If you play tennis, you've probably ever had shoulder pain or discomfort. This racket sport pushes the capacity of this joint to the limit. As a consequence, sports injuries to the shoulder are generated in tennis, and today we'll talk to you about them.
Yes, in tennis, injuries can occur to different components of the shoulder such as the labrum and the rotator cuff. If you want to know which are the most common shoulder pathologies in tennis players and why they arise, read on and you will know everything about them. Let's go!
What are the most common types of shoulder injuries when we play tennis?
The movements of the shoulder exercised in tennis during the service, require the application of enough power. The repeated performance of these movements over the head can overload the shoulder and injure it as a result. There are several shoulder injuries suffered by tennis players, notably SLAP pathologies and those affecting the rotator cuff.
Here is a selection of the most common injuries in this racket sport:
SLAP injuries (upper labrum from anterior to posterior)
SLAP injuries consist of a fraying or tearing of the upper part of the labrum, just where the biceps tendon is inserted. The labrum is a ring of cartilage located in the glenoid cavity, into which the head of the humerus fits. There are several types of SLAP lesions, the most common involving the detachment of the upper labrum and biceps tendon from the glenoid. They produce shoulder pain (usually associated with movements above the head) as well as weakness, decreased mobility and clicking in the same area.
They are generated by repetitive movements of the shoulder or due to a trauma such as a fall. According to biomechanical studies of athletes, the late cocking stage during throws and serves (over the head) is fundamental in the aetiology of SLAP injuries. These pathologies are often associated with scapular dyskinesia and glenohumeral internal rotation deficit (GIRD).
Subacromial bursitis
It consists of the inflammation of the subacromial bursa. This is a small fluid-filled sac located in the shoulder just below the acromion, which helps to decrease friction in this joint. It can be caused by overuse, injury or some pre-existing condition such as rheumatoid arthritis. Athletes like tennis players are prone to it.
This injury causes pain on the outside or tip of the shoulder that can be worse when lifting the arm. Reduced mobility, swelling and redness can also occur. It is common for this pathology to be accompanied by tendonitis in the adjacent tendons.
Rotator cuff tendinitis
It consists of inflammation of the rotator cuff tendons. The latter is a group of 4 muscles and 4 tendons located in the shoulder, which provide stability and mobility. Usually, this tendinitis first affects the supraspinatus tendon of the rotator cuff and ends up gradually damaging the other three.
It is usually caused by repetitive movements of the shoulder such as raising the arm above the head. This movement occurs frequently in tennis practice and other disciplines. Initially the symptoms are: local inflammation and dull pain at the outer tip of the shoulder that worsens with certain movements (pushing, pulling, raising the arm). Later the pain may increase and spread to the shoulder.
Tear of the rotator cuff
It occurs when one or more of the rotator cuff tendons tear, i.e., rupture. They may be partially or completely torn depending on the severity of the injury. As a result, the adhesion of the affected tendons to the head of the humerus is either damaged or eliminated.
This injury can be of traumatic aetiology (fall on extended arm, heavy lifting) or degenerative. Degenerative tears are the most frequent and can develop from repetitive shoulder movements like those in tennis. The symptoms associated with this disease are: pain (at rest, when lifting and lowering the arm), weakness and crackling. When the cause is traumatic the pain is usually more intense.
Dislocated shoulder
Also known as shoulder dislocation, this injury occurs when the head of the humerus partially or completely slips out of the glenoid socket of the shoulder blade. The shoulder is the joint with the greatest range of motion in the human body, which is why it is also the most dislocated. In most cases this dislocation occurs forward, although it can also happen backwards or downwards.
This injury can be generated by a strong blow on the shoulder or by falling on the arm. Also, it can occur due to a forced movement or rotation of this joint. In general, this injury produces visible deformity in the shoulder, loss of mobility, intense pain, swelling and bruising. It can also lead to damage to the muscles, tendons, blood vessels, nerves and others located in the area.
Shoulder micro-instability
Shoulder micro-instability consists of an anatomical alteration of this joint. It causes the head of the humerus to move abnormally and to shift partially from its natural position. Those who suffer from it feel pain and functional limitation in the area, this is often manifested as a feeling of "dead" or weakened shoulder. It is associated with other pathologies such as SLAP injuries.
