- Definition: What is plantar fasciitis or inflammation of the fascia of the foot?
- What are the causes and risk factors for plantar fasciitis?
- Best products for foot pain relief
- Main symptoms that warns us that we have inflammation of the fascia of the foot
- What treatments are available to relieve pain and cure plantar fasciitis?
- What are the most effective prevention methods for plantar fasciitis?
- F.A.Q: Frequently Asked Questions
Among podiatric conditions, plantar fasciitis is a disorder that usually subsides with conservative treatment, 95% of cases of foot fasciitis are curable, although the process of improvement is gradual and slow. Of course, this requires medical examination, rest, physiotherapy and other conservative therapies.
If you want to know what this plantar fascia injury is all about, we invite you to continue reading this post until the end. We will show you in an easy way why this ailment arises and how you can prevent it. Don't miss the frequently asked questions about this inflammation of the sole of the foot.
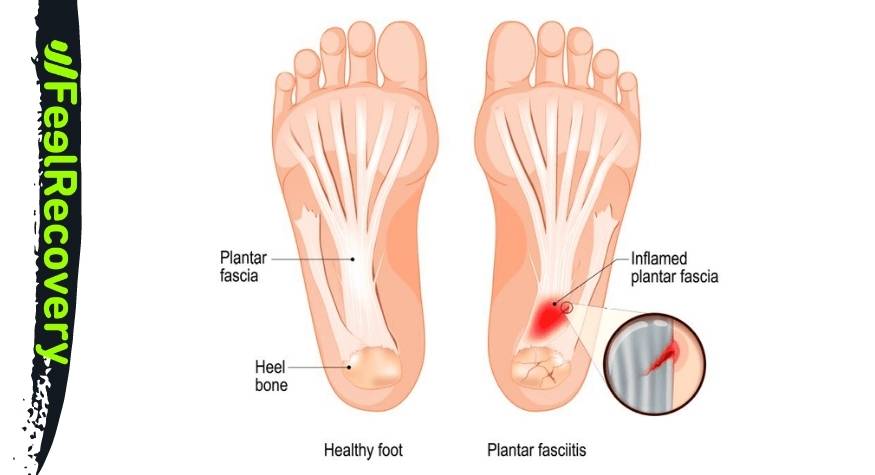
Definition: What is plantar fasciitis or inflammation of the fascia of the foot?
Plantar fasciitis is an irritation of the connective tissue or fascia located on the bottom of the feet. This thick, fibrous tissue connects the calcaneal bone from the heel to the base of the toes, under normal conditions it gives structure to the tissues, supports and helps maintain the plantar arch. However, due to overuse, overweight and other factors, it tends to become inflamed.
This gives rise to a sharp, focused pain at the inferomedial level of the heel, which is the typical symptom of this injury. Although few cases are serious and it is a common disorder in the population, it is a disabling condition for the patient because it prevents them from exercising, moving, walking or standing for long periods of time. If not treated in time, it can worsen into a chronic condition that can lead to more serious complications.
What are the causes and risk factors for plantar fasciitis?
As you might expect runners, gymnasts and footballers are prone to inflammation of their fascia, but top athletes are not the only ones affected. At least 11% of the population has suffered from plantar fasciitis, while women over the age of 50 are more likely to suffer from the condition.
But these are not the only factors, there are several causes that can lead to plantar fasciitis. Let's take a closer look at what they are:
- Overuse of the feet: The feet are relatively small areas of the body that constantly support the entire body weight, exert walking force and are almost permanently stressed. When walking too much, standing for too long or in a bad position, the fascia also swells. In the midst of the stance phase of walking, the plantar fascia is subjected to continuous microtrauma and traction, which can lead to inflammation.
- Gait disturbance: When the foot throws the load to the inner side (pronation) in the gait, plantar fasciitis is likely to occur. This can be treated and diagnosed after a foot strike study to improve the patient's clinical situation.
- Muscle shortening: If any muscle close to the joint of the foot is tight, the fascia will suffer. Perhaps the muscle overstretching is due to biomechanical disorders, tendonitis, contractures or rheumatic diseases.
- Overweight: Excessive weight gain exposes the tissues of the foot to continuous overstress. Such extra pressure causes the fascia to swell easily increasing the chances of the occurrence of plantar fasciitis.
- Wearing heels: The use of heels in shoes generates various disorders in the locomotor system, including plantar fasciitis. This is due to the exaggerated exposure of muscles and tendons (e.g. Achilles tendon) to shortening. In addition, it alters the stride, causing increased stress on the fascia.
- Wearing inappropriate footwear: It is not only high heels that can cause an injury to the fascia, but also any footwear that alters the stride. For example, shoes that are too tight or too loose or even those that expose the sole to a very hard surface.
- Doing demanding work: Any activity that involves the foot being supported or propelling the body exposes the foot to increased stress. Of course, if not rested properly, the chances of injury to the fascia are increased.
- Inadequate body training: Exercise routines that require stress on the foot in a stance position predispose the foot to injury. This is also the case when starting intensive physical activity without proper conditioning is detrimental. Even if there is already a stressful condition for the fascia and a thorough warm-up is not carried out.
