Inflammation of the synovial fluid sacs in the hip is called hip bursitis. This ailment is common in people who play sports and in workers who have to lift heavy things, although all people are exposed to this disease.
In this post we will show you what hip bursitis is, what are the risk factors that increase the chances of contracting it and what are the symptoms that will help you detect the presence of this ailment. We invite you to continue reading because you will find all the information related to this inflammatory disease.
What is hip bursitis?
Hip bursitis can be divided into two types, one called trochanteric bursitis and the other called psoas iliacus bursitis, although this is not as common. This disease is of an inflammatory type and originates in the bursae that are located at the end of the greater trochanter and in the groin region, respectively. In the latter case the pain is not felt in the lower back but in the groin area.
In other words, hip bursitis is the inflammation that occurs in these bursae located in the aforementioned region, which appears when there is an excess of synovial fluid inside them. This causes the space in the joint cavity to be reduced, resulting in excessive pressure on the bursae, which leads to inflammation of the bursae.
What are the causes and risk factors for hip bursitis?
You need to know what risk factors and causes increase the likelihood of hip bursitis. This will help you by not placing further stress on the psoas iliacus and greater trochanter bursa.
Take a look at the list below:
- Age: although hip bursitis is not directly caused by the patient's advanced age, it can appear due to the presence of other diseases such as osteoarthritis and osteoporosis, in which the patient's age is a risk factor. Degenerative diseases can thus atrophy the joint tissues, causing the bursae to become inflamed.
- Trauma: blows, injuries and any dislocation or fracture of the hip can lead to the development of bursitis. This is possible due to stress on the joint area, causing an excess of synovial fluid in the bursa.
- Bone spurs: Osteophytes or bone spurs are also the cause of bursitis caused in the synovial bursa of the trochanter or iliac psoas. This is due to the malfunctioning of the joint causing extreme pressure on the bursa.
- Obesity: excess weight causes overloading of the hip joints, which leads to inflammation of the bursae and wear and tear of the hyaline cartilage.
- High-risk activities: inappropriate heavy lifting or sports that require strain on the lower back can be factors in the development of hip bursitis. An important antecedent of the ailment is the lack of warming up the affected area beforehand. The risk increases even more when repetitive movements are required on a permanent basis.
- Unbalanced diet: A diet rich in fat can cause uric acid to form microcrystals in the hip. This will lead to pressure on the bursae, which will become inflamed over time.
- Bad posture: not only lifting heavy objects without correct technique can lead to bursitis, but also sitting improperly or getting out of bed abruptly can cause inflammation of the bursae.