It arises from accumulated micro-traumatisms that affect the static stabilisers of the shoulder. Repetitive movements over the head and involving external rotation or abduction are associated risk factors. Therefore, it is common in athletes such as tennis players.
Best products for recovery from tennis shoulder injuries
Bestseller
-
Acupressure Mat and Pillow (Black/Gray)
$49.95 -
Acupressure Mat and Pillow (Green/Navy)
$49.95 -
Acupressure Mat and Pillow (Pink/Bordeaux)
$49.95 -
Acupressure Pillow (Black/Gray)
$29.46 -
Acupressure Pillow (Green/Navy)
$29.46 -
Acupressure Pillow (Pink/Bordeaux)
$29.46 -
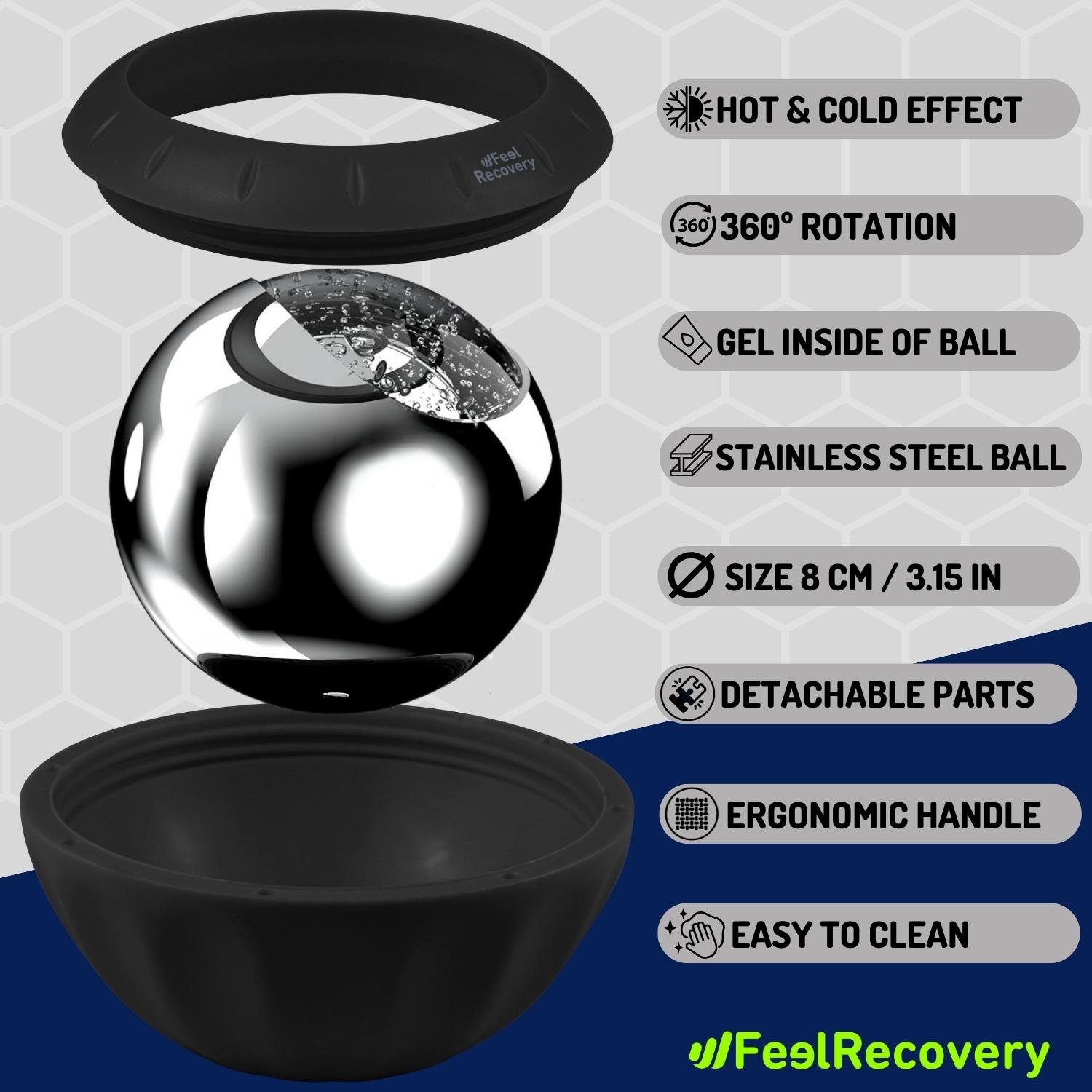
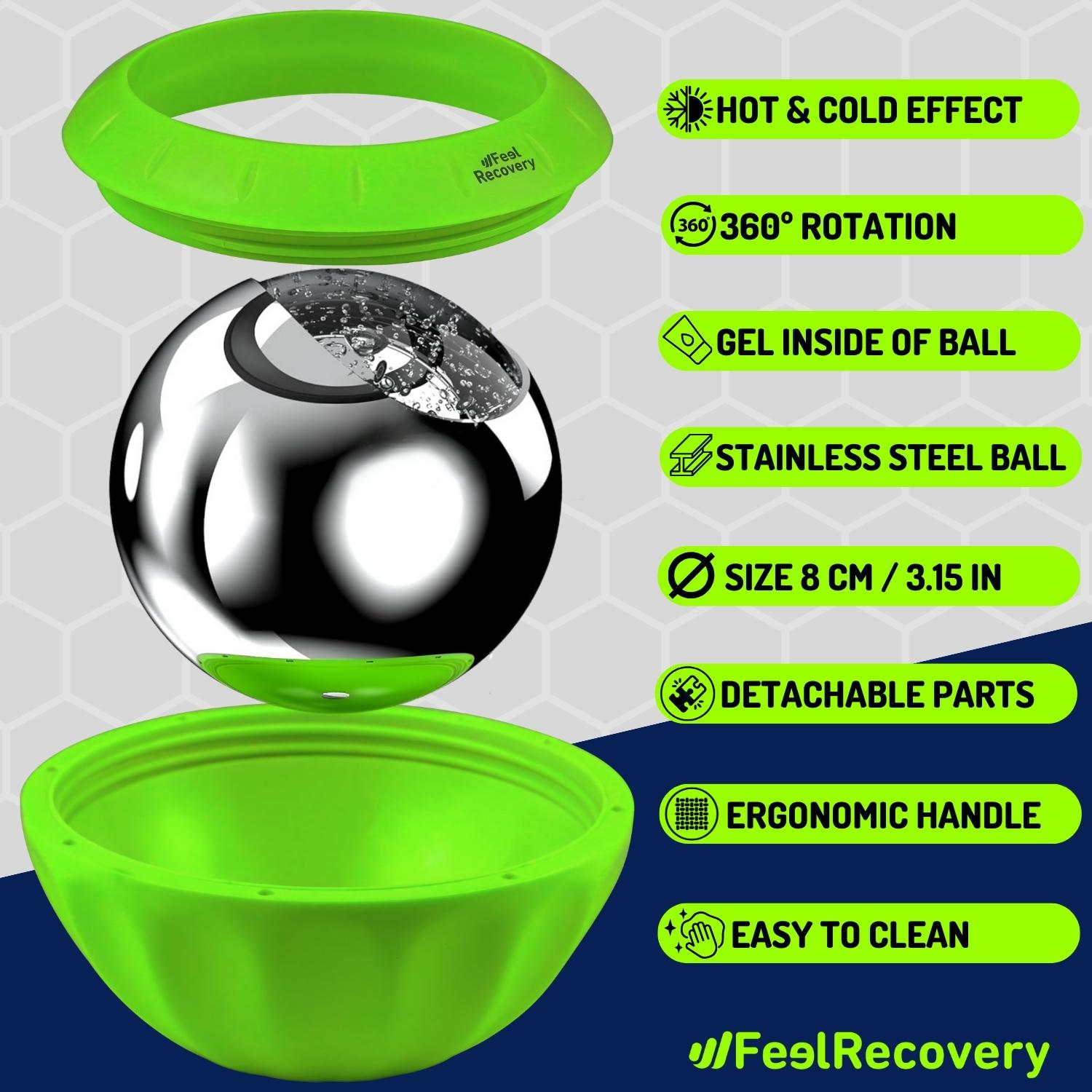
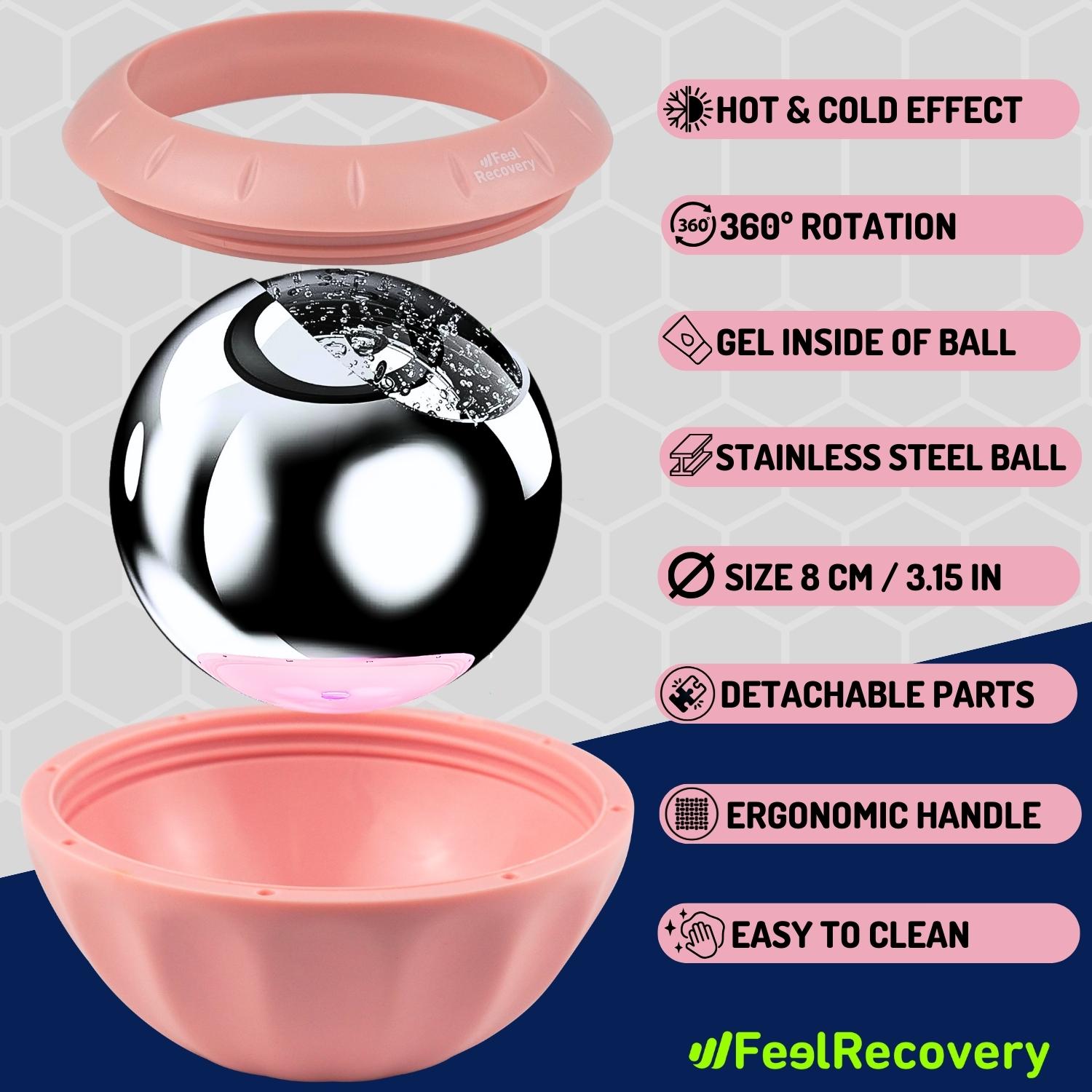
Ice Massage Roller Ball (Black)
$39.95 -
Ice Massage Roller Ball (Green)
$39.95 -
Ice Massage Roller Ball (Pink)
$39.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Hearts)
$24.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Oxford)
$24.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Sport)
$24.95 -
Microwave Heating Pad for Neck Pain Relief (Hearts)
$19.95 -
Microwave Heating Pad for Neck Pain Relief (Oxford)
$19.95 -
Microwave Heating Pad for Neck Pain Relief (Sport)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Hearts)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Oxford)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Sport)
$19.95 -
Shoulder Support Brace (Black)
$24.95 -
Shoulder Support Brace (Green)
$24.95 -
Shoulder Support Brace (Pink)
$24.95 -
Trigger Point Massage Stick (Black)
$14.95 -
Trigger Point Massage Stick (Green)
$14.95 -
Trigger Point Massage Stick (Pink)
$14.95
How to apply RICE therapy to treat shoulder injuries in tennis players?