- Anatomical deformities: Certain biomechanical abnormalities in the locomotor system also play a role in plantar fasciitis. For example, uneven limbs, bone spurs, flat feet and cavus feet, among others. However minor they may seem, they end up affecting the continuous fascial structure in the long term.
- Age of the patient: Like other body tissues, fascia also loses elasticity, stiffness and strength over time. This is why it is common to see people between 40 and 60 years of age with this syndrome.
- Inadequate nutrition: Lack of nutrients in the body means that the body's tissues do not function properly. For this reason, the fascia can suffer if the levels of calcium, magnesium, collagen and others are low.
Best products for foot pain relief
Bestseller
-
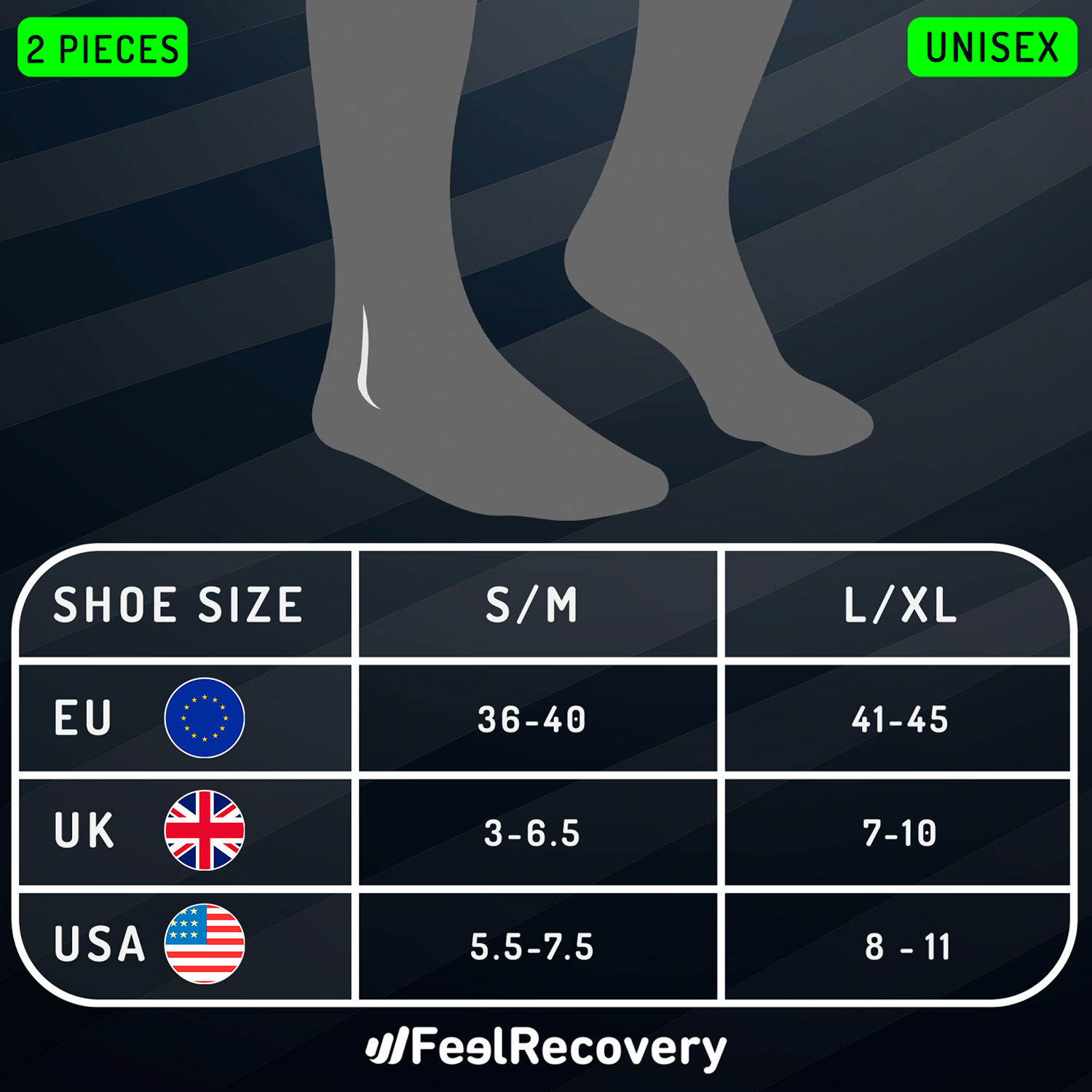
2 Ankle Compression Sleeve (Black/Gray)
$19.95 -
2 Ankle Compression Sleeve (Green/Navy)
$19.95 -
2 Ankle Compression Sleeve (Pink/Bordeaux)
$19.95 -
Acupressure Mat and Pillow (Black/Gray)
$49.95 -
Acupressure Mat and Pillow (Green/Navy)
$49.95 -
Acupressure Mat and Pillow (Pink/Bordeaux)