Best products for hip bursitis
Bestseller
-
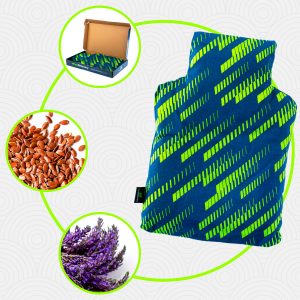
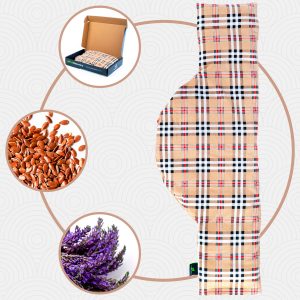
Heating Pad for Microwave Classic Bottle Shaped (Hearts)
$24.95 -
Heating Pad for Microwave Classic Bottle Shaped (Oxford)
$24.95 -
Heating Pad for Microwave Classic Bottle Shaped (Sport)
$24.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Hearts)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Oxford)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Sport)
$29.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Hearts)
$29.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Oxford)
$29.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Sport)
$29.95 -
Microwaveable Heating Pad for Pain Relief (Hearts)
$24.95 -
Microwaveable Heating Pad for Pain Relief (Oxford)
$24.95 -
Microwaveable Heating Pad for Pain Relief (Sport)
$24.95
-
Back Support Belt (Black)
$49.95 -
Back Support Belt (Green)
$49.95 -
Back Support Belt (Pink)
$49.95 -
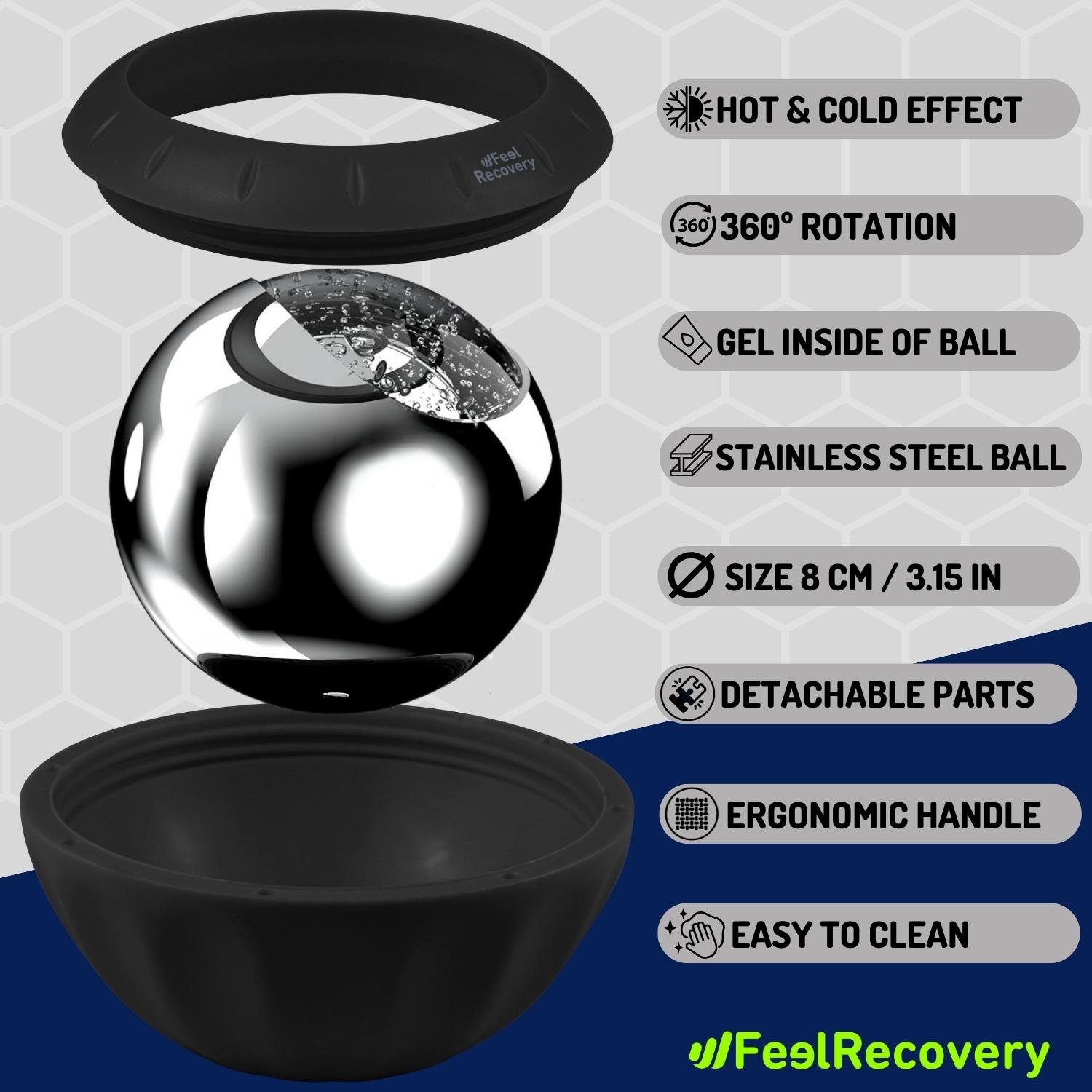
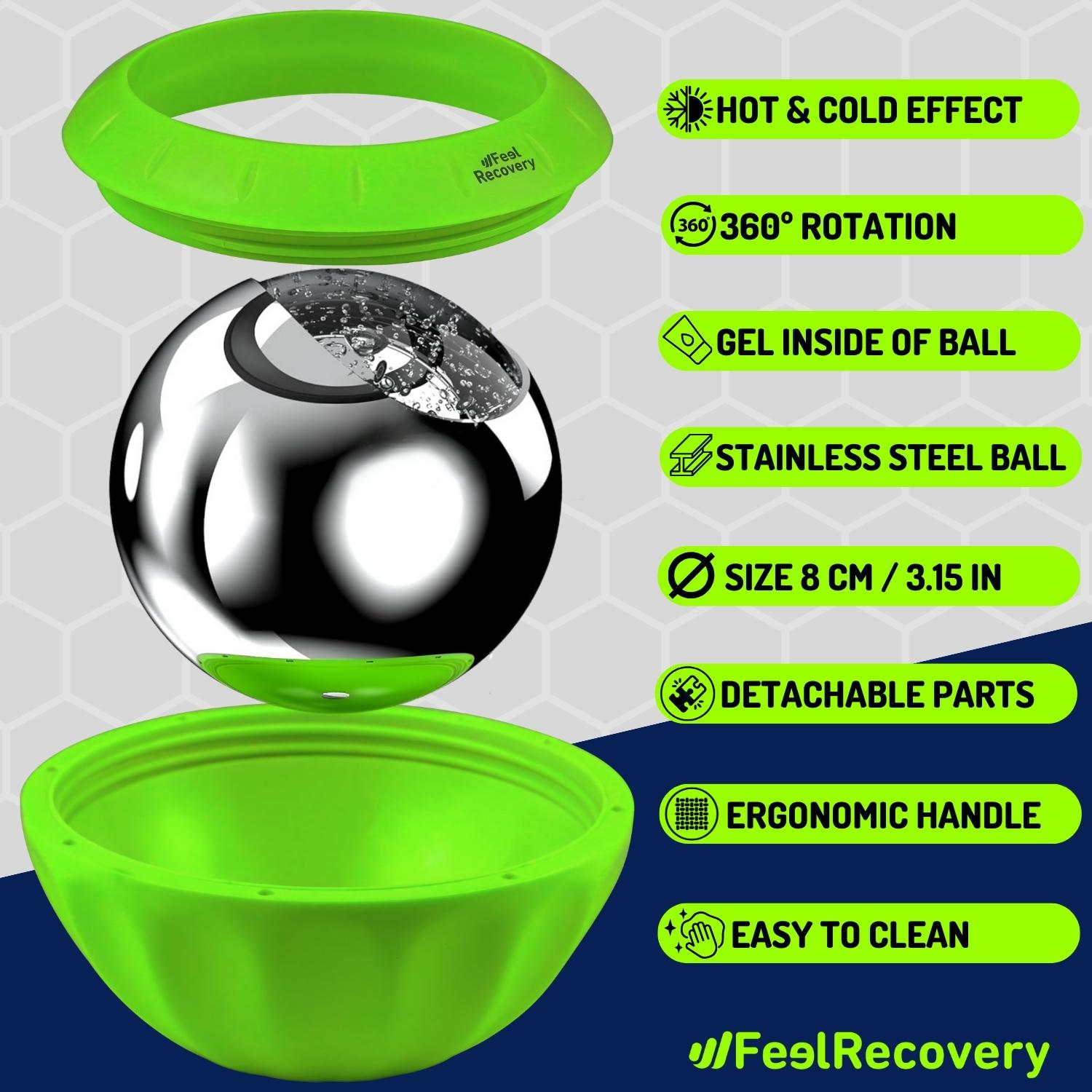
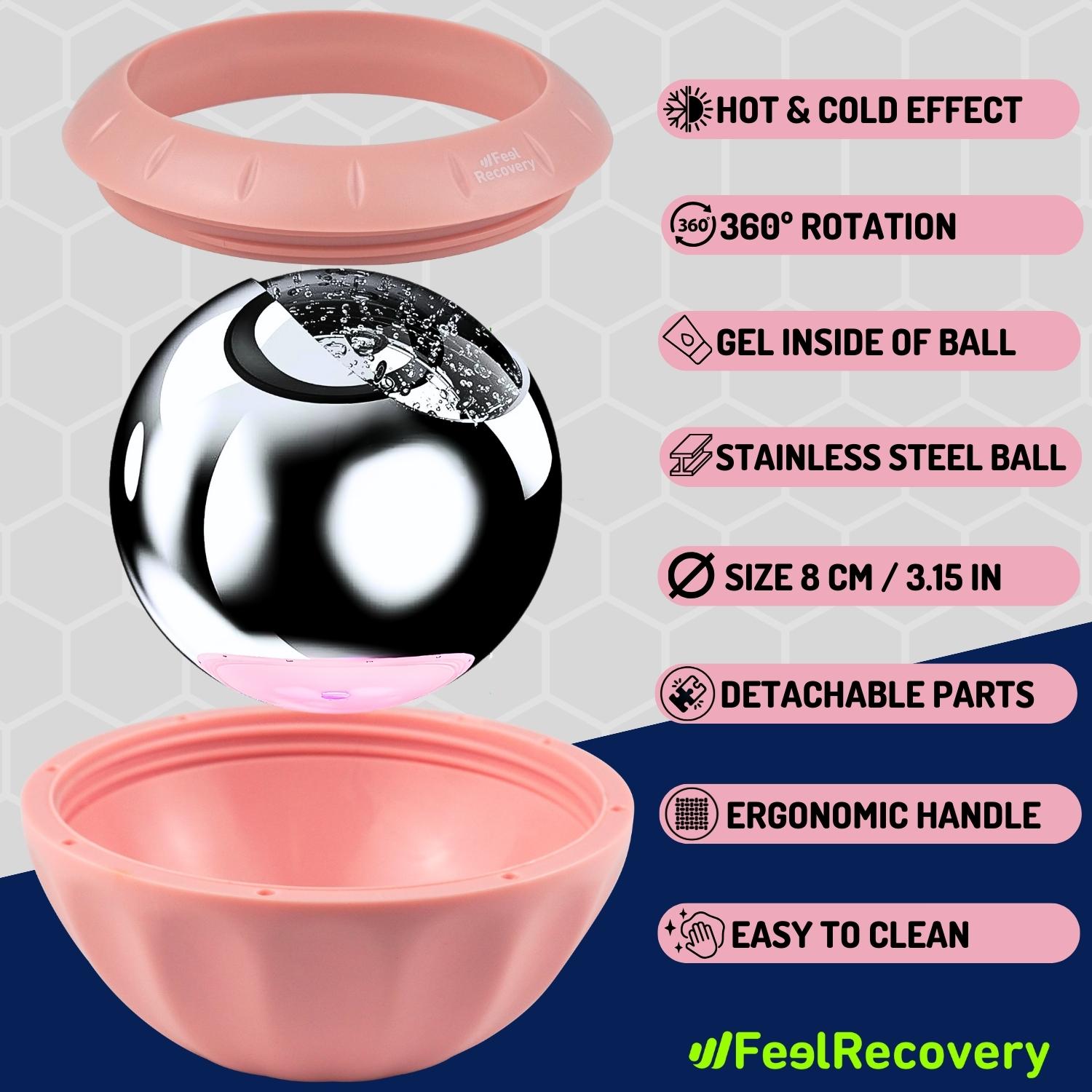
Ice Massage Roller Ball (Black)
$39.95 -
Ice Massage Roller Ball (Green)
$39.95 -
Ice Massage Roller Ball (Pink)
$39.95 -
Sacroiliac Support Belt (Black)
$29.95 -
Sacroiliac Support Belt (Green)
$29.95 -
Sacroiliac Support Belt (Pink)
$29.95 -
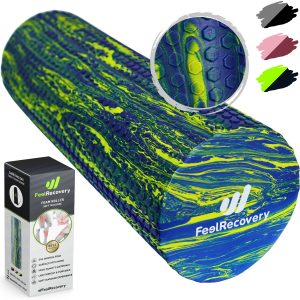
Soft Density Foam Roller for Recovery (Black)
$39.95 -
Soft Density Foam Roller for Recovery (Green)
$39.95 -
