- What is rotator cuff tendinitis?
- What are the causes and risk factors for rotator cuff tendinitis?
- Best products for rotator cuff tendonitis
- Main symptoms that warn us of rotator cuff tendinitis
- What treatments are available to improve and cure shoulder tendonitis?
- Prevention for shoulder tendon inflammation
Keep in mind that tendonitis in the shoulder, and more specifically in the rotator cuff tendon, will cause you to be unable to move your arm and even feel pain in your neck. In addition, the joint is likely to become inflamed and nodules may develop as a result of this condition. It is therefore a good idea to find out what tendinopathy is and what causes it.
This information, explained in a simple way, can be read in the following paragraphs. We will talk about the symptoms that will help you to notice the presence of this injury and which are the treatments and methods to prevent it. Take a look.
What is rotator cuff tendinitis?
The scapulohumeral and acromioclavicular joints are made up of muscles, tendons and bones that contribute to the movement of the shoulder, known as the rotator cuff. Although it is able to withstand continuous strain and sliding, it can also become irritated due to overexertion or catching cold, among other causes.
Regardless of the reason,when the tendons of the infraspinatus, supraspinatus, subscapularis or teres minor muscles become inflamed, then rotator cuff tendinitis arises. It is a particularly painful, debilitating and disabling condition for the patient.
What are the causes and risk factors for rotator cuff tendinitis?
There are different factors that put the onset of rotator cuff tendinitis at risk. See below for the most common ones:
- Over-strain: Certain positions that are held for too long put too much strain on the shoulder, causing the tendons to overwork. For example, when you tend to sleep or always lean your body on your side or when using a computer without resting your arms.
- Repetitive movements: Repeated use of the shoulder joints also causes overload. Keep in mind that the tendon cords are designed to withstand a certain amount of pressure, and by not allowing the tissue to recover, the tendons become irritated and inflamed.
- Impingement syndrome: Also called bottleneck syndrome or subacromial syndrome. It is a small space that develops between the tendons and the acromion, causing inflammation. Whether due to bursitis, postural changes or bone spurs (e.g. in the acromion) such a syndrome is a direct trigger for tendonitis.
- Injuries, traumas, fractures: The body tends to react to blows, falls and any other impact on tissues or bones. The risk of inflammation is further increased if the area has been previously injured or lacerated. Changes due to trauma to bone structures or fractures also affect this joint causing tendonitis.
- Calcified shoulders: In this condition the tendons begin to accumulate calcium deposits, so inflammation is imminent. In fact, it is known as calcifying tendonitis of the shoulder. It usually affects women in their 50s and 60s.
- Frozen or stiff shoulder syndrome: Also called adhesive capsulitis, this occurs when the connective tissue capsule thickens. As a result, the shoulder joints tighten and gradually lose movement.
- Intense sports activities: Athletes tend to suffer from tendinopathies at shoulder level, as they push the muscles and tendons to the extreme. Those who follow an exercise routine (e.g. to strengthen the back) that is too strenuous are also at risk.
- Manual occupations: Similarly, people in manual occupations that are demanding on the shoulders can develop tendinitis. Over-stimulation from long working hours can easily lead to a collapse of the tendons.
- Cold temperatures: Staying in cold places for long periods of time can lead to numbness in the shoulder joint, which - in the event of a sudden movement - can lead to rotator cuff tendinitis.
