- What is dysmenorrhoea or menstrual pain?
- Best products to relieve period pain
- What are the different types of dysmenorrhoea?
- How do we know if we have dysmenorrhoea?
- What causes menstrual cramps and what causes them?
- What are the symptoms of severe menstrual cramps?
- How can we relieve painful menstrual periods through complementary therapies and without medication?
- Why should we avoid taking pills and self-medicating to relieve menstrual pain?
- When is it necessary to see a doctor if we have unbearable menstrual pain?
Need menstrual pain relief? Cramps and period pains are common and can be disabling or, at the very least, very annoying. We find out exactly what it is and how you can identify it and, of course, end up helping you to treat menstrual cramps in the most natural and effective way possible, making you aware of everything you need to know about both the condition itself and the different ways to treat it.
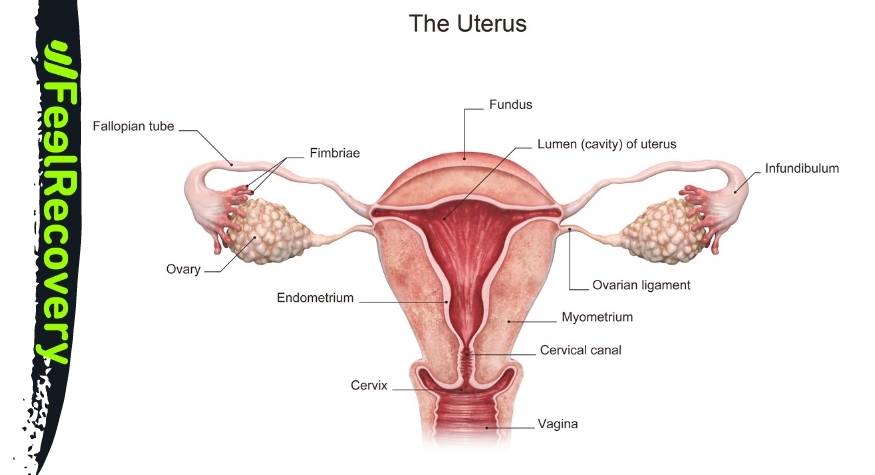
The human body is very complex, and even more so in women. Every month there is a biological condition called menstruation in which the endometrium that has formed on the uterus is expelled, as long as the egg has not been fertilised. This presents as bleeding through the vagina, which sometimes includes endometrial clots, but it also usually comes with other symptoms, including the pain that we want to discuss in this post.
What is dysmenorrhoea or menstrual pain?
Dysmenorrhoea is a pain that occurs during the days of menstruation, that is, when a woman loses her endometrium and bleeds through the vagina. It would also include premenstrual pain.
In particular, dysmenorrhoea refers to pain in the lower abdomen, including the pelvis and abdomen. However, as a woman, you probably already know that this is not the only symptom. The concept refers to this but, of course, we can suffer from other symptoms such as back pain, thigh pain, headaches, etc.
The pain can be constant or present itself as spasms, pricks or even contractions, varying in duration and intensity depending on the cause, pain threshold, drug intake and other aspects that we will see throughout this post.
Best products to relieve period pain
Bestseller
-
Heating Pad for Microwave Classic Bottle Shaped (Hearts)
$24.95 -
Heating Pad for Microwave Classic Bottle Shaped (Oxford)
$24.95 -
Heating Pad for Microwave Classic Bottle Shaped (Sport)
$24.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Hearts)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Oxford)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Sport)
$29.95 -
Microwaveable Heating Pad for Pain Relief (Hearts)
$24.95 -
Microwaveable Heating Pad for Pain Relief (Oxford)
$24.95 -
Microwaveable Heating Pad for Pain Relief (Sport)
$24.95
What are the different types of dysmenorrhoea?
Dysmenorrhoea or painful menstruation is classified into two main types:
Primary dysmenorrhoea
This is conventional menstrual pain that occurs for natural biological reasons. The woman menstruates and, with it, there is a symptomatic picture that includes, in most cases, among other symptoms, the aforementioned pain. This symptom is common, typical of the first days of the cycle and more or less bearable. It includes pain with or without spasms due to the contraction of the uterus, which moves to get rid of the endometrium.
It occurs during adolescence (from six months after the first menstrual period or menarche) and also in youth, and may continue into adulthood. If this occurs, you should be aware that the symptoms become milder and milder, especially after pregnancy.