Soft Density Foam Roller for Recovery (Pink)
$39.95
Main symptoms that warn us that we have hip bursitis
Hip bursitis has a very noticeable and easy to detect symptomatology. For this reason we will show you below what are the signs and symptoms that you should be aware of
- Numbness: stiffness during certain movements, e.g. bending over, can be caused by irritation of the psoas iliacus or trochanter bursae. This is due to the enlargement of the bursa which prevents the joint from functioning properly.
- Pain: Many people confuse low back pain with hip bursitis. It should be borne in mind that in this condition the pain is more constant and does not disappear at the same speed. As there is less space in the joint capsule, the nerves that pass through this area are squeezed, causing discomfort for the patient.
- Appearance of lumps: nodules are likely to appear on the side of the back, which may be related to hip bursitis. It is advisable to see a doctor as a matter of urgency for a correct diagnosis.
- Limited sensitivity: tingling sensation and loss of sensitivity in the lower back are symptoms to be taken into account in the event of the possible appearance of inflammation in the trochanter bursae and iliac psoas.
- Loss of strength: some patients with hip bursitis are unable to lift the upper trunk of the body every time they bend down or cannot stand up in a chair due to muscle fatigue in the affected area.
- Swelling: Swelling in the lower back is less common than other symptoms, but patients have been found to have swelling in the area.