$49.95 -
Acupressure Pillow (Black/Gray)
$29.46 -
Acupressure Pillow (Green/Navy)
$29.46 -
Acupressure Pillow (Pink/Bordeaux)
$29.46 -
Foot Massage Roller for Plantar Fasciitis (Black)
$19.95 -
Foot Massage Roller for Plantar Fasciitis (Green)
$19.95 -
Foot Massage Roller for Plantar Fasciitis (Pink)
$19.95 -
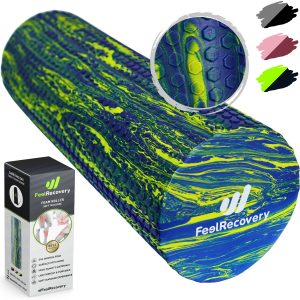
High Density Foam Roller for Muscle (Black/Gray)
$29.95 -
High Density Foam Roller for Muscle (Green/Navy)
$29.95 -
High Density Foam Roller for Muscle (Pink/Bordeaux)
$29.95 -
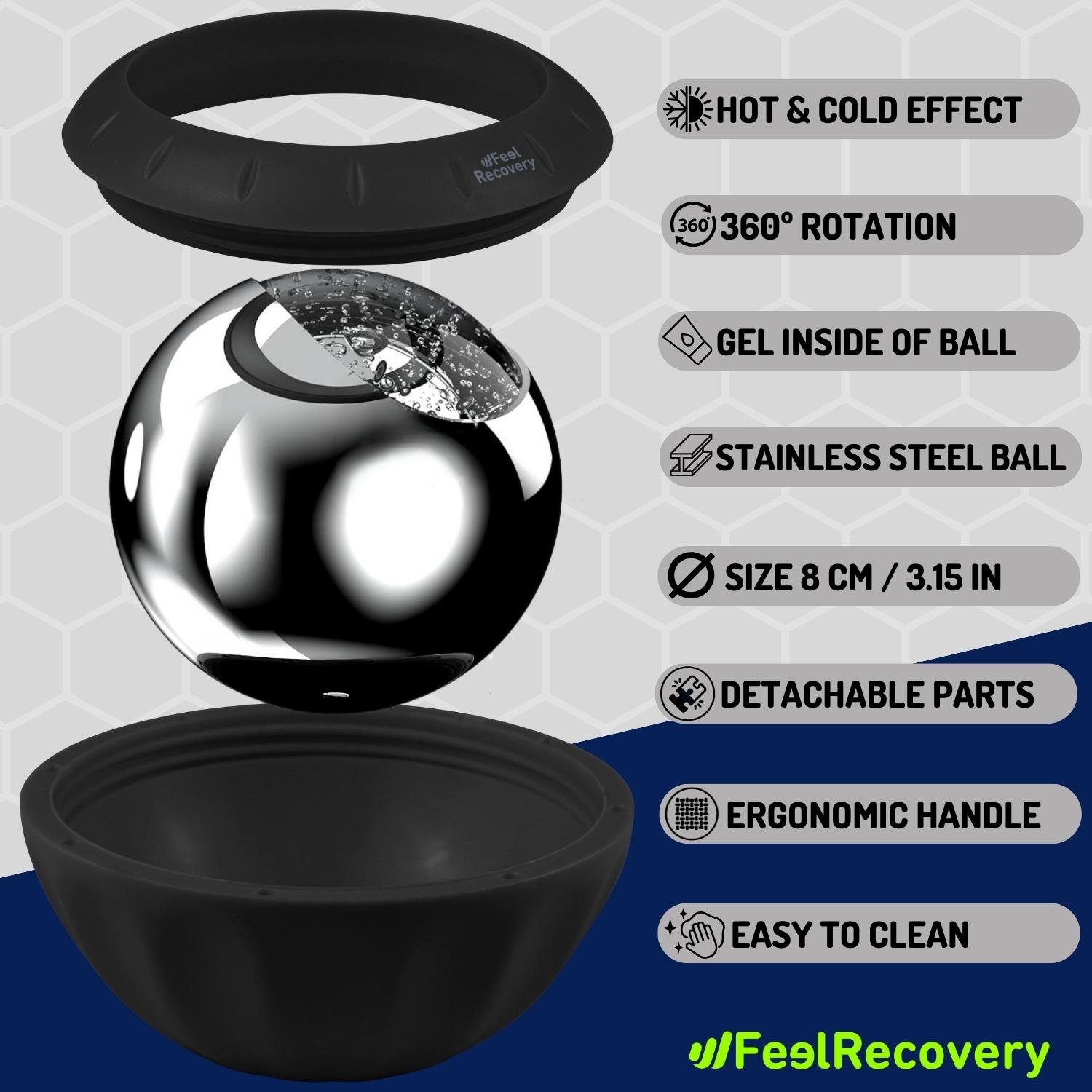
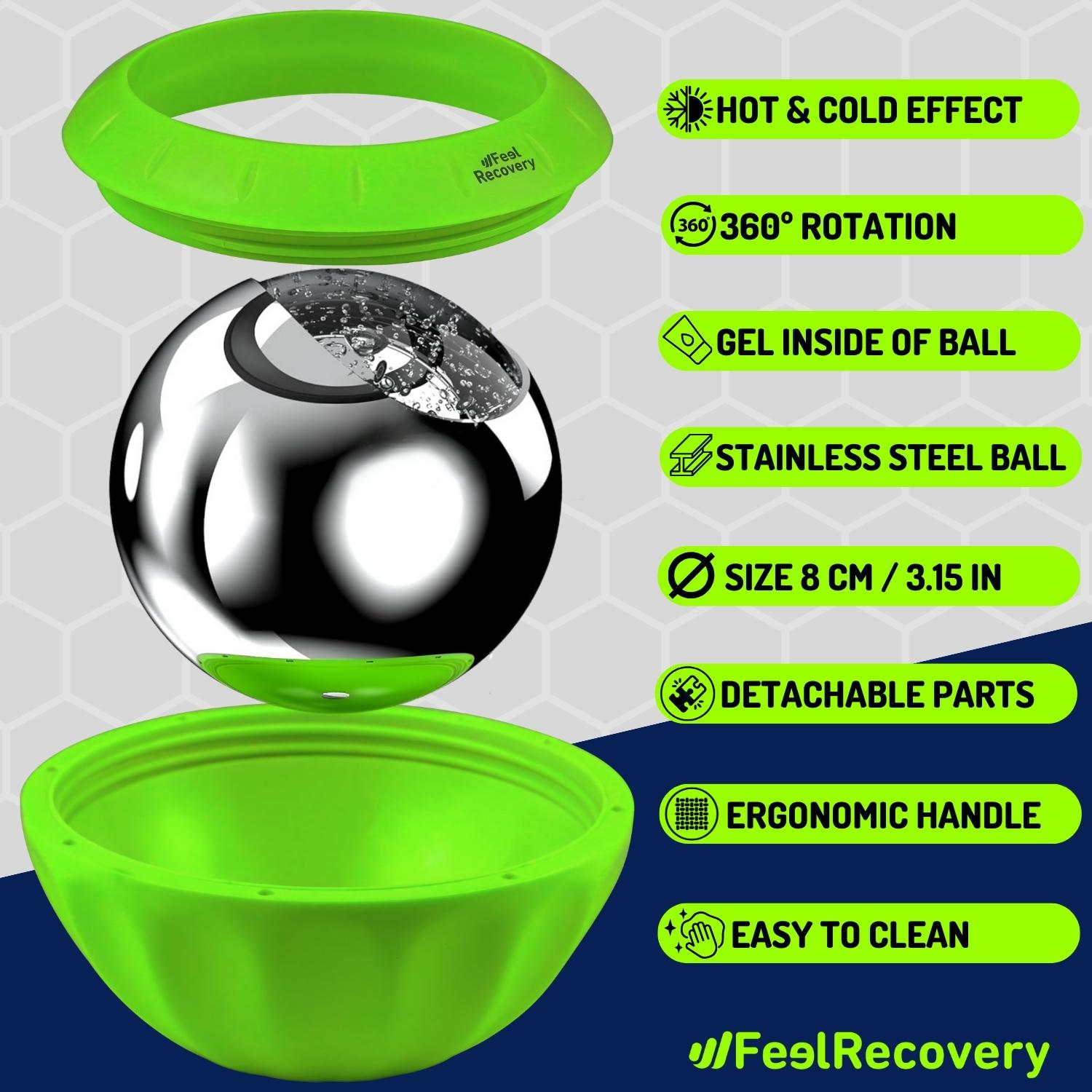
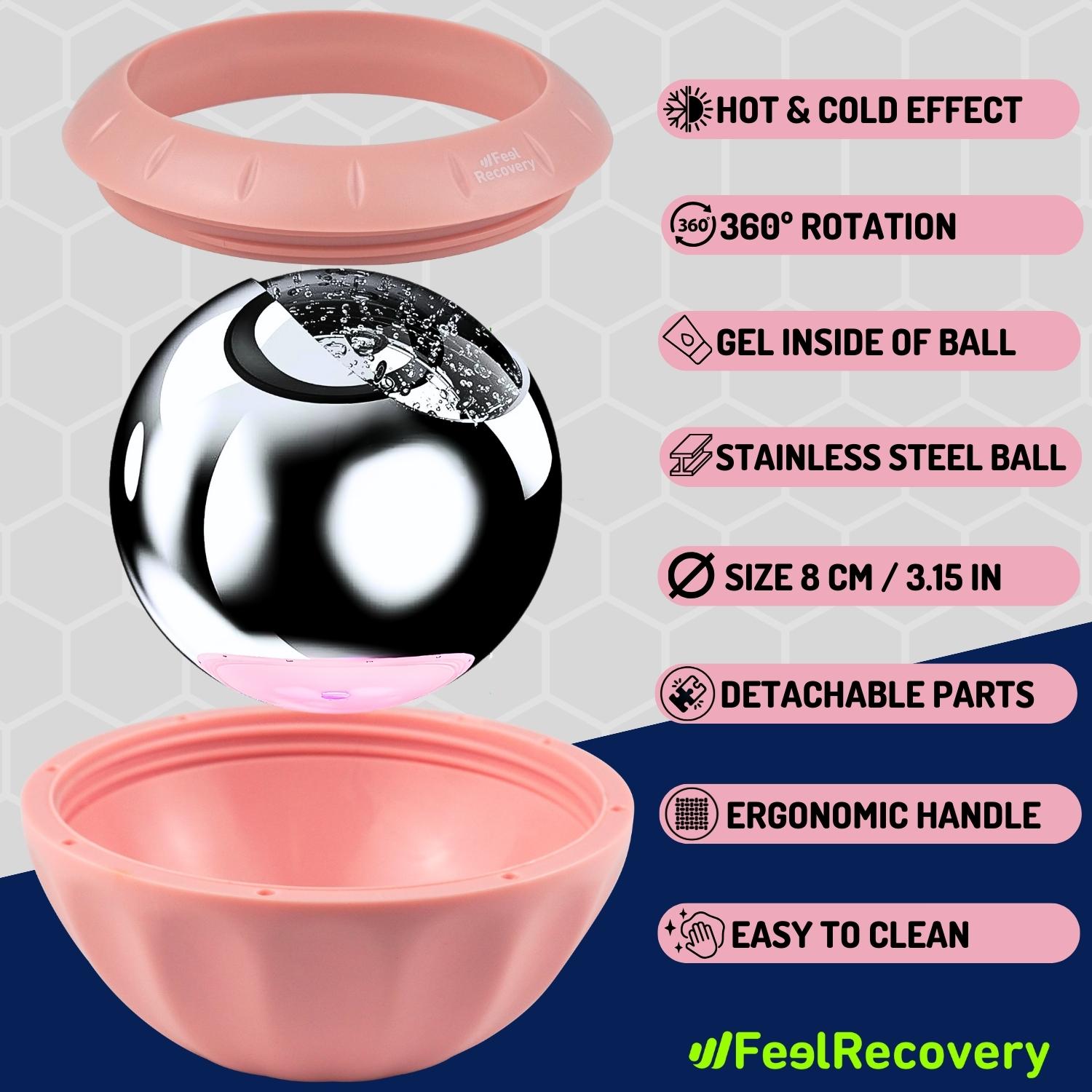
Ice Massage Roller Ball (Black)
$39.95 -
Ice Massage Roller Ball (Green)
$39.95 -
Ice Massage Roller Ball (Pink)
$39.95 -
Ice Pack for Foot - Cold Therapy Socks (Black)
$24.95 -
Ice Pack for Foot - Cold Therapy Socks (Green)
$24.95 -
Ice Pack for Foot - Cold Therapy Socks (Pink)
$24.95 -
Microwavable Heated Slippers (Hearts)
$24.95 -
Microwavable Heated Slippers (Oxford)
$24.95 -
Microwavable Heated Slippers (Sport)
$24.95 -