RICE is a medical care protocol applied to treat injuries. Its name comes from the union of the initials rest, ice, compression and elevation. These four words represent the steps or stages in the application of RICE therapy. There are other similar methodologies, such as the PRICE protocol. This is actually an update of RICE, which introduces a new step: protection.
Below, we explain what each step of PRICE therapy consists of:
- Protection: This is the first step and consists of protecting the member or area affected. To do this, it is necessary to suspend sporting activity and avoid any movement that might aggravate the injury. In this step, it is advisable to use an immobiliser such as slings, joint supports, etc.
- Rest: Subsequently, it is essential to provide rest to the affected area. However, usually this should not be completely immobilized or stiffness could be generated. In general, a rest period of 48 hours is recommended, which includes safe movements for the patient.
- Ice: This step aims to reduce pain and inflammation with the application of cryotherapy on the injury. You should only place a cold compress (with between 10 and 20 °C) on the affected area for about 20 minutes maximum (exceeding this time is dangerous). You can apply the compress 6 to 8 times a day.
- Compression: By properly compressing the injury we promote blood circulation, reducing inflammation, and in turn firming up the affected area. In this step it is possible to bandage the injury with a tissue, this usually must be elastic to allow safe movements. The bandage must be adjusted but must allow circulation.
- Elevation: Elevation of the affected area has anti-inflammatory properties and helps to reduce pain. Basically, at this stage you should support the affected area on an elevated surface, preferably padded. This, seeking that the injury is at a level above the heart. Rest periods are ideal for this step.
References
- Van der Hoeven, H., & Kibler, W. B. (2006). Shoulder injuries in tennis players. British journal of sports medicine, 40(5), 435-440. https://bjsm.bmj.com/content/40/5/435.abstract
- Ellenbecker, T. S. (1995). Rehabilitation of shoulder and elbow injuries in tennis players. Clinics in sports medicine, 14(1), 87-110. https://www.sciencedirect.com/science/article/abs/pii/S027859192030260X
- McCann, P. D., & Bigliani, L. U. (1994). Shoulder pain in tennis players. Sports Medicine, 17, 53-64. https://link.springer.com/article/10.2165/00007256-199417010-00005
- Kibler, W. B. (1995). Biomechanical analysis of the shoulder during tennis activities. Clinics in sports medicine, 14(1), 79-85. https://www.sciencedirect.com/science/article/abs/pii/S0278591920302593
- Chandler, T. J., Kibler, W. B., Stracener, E. C., Ziegler, A. K., & Pace, B. (1992). Shoulder strength, power, and endurance in college tennis players. The American Journal of Sports Medicine, 20(4), 455-458. https://journals.sagepub.com/doi/abs/10.1177/036354659202000416
- Abrams, G. D., Renstrom, P. A., & Safran, M. R. (2012). Epidemiology of musculoskeletal injury in the tennis player. British journal of sports medicine, 46(7), 492-498. https://bjsm.bmj.com/content/46/7/492.short
- Chandler, T. J. (1995). Exercise training for tennis. Clinics in sports medicine, 14(1), 33-46. https://europepmc.org/article/med/7712556
- Nirschl, R. P. (1988). Prevention and treatment of elbow and shoulder injuries in the tennis player. Clinics in Sports Medicine, 7(2), 289-308. https://www.sciencedirect.com/science/article/abs/pii/S0278591920309364
- Eygendaal, D., Rahussen, F. T. G., & Diercks, R. L. (2007). Biomechanics of the elbow joint in tennis players and relation to pathology. British journal of sports medicine, 41(11), 820-823. https://bjsm.bmj.com/content/41/11/820.short
- Perkins, R. H., & Davis, D. (2006). Musculoskeletal injuries in tennis. Physical Medicine and Rehabilitation Clinics, 17(3), 609-631. https://www.pmr.theclinics.com/article/S1047-9651(06)00031-3/fulltext