- Difficulty walking: Bursitis can affect the muscles of the lower back, making walking difficult for the patient. In some cases, asymmetrical ambulation may occur.
What treatments are available to improve the symptoms of hip bursitis?
Once hip bursitis has been diagnosed, the condition can be treated so that it goes into remission within a few weeks. To do this, it is necessary to apply different therapies, which we show you below.
Alternative and complementary therapies
Below you can read about the different alternative therapies that are used to treat inflammation of the bursae in the hip
- Heat and cold therapy: this type of treatment consists of applying elements that emit both temperatures. In this way, the benefits of cold and heat are used to reduce inflammation in the fascia lata tendon, in the psoas iliac synovial bursa and in the bursa of the greater trochanter. In addition, it increases the blood supply, thus causing a better dilatation of the vessels. In order to apply this technique, it should be borne in mind that the session time should not exceed 15 to 20 minutes and should start with the warm elements.
- Compression therapy: The implementation of compression therapy is at the sole discretion of the physician, because the bursae found in the greater trochanter and the psoas iliacus synovial bursa should not be compressed, as this will increase the irritation of the bursa and cause even more inflammation. If used correctly, the hip compression garment can achieve immobilisation of the joint, but it must be borne in mind that in this area the patient must be rested completely in order to achieve this objective.
- Massage therapy: As with compression therapy, massage therapy is not recommended for treating hip bursitis because it can increase irritation of the bursae due to the pressure exerted on the area. On the other hand, if massage therapy is used to stimulate balance, increase and decrease the patient's stress so that he/she can better cope with the pain, it is only recommended if prescribed by the acting physician.
- Acupressure therapy: As mentioned above, pressure should not be applied to the bursa areas of the hip, as this will cause more pain and inflammation. This does not mean, however, that this Chinese medicine cannot be applied to other strategic points of the body, because in this way the patient will release endorphins that will work as natural painkillers. Therefore, the implementation of this technique is at the discretion of the medical specialist.
- Thermotherapy: heat therapy can be applied to the lower back by means of different techniques that help to dilate the capillary walls of the tissues. This helps to reduce muscle stiffness, elongate the tendons and improve the opening of the joint cavity. All this will influence the pressure on the bursa before therapy, which will make the patient feel a sense of well-being and the disease will go into remission faster.
- Natural remedies using plants: Peppermint, ginger, chamomile and lavender all have analgesic and anti-inflammatory properties. For this reason, these natural plants are used for the preparation of infusions to be ingested by the patient to reduce stress and reduce inflammation and pain in the hip. It should be borne in mind that to use this complementary treatment it is necessary to consult a doctor beforehand.
- Healthy lifestyle habits: the aim of this therapy is for the patient to understand the complexity of hip bursitis and the causes that led to it. For this reason, the doctor teaches the patient how to cope with daily activities so that the bursa located in the hip is not re-injured. In this way, the person can learn how to exercise correctly, what kind of food to eat and the best time to rest the joint.
Nutritional supplements
This type of complementary treatment is based on including different components and nutrients in the patient's diet that will help to improve the symptoms and help hip bursitis to go into remission in the shortest possible time.
To do this, different components that are present in the joints are used, such as glucosamine and chondroitin sulphate. But in addition to this it is also possible to incorporate magnesium, hyaluronic acid, selenium, B vitamins and vitamin D. All these nutrients must be prescribed by the doctor and the mode of consumption must be chosen, which can be syrup, powder or pills.
Physiotherapy treatments
Physiotherapy is a technique used to reduce pain, inflammation and stiffness in hip bursitis. This treatment is based on repetitive exercises to restore movement and full opening of the hip joints.
There are different methods that are applied according to the physiotherapist's criteria. Among the most common are electrotherapy, based on electrical impulses to stimulate the nerves and vessels in the affected area; ultrasound, to produce internal heat; and laser application, which also stimulates blood flow. It should be noted that massage is not recommended for the treatment of bursitis, so self-massage should never be practised.
Medications
The symptoms of hip bursitis can be reduced by means of drug therapy. In this treatment, the patient is prescribed paracetamol or another type of opioid analgesic to reduce inflammation and control pain. In addition, NSAIDs (non-steroidal anti-inflammatory drugs) such as aspirin and ibuprofen may be prescribed. In cases where infections occur, the physician may choose antibiotics.