Microwaveable Heating Pad for Pain Relief (Hearts)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Oxford)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Sport)
$19.95 -
Pack 2 In 1 Foam Roller High + Soft Density (Black/Gray)
$29.95 -
Pack 2 In 1 Foam Roller High + Soft Density (Green/Navy)
$29.95 -
Pack 2 In 1 Foam Roller High + Soft Density (Pink/Bordeaux)
$29.95 -
Soft Density Foam Roller for Recovery (Black)
$29.95 -
Soft Density Foam Roller for Recovery (Green)
$29.95 -
Soft Density Foam Roller for Recovery (Pink)
$29.95 -
Sport Compression Socks (1 Pair) (Black/Gray)
$19.95 -
Sport Compression Socks (1 Pair) (Green/Navy)
$19.95 -
Sport Compression Socks (1 Pair) (Pink/Bordeaux)
$19.95
Main symptoms that warns us that we have inflammation of the fascia of the foot
Various health problems can arise in the foot area, such as retrocalcaneal bursitis or bone spurs, among others. Knowing the symptomatology of plantar fasciitis helps to rule out and provide the correct medical treatment.
For the patient, these signs are a wake-up call to seek specialised help:
- Heel pain: Because of the swelling, the nerves are disturbed and severe to moderate pain occurs, which is reflected right in the heel. Sometimes it spreads to the entire inner edge and arch of the feet.
- Increased sensitivity: Tingling and a burning sensation may be felt on the sole of the foot. In addition, the area will be much more sensitive to touch on palpation. This increased sensation is due to micro-injuries to nerves and tissues in the area.
- Inflammation: When dense connective tissue becomes inflamed internally, there is an increase in external volume. For this reason, the entire sole of the foot may become externally swollen.
- Increased temperature: The entire sole of the foot is likely to feel a rise in temperature. This is a direct consequence of the swelling where the blood supply is incorrect.
- Difficulty supporting the foot: This is one of the most common and recurrent symptoms suffered by patients. As the sole of the foot is swollen, it is possible that the pain does not allow correct support.
What treatments are available to relieve pain and cure plantar fasciitis?