Best products for rotator cuff tendonitis
Bestseller
-
Acupressure Mat and Pillow (Black/Gray)
$49.95 -
Acupressure Mat and Pillow (Green/Navy)
$49.95 -
Acupressure Mat and Pillow (Pink/Bordeaux)
$49.95 -
Acupressure Pillow (Black/Gray)
$29.46 -
Acupressure Pillow (Green/Navy)
$29.46 -
Acupressure Pillow (Pink/Bordeaux)
$29.46 -
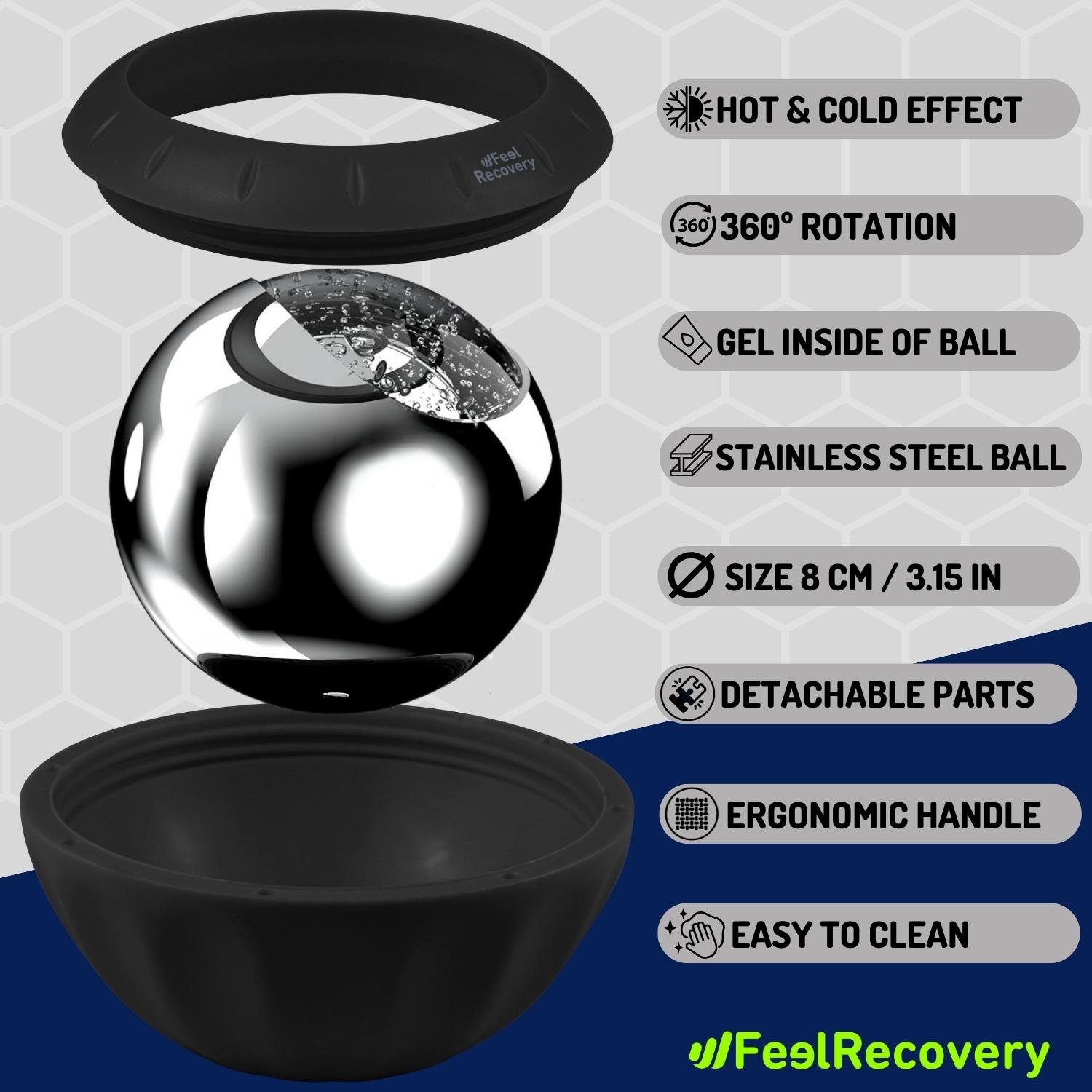
Ice Massage Roller Ball (Black)
$39.95 -
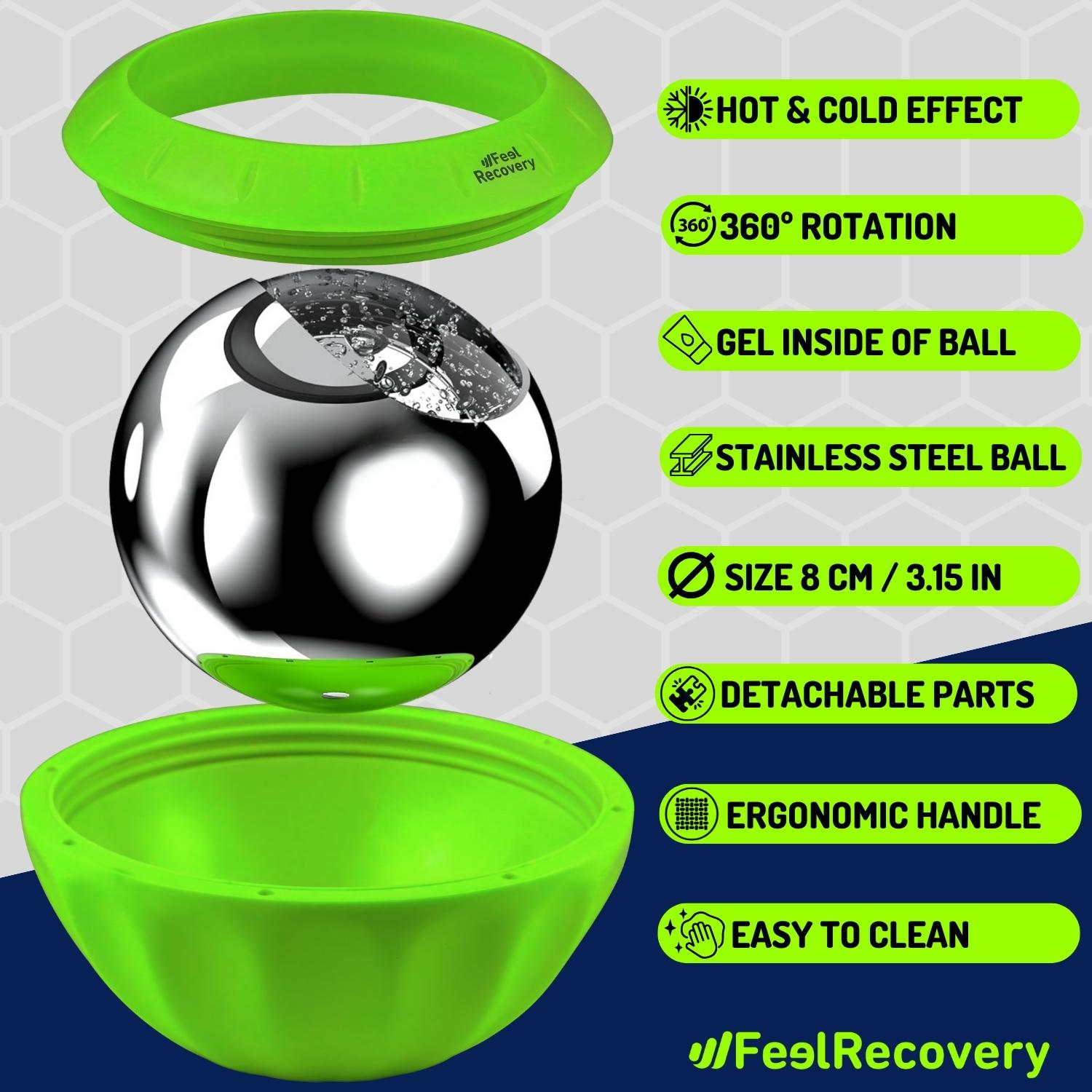
Ice Massage Roller Ball (Green)
$39.95 -
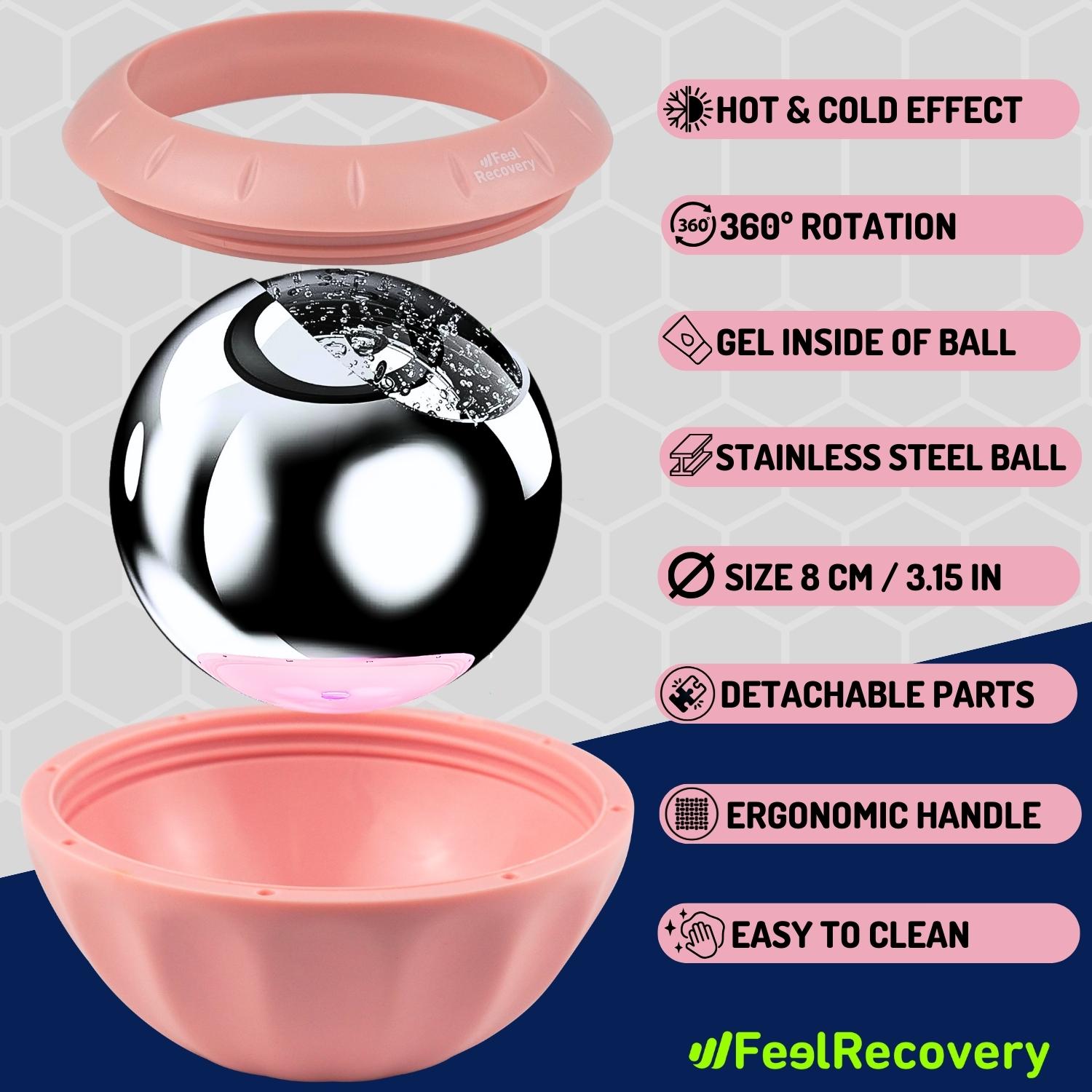
Ice Massage Roller Ball (Pink)
$39.95 -