It follows that self-medication should never be practised, because of the complications that this can lead to either increased symptoms or internal bleeding. For this reason, drug therapy should be guided by a specialised physician.
Surgery and fluid removal
The bursae in the hip can be de-inflated by removing the synovial fluid. This is done using syringes where needles are placed directly into the affected area to remove all the excess fluid located in the joint.
It should be noted that this process is somewhat invasive and the patient's recovery is based on complete rest. On the other hand, synovial bursae can be removed by a surgical procedure called bursectomy.
What are the most effective prevention methods for hip bursitis?
See the following list in which we will explain different alternatives that will help you prevent the occurrence of hip bursitis
- Avoid sudden movements: sudden actions can affect the tensor fascia latae, which can cause pain in the hip joint area and cause the synovial bursa of the trochanter and iliac psoas to become inflamed.
- Correct posture: it is important to learn to sit with your back against the chair. In addition, if it is necessary to lift heavy things, this should be done with a straight back and with the knees pressed together to avoid injury to the hip muscles, causing less space in the bursae.
- Eat a balanced diet: foods that are rich in uric acid do not allow this toxic component to be eliminated from the blood, which generates microcrystals in the joints. This affects the opening of the joint, causing muscle tension and excess synovial fluid.
- Get enough sleep: It is important to rest the joint for as long as necessary. For this reason, resting for 7 to 8 hours will help the muscles and tendons relax to avoid injury to the synovial fluid sacs.
- Warm up the muscular area: if you are an athlete or if you have to do manual work that requires effort and demands on the hip, it is advisable that before carrying out this work you do stretching and warm-up movements. This will help your muscular and mental system prepare for the task.
- Stop all activity: If you feel pain in the hip area or if the area is swollen, it is advisable to see a doctor as soon as possible. This will help you avoid further swelling in the bursae and help the disease go into remission more quickly.
References
- Schapira, D., Nahir, M., & Scharf, Y. (1986). Trochanteric bursitis: a common clinical problem. Archives of physical medicine and rehabilitation, 67(11), 815-817. https://www.archives-pmr.org/article/0003-9993(86)90164-4/fulltext
- GORDON, E. J. (1961). Trochanteric bursitis and tendinitis. Clinical Orthopaedics and Related Research®, 20, 193-202. https://journals.lww.com/clinorthop/citation/1961/00200/trochanteric_bursitis_and_tendinitis.20.aspx
- Collee, G., Dijkmans, B. A. C., Vandenbroucke, J. P., & Cats, A. (1991). Greater trochanteric pain syndrome (trochanteric bursitis) in low back pain. Scandinavian journal of rheumatology, 20(4), 262-266. https://www.tandfonline.com/doi/abs/10.3109/03009749109096798
- Alvarez-Nemegyei, J., & Canoso, J. J. (2004). Evidence-based soft tissue rheumatology: III: trochanteric bursitis. JCR: Journal of Clinical Rheumatology, 10(3), 123-124. https://journals.lww.com/jclinrheum/Abstract/2004/06000/Evidence_Based_Soft_Tissue_Rheumatology__III_.6.aspx
- Raman, D., & Haslock, I. (1982). Trochanteric bursitis--a frequent cause of'hip'pain in rheumatoid arthritis. Annals of the Rheumatic Diseases, 41(6), 602-603. https://ard.bmj.com/content/41/6/602.short
- McAfee, J. H., & Smith, D. L. (1988). Olecranon and prepatellar bursitis. Diagnosis and treatment. Western Journal of Medicine, 149(5), 607. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1026560/
- Reilly, D., & Kamineni, S. (2016). Olecranon bursitis. Journal of shoulder and elbow surgery, 25(1), 158-167. https://www.sciencedirect.com/science/article/abs/pii/S1058274615004693
- Khodaee, M. (2017). Common superficial bursitis. American family physician, 95(4), 224-231. https://www.aafp.org/pubs/afp/issues/2017/0215/p224.html
- Rasmussen, K. J. E., & Fanø, N. (1985). Trochanteric bursitis: treatment by corticosteroid injection. Scandinavian journal of rheumatology, 14(4), 417-420. https://www.tandfonline.com/doi/abs/10.3109/03009748509102047
- Sayegh, E. T., & Strauch, R. J. (2014). Treatment of olecranon bursitis: a systematic review. Archives of orthopaedic and trauma surgery, 134, 1517-1536. https://link.springer.com/article/10.1007/s00402-014-2088-3