Secondary dysmenorrhoea
This is pain, sometimes delayed and sometimes direct, caused by pelvic abnormalities, chronification of pathologies and basically advanced age. In general, abnormalities affecting any pelvic viscera will cause pain. This pain is stronger, variable according to the cause and the aggravating factors are age, if there is chronification of the pain, etc.
It is not common at an early age, unless the patient suffers from these pathologies. It usually appears in adulthood and, although at first the pain and the other symptoms that go hand in hand are quite intense, over the years the symptoms become chronic. When the cause is not cured, the symptoms multiply both in extent and severity (an infection, for example).
More symptoms also appear as a result of the diseases that cause secondary dysmenorrhoea. We will look at all of them below.
How do we know if we have dysmenorrhoea?
Knowing the classification of dysmenorrhoea and with what you will read below, it will not be difficult to identify menstrual pain, differentiating it from other pain and, in turn, knowing whether it is primary or secondary, which is really important.
In short, the symptoms of this ailment are mainly that the pain occurs in the lower abdomen, abdomen and pelvis, which may or may not extend to the upper thighs and lower back. In addition, it is very common for spasms or twinges to appear. Menstrual pain will occur during the days of bleeding or prior to bleeding. Therefore, if you are suffering from it during this period of time and then it subsides, it has already been identified.
If you have pain in your ovaries, uterus, pelvis or, in general, in the area where your reproductive system is located when you are not bleeding (or just before your period), see your doctor because it is very likely that it is not menstrual pain.
Dysmenorrhoea does not involve stomach pain, so it is important to identify this. Do not confuse nausea, which can occur during menstruation, with stomach pain. This symptom is not related to the reproductive system and therefore has nothing to do with it.
In addition to the pain, if you see other symptoms that coincide with the ones we will see later, it would be strange if you do not have dysmenorrhoea. However, you must identify what type it is, whether it is primary or secondary dysmenorrhoea. This is essential so that, in the case of secondary dysmenorrhoea, you can look for its causes and treat them accordingly, according to a gynaecological professional.
If in doubt or suspecting that you have secondary dysmenorrhoea, see your doctor to get a diagnosis of the cause so that you can start treating it as soon as possible. This will ensure that you do not suffer from other symptoms and, at the same time, you will be able to reduce or eliminate other related pains.
What causes menstrual cramps and what causes them?
The causes of menstrual cramps include:
- Menstruation: Menstruation itself and what it entails for our body is the cause of many symptoms, especially in the younger years. This means that we suffer from them without there being a gynaecological cause, there is no pathology behind them, only the changes that menstruation brings (nausea, headache, fluid retention, pain and cramps). There are basically two points: the contractions of the uterus to detach the endometrium and the hormonal change. These are responsible for virtually all symptoms of menstrual pain.
- Prostaglandin and arachidonic acid: Primary dysmenorrhoea is basically caused by an imbalance of chemicals in the body. There is an excess of prostaglandins and arachidonic acid. These are responsible for controlling uterine contractions, which are enhanced.
- Contractions of the uterus: As we have just seen, these occur when the chemicals necessary to expel the endometrium are produced once each time (when we menstruate). The contractions, which in themselves cause pain in the area, can pinch tissues and affect the circulatory system, diverting the supply of nutrients and causing pain in nearby muscles, such as in the pelvic or lower back area.
- Endometriosis: This is the abnormal growth of endometrial tissue, which continues to grow on the outside of the uterus, in the pelvis or in the cavity of the abdomen. This means that its pressure causes pain in the area.
- Pelvic inflammatory disease: This occurs before the end of the period but is not related to it. In fact, this infection becomes more widespread and aggravated, with an increasing diversity of symptoms, which become more intense and frequent.
- Infections in the uterine cavity: Many of the infections we have in this cavity will worsen and, in fact, also cause the appearance of some of the symptoms that occur during menstruation. In fact, dysmenorrhoea is the clearest example of this, even modifying the type of pain, which becomes sharp, stabbing, lacerating, discriminating very well from conventional menstrual pain.
- Uterine adenomyosis: This is the enlargement of the uterus due to the presence of endometrial glands and stroma in the muscular tissue of the uterus. This means, firstly, that the endometrium is sometimes larger, leading to more bleeding, and secondly, that the larger uterus presses on the other elements when it contracts.
- Foreign bodies: The presence of foreign bodies can interfere with the activity of the uterus, which moves during these days of the month. Obviously, a misplaced endometrium is also hit by these elements, which can be biological, such as fibroids and uterine fibroids, polyps and cysts, or foreign with a copper IUD.