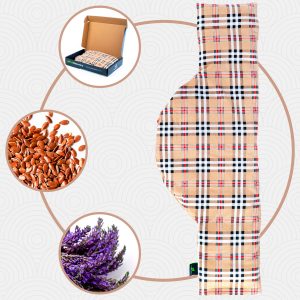
Microwave Heating Pad for Neck & Shoulder Pain Relief (Hearts)
$24.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Oxford)
$24.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Sport)
$24.95 -
Microwave Heating Pad for Neck Pain Relief (Hearts)
$19.95 -
Microwave Heating Pad for Neck Pain Relief (Oxford)
$19.95 -
Microwave Heating Pad for Neck Pain Relief (Sport)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Hearts)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Oxford)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Sport)
$19.95 -
Shoulder Support Brace (Black)
$24.95 -
Shoulder Support Brace (Green)
$24.95 -
Shoulder Support Brace (Pink)
$24.95 -
Trigger Point Massage Stick (Black)
$14.95 -
Trigger Point Massage Stick (Green)
$14.95 -
Trigger Point Massage Stick (Pink)
$14.95
Main symptoms that warn us of rotator cuff tendinitis
Learn the main signs that will help you to notice the presence of inflammation in the tendons of the shoulder:
- Pain: People with rotator cuff tendinitis feel a sharp, pulling pain that causes muscle weakness in the area. Such pain can spread from the upper edge of the shoulder to the neck.
