Compression: You should compress the wound to give firmness and promote circulation, helping to reduce inflammation. You can use a somewhat flexible tissue that allows safe movement. Do not press too hard or you will cut off the circulation.
- Elevation: Elevating the injury helps to reduce inflammation and relieve pain. You should only support the affected area on a cushioned surface (such as a pillow) raising it to a level above the heart. You can perform this step in periods of rest perfectly.
References
- Hainline, B. (1995). Low back injury. Clinics in Sports Medicine, 14(1), 241-265. https://europepmc.org/article/med/7712553
- Campbell, A., Straker, L., O’Sullivan, P., Elliott, B., & Reid, M. (2013). Lumbar loading in the elite adolescent tennis serve: link to low back pain. Med Sci Sports Exerc, 45(8), 1562-1568. https://europepmc.org/article/med/23470302
- Silva, R. T. D., De Bortoli, A., Laurino, C. F. D. S., Abdalla, R. J., & Cohen, M. (2006). Sacral stress fracture: an unusual cause of low back pain in an amateur tennis player. British Journal of Sports Medicine, 40(5), 460-461. https://bjsm.bmj.com/content/40/5/460.short
- Alyas, F., Turner, M., & Connell, D. (2007). MRI findings in the lumbar spines of asymptomatic, adolescent, elite tennis players. British journal of sports medicine, 41(11), 836-841. https://bjsm.bmj.com/content/41/11/836.short
- Campbell, A., O'Sullivan, P. E. T. E. R., Straker, L., Elliott, B., & Reid, M. (2014). Back pain in tennis players: a link with lumbar serve kinematics and range of motion. Medicine and science in sports and exercise, 46(2), 351-357. https://europepmc.org/article/med/23877374
- Abrams, G. D., Renstrom, P. A., & Safran, M. R. (2012). Epidemiology of musculoskeletal injury in the tennis player. British journal of sports medicine, 46(7), 492-498. https://bjsm.bmj.com/content/46/7/492.short
- Chandler, T. J. (1995). Exercise training for tennis. Clinics in sports medicine, 14(1), 33-46. https://europepmc.org/article/med/7712556
- Nirschl, R. P. (1988). Prevention and treatment of elbow and shoulder injuries in the tennis player. Clinics in Sports Medicine, 7(2), 289-308. https://www.sciencedirect.com/science/article/abs/pii/S0278591920309364
- Eygendaal, D., Rahussen, F. T. G., & Diercks, R. L. (2007). Biomechanics of the elbow joint in tennis players and relation to pathology. British journal of sports medicine, 41(11), 820-823. https://bjsm.bmj.com/content/41/11/820.short
- Perkins, R. H., & Davis, D. (2006). Musculoskeletal injuries in tennis. Physical Medicine and Rehabilitation Clinics, 17(3), 609-631. https://www.pmr.theclinics.com/article/S1047-9651(06)00031-3/fulltext