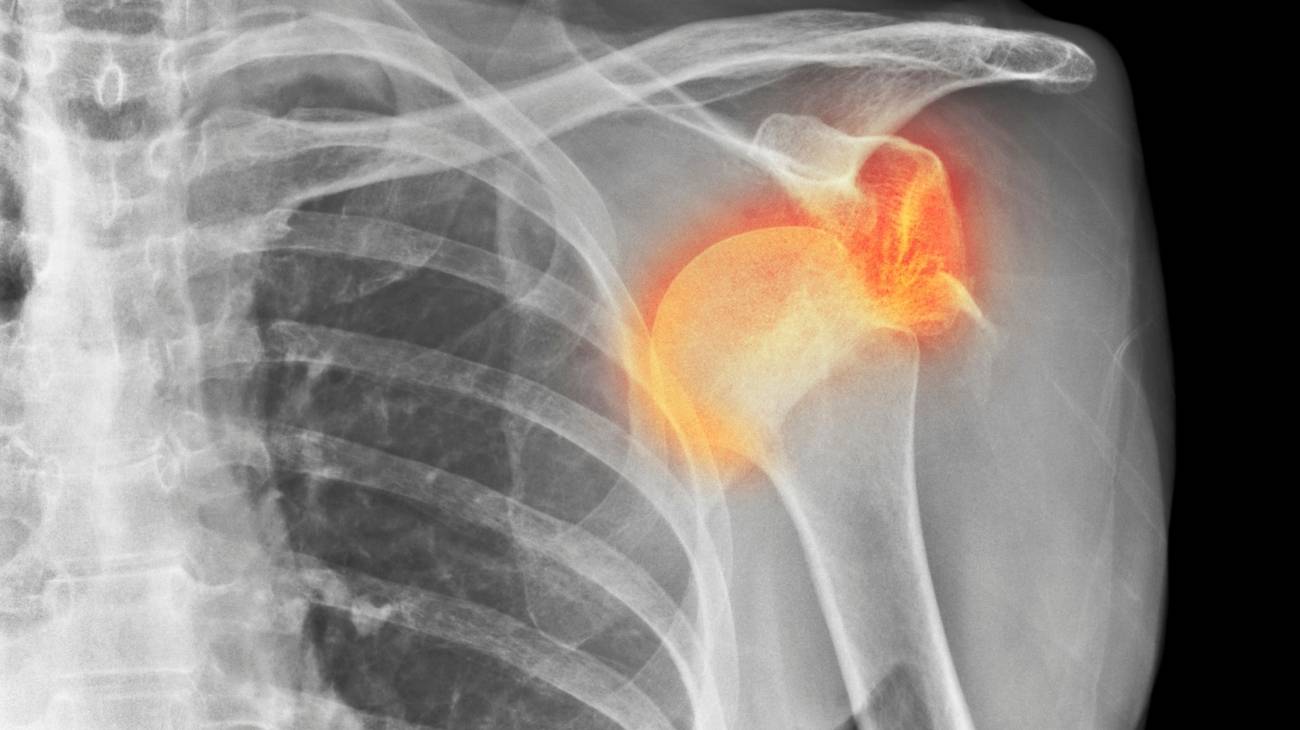
As the main means of diagnosis, doctors use physical examination and X-rays. If the diagnosis of plantar fasciitis has been successful, it is likely that one of the following treatments will be recommended.
Alternative and complementary therapies
In this type of treatment, the aim is to improve symptoms by means of different techniques. See below what they are all about:
- Hot and cold therapy: Using alternating hot and cold therapy has shown promising results in reducing inflammatory signs. This technique involves immersing the affected foot(s) in cold water for a short period of time. The same process is then carried out with warm or hot (not extreme) water. Physiotherapists advise that this time should not exceed 15 minutes. In addition, both temperatures should be kept under control so that they do not cause lacerations and produce the desired effect on the fascia. All sessions should begin and end with heat.
- Compression therapy: By using compression garments, bandages or compression braces over the entire area, the blood supply is improved. This allows the swelling to be reduced, offering relief to the patient, and even reduces pressure on the plantar arches. Although this supportive therapy is effective at the beginning of treatment, it is not advisable to prolong it too long. The use of splints during the night has been shown to have positive effects on waking up, as the compression it exerts means that the internal swelling is not excessive and prevents mobility the following day.
- Massage therapy: There are various self-massages recommended by physiotherapists. For example, there is one that is applied from a comfortable position using the knuckles, which are brought slowly from the heel to where the toes start. Specialists recommend doing this every 5 days for 3 to 5 minutes. It is also possible to place the fingertips in the centre to make deep, pulling movements on each side of the sole of the foot. It is also valid to use a rotating cylindrical implement to massage the affected area. It is not necessary to use oils or creams in these self-massages, although it is always a good idea to consult a specialist first.
- Acupressure therapy: Based on the trigger or pressure points of acupuncture it is possible to achieve an analgesic effect through massage. Acupressure is applied by therapists with the fingertips and light to moderate pressure. The arch and heel area is massaged to "numb" the nerve response to pain. It is less invasive than acupuncture, but should still be discussed with your doctor before starting this type of treatment.
- Thermotherapy: The use of heat as a therapeutic and regenerative means is also valid for plantar fasciitis. It all depends on the state of inflammation and medical recommendations. Thermotherapy includes different practices from warm water bags, footbaths and even the use of heating pads. This treatment stimulates the capillary walls for better blood flow.