- Fatigue, illness or an impaired immune system: Any of these circumstances will make menstrual symptoms worse, with pain being stronger, cramps more numerous, dizziness easier to produce, etc.
What are the symptoms of severe menstrual cramps?
Although menstruation is natural, basic and common, dysmenorrhoea is accompanied by many other symptoms, which we will discuss below:
- Pelvic pain with contractions: Stronger contractions cause the pain to increase. These are more intense simply because they generate more prostaglandin. As a result, there is less blood flow to the uterus, which also causes pain. This can become chronic, which is caused by a pathology such as endometriosis.
- Cramps in the lower abdomen: Cramps do not usually occur with primary dysmenorrhoea, but they do in secondary dysmenorrhoea, as they are caused by other diseases that we have already discussed. They can become chronic, resulting in a continuous dull ache. Cramps caused by primary dysmenorrhoea tend to ease with consecutive menstrual periods and after pregnancy.
- Pelvic or abdominal cramps: Cramps that occur in the abdomen are not normally caused by menstruation, although they do occur during these days. They are usually caused by endometriosis and other problems. Even so, they are still an obvious cause of menstrual pain by their very definition.
- Ovarian twinges: The reproductive system is swollen and pressurised, which causes twinges in weak or sensitive organs and organelles, such as the ovaries. They will disappear as the swelling goes down.
- Pain in the lower back and thighs: This is referred pain. It is caused by the contractions that occur in the uterus, not because of the contractions themselves, but because they can prevent the supply of oxygen to the muscles in these areas.
- Swollen, tender and sore breasts: Touching your breasts can be unpleasant and even painful. Visually they look bigger and you will also feel fuller. The pain is caused by progesterone; the swelling is caused by progesterone and prolactin. Both can cause the tissue to swell. Fluid retention also increases the volume of the breasts.
- Nausea: Nausea is caused by the presence of prostaglandin in the blood. It is also caused by a change in hormones, however small (apart from the one we have just mentioned). In the stomach, more gastric juices are produced which contain hydrochloric acid, an intense element that our organism tries to expel in a natural way by moving it up the oesophagus, through gagging and vomiting.
- Dizziness: This is common due to the loss of blood, which leaves us weakened because it takes with it essential elements for the normal functioning of our organism (especially iron).
- Fatigue: If this is significant, it may be due to one of the pathologies associated with secondary dysmenorrhoea. There are problems which, because of the way they occur or for other reasons, make us feel tired or exhausted for no apparent reason, much more quickly than usual.
- Abdominal bloating: This is caused by fluid retention and usually disappears during the period. It is a common symptom during menstruation and, above all, a few days before, but of course, depending on how it occurs, it can cause pain. It is a hormonal reason, with progesterone and oestrogen being the main players.
- Weight gain: This is a consequence of fluid retention. It is not a real increase, because as you urinate it will disappear. In addition, you may gain a few grams because you change your diet, something we tend to do due to emotional changes.
- Constipation: The extra progesterone that is generated in the days before menstruation is the cause of lower intestinal motility. It is the intestines that favour the expulsion of faeces and their low motility delays this expulsion.
- Headache: As in the case of nausea, it is the hormone prostaglandin in the blood that causes it. The same happens because of the rapid drop in oestrogen. This means that there is no cure, you cannot get rid of a period headache, only alleviate the symptoms. If you do get menstrual headaches, you will differentiate them because they include aura, blind spots or flashes and even having a numb face with tingling.
- Food cravings: Again, it's hormones that cause cravings. Their fluctuation causes neurotransmitters to modify the messages that reach the brain. Sweet, fatty and carbohydrate foods are most in demand (the serotonin in these make us feel better, happier).
- Mood swings and irritability: And, once again, hormones. We feel sad, everything affects us more, we get irritable and can easily get into a bad mood. It is progesterone that is responsible for this by affecting the concentration of gamma butyric acid, increasing irritability and nervousness. There is also a decrease in the secretion of noradrenaline, which is what keeps us in a good mood.
How can we relieve painful menstrual periods through complementary therapies and without medication?
It is important to know that there are many ways to reduce or even eliminate menstrual pain without resorting to pills or other medications. Complementary and alternative therapies, as non-invasive therapies are called, have many benefits for our bodies, and one of them is the successful treatment of pain of various kinds.
Let's take a look at the best alternative therapies for treating dysmenorrhoea:
Thermotherapy
Applying heat to areas of non-acute pain is a simple and non-negative way of reducing this symptom. The pressure is reduced, the capillaries dilate and there is a sedative effect.