- Inflammation: Another factor in the symptomatology is swelling, which will start to become visible externally. In these conditions, not only the tendons become irritated, but the bursae surrounding the tendons tend to become inflamed as well. As a result, the shoulder will feel enlarged and abnormal to the touch.
- Redness: It is common for the skin to appear reddened externally due to the inflammatory disturbance. This happens because of increased blood flow to the area and significant structural changes in the tissue.
- Poor mobility: Because of the excessive inflammation, the shoulder joint begins to have compromised mobility. As a result, it is often difficult for the patient to perform common movements. A feeling of heaviness is also common in these cases of shoulder tendinopathy.
- Increased pain when moving: The joint area is sore, swollen and weak due to the condition. In addition, the joint space is narrowed by the swelling. Thus, so many changes cause a painful sensation in the nerves when trying to move the arm.
- Appearance of nodules: It is also common to find lumps in the affected area. This is generated by the constant tension on the tendon, causing the thickening to be visible from the surface of the skin.
What treatments are available to improve and cure shoulder tendonitis?
In order to improve the patient's condition, different lines of conservative treatment are established for the shoulder. If this does not work, more invasive means are used in an attempt to cause as little damage as possible.
Take a look at these therapies:
Alternative and complementary therapies
Take a look at the following therapies that are used in a complementary way for this type of complaint:
- Hot and cold therapy: Contrasting temperature therapy is highly valued in tendonitis, although the shoulder region is difficult to immerse, compresses or scarves can be used. Using alternating cold and heat for a short period of time shortens the recovery process due to the anti-inflammatory and analgesic effects. The temperature should range from -20° to -10°, while the heat should vary between 37° and 39°. Both applications should not exceed 20 minutes.
- Compression therapy: Using compression garments or elastic bandages, doctors apply pressure to the affected shoulder. Basically, this method tries to contain the swelling so that it does not continue to affect the tendon structures. At the same time, they provide protection against further injury and give you some gradual mobility. Bandages should still be applied by a specialist to get the correct level of compression.
- Massage therapy: There are different types of massage that promote a painless recovery process. One of them is self-massage directed at the supraspinatus, infraspinatus, teres minor and teres major. Some cause momentary pain, but then improve muscle tension. It should be noted that these deep transverse massages should be directed against the fibres.
- Acupressure therapy: In contrast to massage therapy, acupressure uses acupuncture points as a reference, as it is at these points that manual pressure is safely applied. Fingers are used to apply gentle pressure to the painful areas and a relaxed location is sought. However, if the therapy does not have the desired effect in a short time, it is advisable to discontinue its use.
- Thermotherapy: This treatment uses heat as a therapeutic medium, especially in cases where the initial trauma has subsided, but the pain continues. This is because it has a vasodilator effect that influences the metabolism and the body's defences. It is a means of analgesic and elastin generation, so it is applied with different elements such as compresses, saunas and ultrasound, among others.
- Natural remedies using plants: Plants with anti-inflammatory and sedative effects such as aloe vera, ginger, mint, sage or rosemary are beneficial for relieving the symptoms of rotator cuff tendinitis. Most are applied to the external area where there are no lacerations or open wounds, although others are taken or integrated into the diet as is the case with ginger. Although they are folk remedies they should never be taken without medical supervision.