- Naturalremedies using plants: Topically, many patients have seen improvements by reducing the signs of inflammation with certain plants. For example, turmeric, ginger and cayenne pepper are often used in this treatment, but this requires consultation with the acting physician for final approval. Aloe vera gel applied to the external area without lacerations is also beneficial.
- Healthy lifestyle habits: The physician will advise balanced standing until improvement is noted. For example, exercise routines should be much more moderate or the patient may be referred to a nutritionist to lose body weight along with exercise. A balanced diet and a healthy lifestyle will improve the condition. In addition, the podiatrist is likely to recommend the use of ergonomic shoe inserts. All these aspects are addressed in this re-education therapy.
Nutritional supplements
The nutrients that are used in syrups, liquids, powders or tablets as food supplements are:
- Omega 3: Certain nutritional supplements contain fatty acids that help to reduce inflammation, although the body does not produce it, it is possible to incorporate it through the diet. Omega 3 is found in fish, nuts and other foods.
- Vitamin B complex: This set of 8 vitamins is used to provide a natural analgesic effect. It includes cobalamin, thiamin, riboflavin, niacin, pantothenic acid and pyroxena, among others. They are very useful, with proven results, in combating pain associated with fascia injury.
- Calcium and magnesium: Calcium is usually obtained from dairy foods, certain vegetables and fish. However, in certain individuals, calcium supplements provide the amount that is not naturally absorbed by the body. It is often combined with magnesium (another element required by the body). These elements can possibly prevent the development of heel spurs. Also, it is important to note that these substances may interact with your medication.
Physiotherapy treatments
The most commonly used rehabilitation therapies for this type of ailment are:
- Stretching and strengthening exercises: Various sets of tissues need to regain lost elasticity and strength after plantar fasciitis. With repetitive stretching, the muscles gradually regain their strength, while toning and stretching exercises cause eccentric isometry.
- Myofascial release: Also called myofascial trigger point therapy. It focuses on maintaining or returning the fascia to an optimal state by means of certain pressures or movements, usually applied to the whole body to release tensions in the fascia and thus restore the patient's mobility.
- Ultrasound: Ultrasound is one of the most widely used physiotherapeutic means of healing connective tissue using sound energy. These mechanical vibrations are transmitted out of the body by various devices. Today's therapists tend to prefer pulsed energy equipment.
- Extracorporeal shock wave therapy: Also known by its acronym ESWT, this is a non-invasive therapeutic treatment widely used for plantar fasciitis. Its advantage over other treatments is that it does not require immobilisation or alteration of the patient's habits.
- PEM: Percutaneous microelectrolysis (PEM) uses galvanic current to produce a regulated inflammatory response. Contradictory as it may sound, the stimulation triggers a natural recovery response. The vasodilatory effects are momentary, as they subside after a week.
- High-power laser therapy: High-intensity laser therapy acts on cell membranes using biostimulation by means of a high-power laser that achieves greater penetration into the tissues. This is the only way to obtain a more effective response according to the opinion of many specialists.
- Hydrotherapy: This is a very broad form of therapy that encompasses different uses of water. It acts as a restorative, therapeutic agent and above all to restore mobility. It is also applied to achieve relief, improve balance, reduce swelling, among others. Among the methods most recommended by therapists for this condition is the therapeutic tank, although whirlpool baths are another alternative.
- Contact hyperthermia or tecartherapy: This method uses radio waves as a means of electrotherapy to regenerate the affected tissues. These long-range waves are sent into the body through external accessories. In this technique there is a resistive and a capacitive modality depending on the case. It is usually called TECAR.
- Mechanotherapy: This treatment makes use of toning and stretching exercises in combination with other methods. For example, proprioception exercise, balance restoration and correct gait training are some of the techniques used in this therapy.
Medications
Pharmacological therapy uses the following medications to treat the injury to the fascia:
- NSAIDs: Non-steroidal anti-inflammatory drugs are part of the conservative treatment for plantar fasciitis. Depending on the case, only Ibuprofen, Diclofenac (potassium or sodium) and Ketoprofen may be prescribed by the doctor. These have not only anti-inflammatory but also analgesic effects.
- Local steroid injections: Cortisone has a strong anti-inflammatory property. Based on this, it is often recommended by doctors and placed in cases of fascial inflammation, which reduces the swelling of the surrounding ligaments and brings relief. They are left for very specific cases where the next step, if they do not work, is surgery.
- PRP: Platelet-rich plasma, or PRP, is a very useful preventive regeneration methodology with favourable results in associated disorders such as heel spurs and tendonitis.
- Botulinum toxin type A: This is applied by infiltration to ensure greater precision. This substance allows the release of acetylcholine and neurotransmitters to be inhibited to reduce muscle contractions. It has relaxing, therapeutic and analgesic effects by relieving painful spasms.
It should be kept in mind that drug therapy should be guided and advised by the physician. Self-medication is not recommended because it could cause irreparable damage.