All you have to do is get hold of a product such as a thermal pillow for microwaves etc. and place it, once warm, on the area that hurts. It is also very useful to take a hot shower (or better a bath) or go to a sauna, the effects are the same.
As well as soothing the pain, it reduces cramps and even improves your mood, as you will feel calm, serene and peaceful, with a calm and focused mind. This also helps to take the focus off the pain we suffer and relax more. Remember that the temperature should never be too high and that overuse of this method can lead to drowsiness and dizziness (typical of menstrual symptoms).
Massage therapy
You can perform a very simple self-massage to soothe menstrual cramps. We are not talking about a decontracting manoeuvre or similar, but about a delicate and relaxing work that includes the following steps:
- Lying down or lying on a chair.
- Use vegetable oil to act as a lubricant. Try using an oil of ginger, cinnamon, chamomile, white willow, anise, valerian or sage, or make your own. Including these ingredients will also help to reduce both the tension in the tissues and the pain itself.
- It should be applied gently and in the pelvic area.
- Start by applying circular movements just around the navel and in a clockwise direction, thus activating the blood circulation.
- As you get used to this manipulation, apply more pressure, but never feel pain from the massage itself.
- Use both hands.
- Hold this movement for two minutes.
- The other massage movement for periods is the up and down stroking movement, from the upper navel to the pubic area.
- Apply heat to the area for 15 minutes just before the self-massage.
Acupressure therapy
Acupressure consists of the manipulation of some very particular points of our body to try to heal other pathologies that occur in any area, whether internal or external. To relieve menstrual pain with acupressure we have three options or points to work on.
We encourage you to try it yourself with the following indications:
- Hegu point: Between fingers 1 and 2, between metacarpals 1 and 2, on the back of the hand. Apply moderate pressure and draw small circles. It is used to treat pain in general and headache in particular.
- Sanyinjiao point: This point is about 5 centimetres above the prominent inner ankle bone, on the tibia. It is very sensitive so its palpation is often painful. Even so, do not hesitate to exert moderate pressure. It reduces pelvic disorders, including reducing the intensity of cramps and thus pain.
- Taichong point: It is located between metatarsals 1 and 2, between toes 1 and 2. It is a general regulator of menstruation and reduces anxiety and pain.
How to apply acupressure therapy correctly?
- Massage each point for one minute.
- Do this for five days immediately prior to menstruation.
- Repeat twice a day.
- During your period, especially when the pain is stronger, try to increase the frequency.
By working on the three points with the given guidelines, you not only reduce the intensity of menstrual pain, but also make it last for fewer days.
Other effective alternative therapies
In addition to the above therapies, there are other ways to treat menstrual pain which, as you will see, are also simple, effective and highly recommended for your health.
- Natural remedies using plants: Take fennel, ginger tea or lemon in hot infused drinks. As we have seen, create your own massage lotion with the plants listed in the previous section (ginger, cinnamon, chamomile, white willow, anise, valerian or sage). Use essences of these plants to infuse or take relaxing baths.
- Acupuncture: This is done by working on the same points as detailed in the acupressure section. However, on this occasion, finger pressure will not be used, but very thin needles specific for this therapy will be stuck into the points. A professional must be consulted because the technique must be known in order to introduce the needles at certain millimetres into the dermis and in the corresponding degrees in each case.
- Kinesiotherapy: In this case, the star resource will be the Kinesiotape (neuromuscular bandage), an elastic cotton tape that faithfully emulates the characteristics of the epidermis, having an adhesive side. Josya Sijmonsma recommends it and offers data on its effectiveness in the book "Neuromuscular Bandage Manual". We place this bandage crosswise, from the navel to the pubis and between the iliac spines, just at the front. At the back, only a small horizontal bandage is necessary. Its placement is quite complex, so it must be a professional in kinesiotherapy who is in charge of doing it according to specific values.
- Osteopathy: Manual therapy or osteopathy will help you in a really simple way. Manipulation to avoid restriction of lumbar mobility, correction of the diaphragm and uterus as well as sympathetic inhibition of the L1, L2 and L3 vertebrae and stimulation of the parasympathetic sacrum should be carried out. The pain is less intense and lasts for fewer days.
- Cutaneous electrostimulation: Transcutaneous nerve electrostimulation can be used. This is an electric current that stimulates the nerve fibres through skin stimulation. This releases endorphins, which are analgesic, and improves the pain threshold, so that it has to be more intense for us to perceive it.
- Relaxation: There are different postures and stretches used in relaxation sessions that you can easily do at home. It is all about focusing on the moment, doing harmonious and slow postures, controlling your breathing and trying to relax as much as possible.