- Healthy lifestyle habits: It is likely that the patient will need to integrate new habits into their routine following acute tendonitis. For example, altering the exercise routine to a more gentle one, practising yoga or wearing preventive bandages may help. It is also wise to watch your diet by adding fibre-rich foods, nuts, seeds, tomatoes and fish.
Nutritional supplements
It is possible to incorporate by means of syrups, pills or powders different nutrients that will help tendinitis recovery. Among the most commonly prescribed by doctors are:
- Glucosamine: This is a natural supplement especially indicated to improve the condition of tendons and joints. This allows the body to recover the protein that is naturally produced in the body and that is lost over the years.
- Chondroitin: Although more focused on the regeneration of joint cartilage, it also supports tendon health. It tends to be found in conjunction with glucosamine and other associated supplements.
- Omega 3: A dietary supplement widely used in cardiovascular health due to the great benefits it contains. This nutrient, found in fish, may be useful if tendonitis is related to arthritis or osteoarthritis as it supports bone health.
- Hyaluronic acid: HA is not only used for aesthetic purposes, as this compound is found in many tissues of the body to capture water. As this property is lost over time, many people consume it as a supplement.
- Collagen: Collagen is a substance already present in an integral form in the tissues. Even so, many people require its oral or injected consumption to reduce the symptoms of tendinitis.
- MSM: Methylsulfonylmethane is a synthesised supplement that is effective in reducing pain, although caution should be exercised as there is not yet sufficient scientific evidence to support it. For this reason, it should be prescribed by a doctor.
Physiotherapy treatments
Some treatments include:
- Rehabilitation exercises: In the middle phase of the rehabilitation process, it is necessary to adapt to strengthening exercises. These will allow the joint to regain mobility, tone and muscle strength. They are usually repetitions, strengthening exercises and pendulum exercises.
- Percutaneous Intratisular Electrolysis (PIE): This is a moderately invasive treatment where a thin (acupuncture) needle is inserted into the painful area, which is guided by ultrasound to transmit a low-frequency galvanic current into the region. Its aim is to destroy the damaged tissue and produce a natural inflammation that aims at vasodilatation. It is indicated in chronic tendinopathies where it is possible to complement other treatments under anaesthesia (e.g. infiltration).
- Radiofrequency Indiba: This treatment uses radiofrequency waves as a regenerative medium. It is a method considered safe, innocuous and effective in acute and chronic inflammatory pathologies. These currents or electrical waves stimulate the blood circulation, allowing the tissue to heal naturally. In this way, a sedative effect is achieved, which is required by the patient to obtain mobility, and is even recommended by specialists after surgery.
- Shockwaves: Using EMS devices outside the body, high-frequency sound waves are transmitted. These shock waves penetrate into the tissue and have a vasodilator effect. In this way, the body itself is stimulated to activate its natural defences and heal properly.
- Decompression and joint coaptation: These are manual techniques or manoeuvres that the physiotherapist performs with caution in order to decompress the area. These medium manipulation efforts seek to reduce tension and improve the inflamed space.
- Dry needling: Using fine acupuncture needles, dry needling seeks to bring relief from rotator cuff tendinitis. It is not valid for all patients, in fact, it is the physiotherapist who will establish its necessity.
Medications
Drug therapy includes:
- NSAIDs: Certain drugs such as Naproxen, Ibuprofen and others can reduce primary inflammation. The continuity and frequency of use should be regulated by a specialist, so they should never be self-medicated without the supervision of a doctor.
- Corticosteroids: Cortisone injection significantly helps to improve inflammation. It is usually administered with a local anaesthetic so as not to cause further pain in the tendons or joints. Keep in mind that this treatment is used when conservatives have failed and must be applied by a health specialist.
Surgeries
In advanced cases of shoulder tendinitis it is possible to perform surgical interventions, which are mentioned below:
- Rotator cuff repair: Surgery can be aimed at repairing one of the torn tendons in the rotator cuff using general or regional anaesthesia. These techniques are applied in cases where tendinosis has caused a partial or total rupture.