Surgery
Only in certain chronic cases where conservative treatment is insufficient is it possible to apply this technique. Under local anaesthesia, an incision is made to cut the plantar fascia, although some post-surgical pain may occur after the operation. Even so, it is appropriate in certain cases to allow stretching and restore mobility. Another side effect may be the development of flat feet.
What are the most effective prevention methods for plantar fasciitis?
Although most individuals will suffer from plantar fasciitis at some point in their lives, it is possible to prevent it.
- Use appropriate footwear: All footwear should be ergonomic and appropriate to the anatomy of the foot, without being too tight or loose. So the person should feel comfortable.
- Stretching and warming up: Before carrying out any exercise it is important to perform comprehensive stretches. This type of activity should last at least 15 to 20 minutes to adapt the tissues to the action to be performed.
- Maintain balance in body positions: To maintain a healthy muscular posture is necessary to avoid plantar fasciitis; in addition, it is advisable to alternate positions. The body needs to move, but it also needs to rest (when sitting, lying down or standing still), so that the biomechanical systems are not strained.
- Eating a balanced diet: Along with exercise, eating a balanced diet helps to avoid obesity. It is possible to integrate certain foods rich in calcium, vitamin D, proteins and mineral salts. With the help of a nutritionist it is possible to lose weight, if the doctors deem it necessary.
- Regular balanced exercise: Regular exercise against sedentary lifestyles prevents overweight and keeps the entire joint system, especially the feet, in balance. This makes it less likely to suffer from plantar fasciitis.
- Avoid extreme workouts: As opposed to healthy exercise, there are certain routines or sports that place extra demands on the body because they require the foot to be placed in awkward positions. They can even lead to putting too much weight on them. Leaving these kinds of extreme activities aside decreases the likelihood of the occurrence of fascial injury.
F.A.Q: Frequently Asked Questions
Find out the most frequently asked questions about plantar fasciitis:
References
- Buchbinder, R. (2004). Plantar fasciitis. New England Journal of Medicine, 350(21), 2159-2166. https://www.nejm.org/doi/full/10.1056/nejmcp032745
- DeMaio, M., Paine, R., Mangine, R. E., & Drez, D. (1993). Plantar fasciitis. Orthopedics, 16(10), 1153-1163. https://journals.healio.com/doi/abs/10.3928/0147-7447-19931001-13
- Goff, J. D., & Crawford, R. (2011). Diagnosis and treatment of plantar fasciitis. American family physician, 84(6), 676-682. https://www.aafp.org/pubs/afp/issues/2011/0915/p676.html
- Schepsis, A. A., Leach, R. E., & GOUYCA, J. (1991). Plantar fasciitis: etiology, treatment, surgical results, and review of the literature. Clinical Orthopaedics and Related Research (1976-2007), 266, 185-196. https://journals.lww.com/corr/Abstract/1991/05000/Plantar_Fasciitis__Etiology,_Treatment,_Surgical.29.aspx
- Riddle, D. L., Pulisic, M., Pidcoe, P., & Johnson, R. E. (2003). Risk factors for plantar fasciitis: a matched case-control study. JBJS, 85(5), 872-877. https://journals.lww.com/jbjsjournal/Abstract/2003/05000/Risk_Factors_for_Plantar_Fasciitis__A_Matched.15.aspx
- Lynch, D. M., Goforth, W. P., Martin, J. E., Odom, R. D., Preece, C. K., & Kotter, M. W. (1998). Conservative treatment of plantar fasciitis. A prospective study. Journal of the American Podiatric Medical Association, 88(8), 375-380. https://japmaonline.org/view/journals/apms/88/8/87507315-88-8-375.xml
- Crosby, W., & Humble, R. N. (2001). Rehabilitation of plantar fasciitis. Clinics in podiatric medicine and surgery, 18(2), 225-231. https://europepmc.org/article/med/11417152
- Snider, M. P., Clancy, W. G., & McBeath, A. A. (1983). Plantar fascia release for chronic plantar fasciitis in runners. The American journal of sports medicine, 11(4), 215-219. https://journals.sagepub.com/doi/abs/10.1177/036354658301100406
- Digiovanni, B. F., Nawoczenski, D. A., Malay, D. P., Graci, P. A., Williams, T. T., Wilding, G. E., & Baumhauer, J. F. (2006). Plantar fascia-specific stretching exercise improves outcomes in patients with chronic plantar fasciitis: a prospective clinical trial with two-year follow-up. JBJS, 88(8), 1775-1781. https://journals.lww.com/jbjsjournal/Abstract/2006/08000/Plantar_Fascia_Specific_Stretching_Exercise.13.aspx
- DiGiovanni, B. F., Nawoczenski, D. A., Lintal, M. E., Moore, E. A., Murray, J. C., Wilding, G. E., & Baumhauer, J. F. (2003). Tissue-specific plantar fascia-stretching exercise enhances outcomes in patients with chronic heel pain: a prospective, randomized study. JBJS, 85(7), 1270-1277. https://journals.lww.com/jbjsjournal/Abstract/2003/07000/Tissue_Specific_Plantar_Fascia_Stretching_Exercise.13.aspx