Why should we avoid taking pills and self-medicating to relieve menstrual pain?
Firstly, self-medication is one of the main health problems in our society. While it is true that broad-spectrum medications are generally prescribed for typical ailments, we do not all function in the same way, nor does our body have the same reaction to a drug as anyone else's. This means that we should not make our own decisions. This means that we should not make our own decisions when it comes to medication.
On the other hand, any pill for menstrual pain has side effects. Some are obvious and some are not so obvious. This means that, even if we do not notice them in the short term, everything we take will have a negative impact, to a greater or lesser extent.
When is it necessary to see a doctor if we have unbearable menstrual pain?
In general, during the first years of menstruation, suffering from primary dysmenorrhoea, there are uterine contractions and cramps accompanied by pain in the area, in the pelvis and sometimes reaching the back. Headache, bloating and the urge to vomit may also be normal. Psychologically you may also feel more irritable and vulnerable, becoming sad more easily, suffering from mental fatigue, etc.
The following are not considered "normal" and should be seen by a medical professional:
- If you are over 25 or 30 and new symptoms are appearing. These are typical of secondary dysmenorrhoea, which we have already seen appears later and as a consequence of some circumstance, generally treatable and which, in fact, can aggravate as well as create or promote other problems.
- Also if you notice that the symptoms are getting worse month by month.
- If the treatments recommended by your doctor do not mitigate the symptoms.
- If your first severe cramps occur after the age of 25.
- If you have a fever as a result.
- If the pain persists or appears when you are not menstruating.
- If premenstrual symptoms continue during the second phase of your period.
References
- Latthe, P. M., & Champaneria, R. (2011). Dysmenorrhoea. BMJ clinical evidence, 2011. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3275141/
- Armour, M., Parry, K., Manohar, N., Holmes, K., Ferfolja, T., Curry, C., ... & Smith, C. A. (2019). The prevalence and academic impact of dysmenorrhea in 21,573 young women: a systematic review and meta-analysis. Journal of women's health, 28(8), 1161-1171. https://www.liebertpub.com/doi/abs/10.1089/jwh.2018.7615
- Ju, H., Jones, M., & Mishra, G. (2014). The prevalence and risk factors of dysmenorrhea. Epidemiologic reviews, 36(1), 104-113. https://academic.oup.com/epirev/article/36/1/104/566554
- Grandi, G., Ferrari, S., Xholli, A., Cannoletta, M., Palma, F., Romani, C., ... & Cagnacci, A. (2012). Prevalence of menstrual pain in young women: what is dysmenorrhea?. Journal of pain research, 169-174. https://www.tandfonline.com/doi/full/10.2147/JPR.S30602
- Parker, M. A., Sneddon, A. E., & Arbon, P. (2010). The menstrual disorder of teenagers (MDOT) study: determining typical menstrual patterns and menstrual disturbance in a large population‐based study of Australian teenagers. BJOG: An International Journal of Obstetrics & Gynaecology, 117(2), 185-192. https://obgyn.onlinelibrary.wiley.com/doi/abs/10.1111/j.1471-0528.2009.02407.x
- Anastasakis, E., Kingman, C. E., Lee, C. A., Economides, D. L., & Kadir, R. A. (2008). Menstrual problems in university students: an electronic mail survey. in vivo, 22(5), 617-620. https://iv.iiarjournals.org/content/22/5/617.short
- Jo, J., & Lee, S. H. (2018). Heat therapy for primary dysmenorrhea: A systematic review and meta-analysis of its effects on pain relief and quality of life. Scientific reports, 8(1), 16252. https://www.nature.com/articles/s41598-018-34303-z
- Igwea, S. E., Tabansi-Ochuogu, C. S., & Abaraogu, U. O. (2016). TENS and heat therapy for pain relief and quality of life improvement in individuals with primary dysmenorrhea: a systematic review. Complementary therapies in clinical practice, 24, 86-91. https://www.sciencedirect.com/science/article/abs/pii/S1744388116300329
- Ozgoli, G., Goli, M., & Moattar, F. (2009). Comparison of effects of ginger, mefenamic acid, and ibuprofen on pain in women with primary dysmenorrhea. The journal of alternative and complementary medicine, 15(2), 129-132. https://www.liebertpub.com/doi/abs/10.1089/acm.2008.0311
- French, L. (2005). Dysmenorrhea. American family physician, 71(2), 285-291. https://www.aafp.org/pubs/afp/issues/2005/0115/p285.html