- Bursectomy: If the inflammation is not only in the tendons, but also in the bursa, it is advisable to use this removal technique.
Prevention for shoulder tendon inflammation
Regardless of a person's health condition, profession or sporting activities, tendonitis can be prevented.
The most effective preventive measures for this purpose are listed below:
- Warm up the shoulders: Any joint area must be well prepared for intensive physical exercise. The best way to do this is by warming up beforehand. With 15 minutes of gentle rotational movements, lifts, flexions, extensions and contractions is sufficient. Within these, stretching exercises are essential.
- Controlled exercise routines: Avoiding exercises in extreme postures, respecting biomechanics and using appropriate weights, it is possible to know the right weight for our physical condition.
- Vary movements and exercises: If only one shoulder is subjected to the same exercise it will probably become congested. Because of this, it is best to vary routines at different angles and in a coordinated manner.
- Improve proprioception: Stability and correct posture are essential. For this, proprioception exercises for athletes and anyone else are very useful. They will help you understand where your body parts are in relation to space at all times to avoid future injuries.
- Avoid a sedentary lifestyle: People who are not active on a frequent basis are likely to place a greater demand on immobilised tendons. This is because the tissues are not accustomed to working, and will recienten when a sudden movement is made or a task needs to be performed.
References
- Lewis, J. S. (2009). Rotator cuff tendinopathy. British journal of sports medicine, 43(4), 236-241. https://bjsm.bmj.com/content/43/4/236.short
- Seitz, A. L., McClure, P. W., Finucane, S., Boardman III, N. D., & Michener, L. A. (2011). Mechanisms of rotator cuff tendinopathy: intrinsic, extrinsic, or both?. Clinical biomechanics, 26(1), 1-12. https://www.sciencedirect.com/science/article/abs/pii/S0268003310002214
- Littlewood, C., Ashton, J., Chance-Larsen, K., May, S., & Sturrock, B. (2012). Exercise for rotator cuff tendinopathy: a systematic review. Physiotherapy, 98(2), 101-109. https://www.sciencedirect.com/science/article/abs/pii/S0031940611004536
- Littlewood, C., May, S., & Walters, S. (2013). Epidemiology of rotator cuff tendinopathy: a systematic review. Shoulder & Elbow, 5(4), 256-265. https://journals.sagepub.com/doi/abs/10.1111/sae.12028
- Littlewood, C., Malliaras, P., & Chance-Larsen, K. (2015). Therapeutic exercise for rotator cuff tendinopathy: a systematic review of contextual factors and prescription parameters. International Journal of Rehabilitation Research, 38(2), 95-106. https://www.ingentaconnect.com/content/wk/ijrre/2015/00000038/00000002/art00001
- Millar, N. L., Silbernagel, K. G., Thorborg, K., Kirwan, P. D., Galatz, L. M., Abrams, G. D., … & Rodeo, S. A. (2021). Tendinopathy. Nature reviews Disease primers, 7(1), 1. https://www.nature.com/articles/s41572-020-00234-1
- Rees, J. D., Maffulli, N., & Cook, J. (2009). Management of tendinopathy. The American journal of sports medicine, 37(9), 1855-1867. https://journals.sagepub.com/doi/abs/10.1177/0363546508324283
- Maffulli, N., Wong, J., & Almekinders, L. C. (2003). Types and epidemiology of tendinopathy. Clinics in sports medicine, 22(4), 675-692. https://www.sportsmed.theclinics.com/article/S0278-5919(03)00004-8/fulltext
- Riley, G. (2008). Tendinopathy—from basic science to treatment. Nature clinical practice Rheumatology, 4(2), 82-89. https://www.nature.com/articles/ncprheum0700
- Xu, Y., & Murrell, G. A. (2008). The basic science of tendinopathy. Clinical orthopaedics and related research, 466, 1528-1538. https://link.springer.com/article/10.1007/s11999-008-0286-4