- What is dislocation of the shoulder joint?
- What are the causes and risk factors for shoulder dislocation?
- Best products for shoulder dislocation
- Main signs and symptoms that warn us that we have a shoulder dislocation
- What is the first aid for a dislocated shoulder?
- What methods of prevention are the most effective for shoulder dislocation?
One of the most common injuries is dislocation of the shoulder joint. This is due to the causes and risk factors for this type of musculoskeletal injury. For this reason, it is important to know what a dislocated shoulder is and what are the symptoms of a dislocation in the joint of the glenoid socket of the scapula.
You can read about the partial or complete slippage of the head of the humerus below. We will explain, in detail, how to prevent this trauma and how to practice first aid using physiotherapeutic protocols. Have a look.
What is dislocation of the shoulder joint?
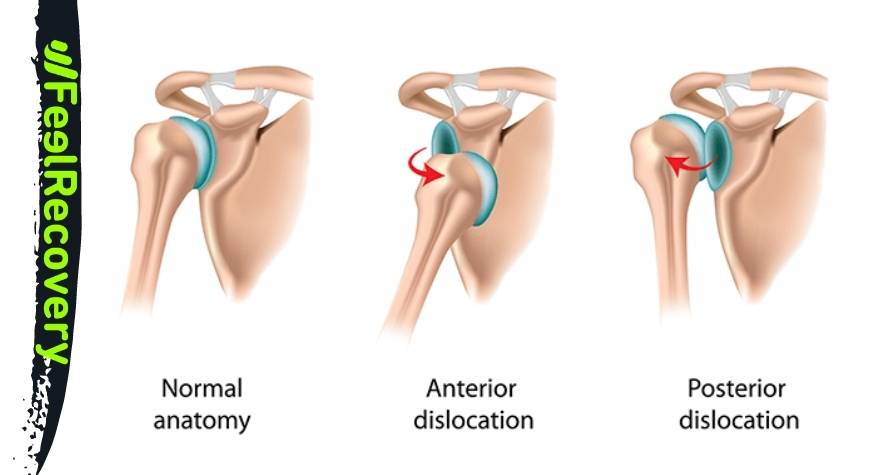
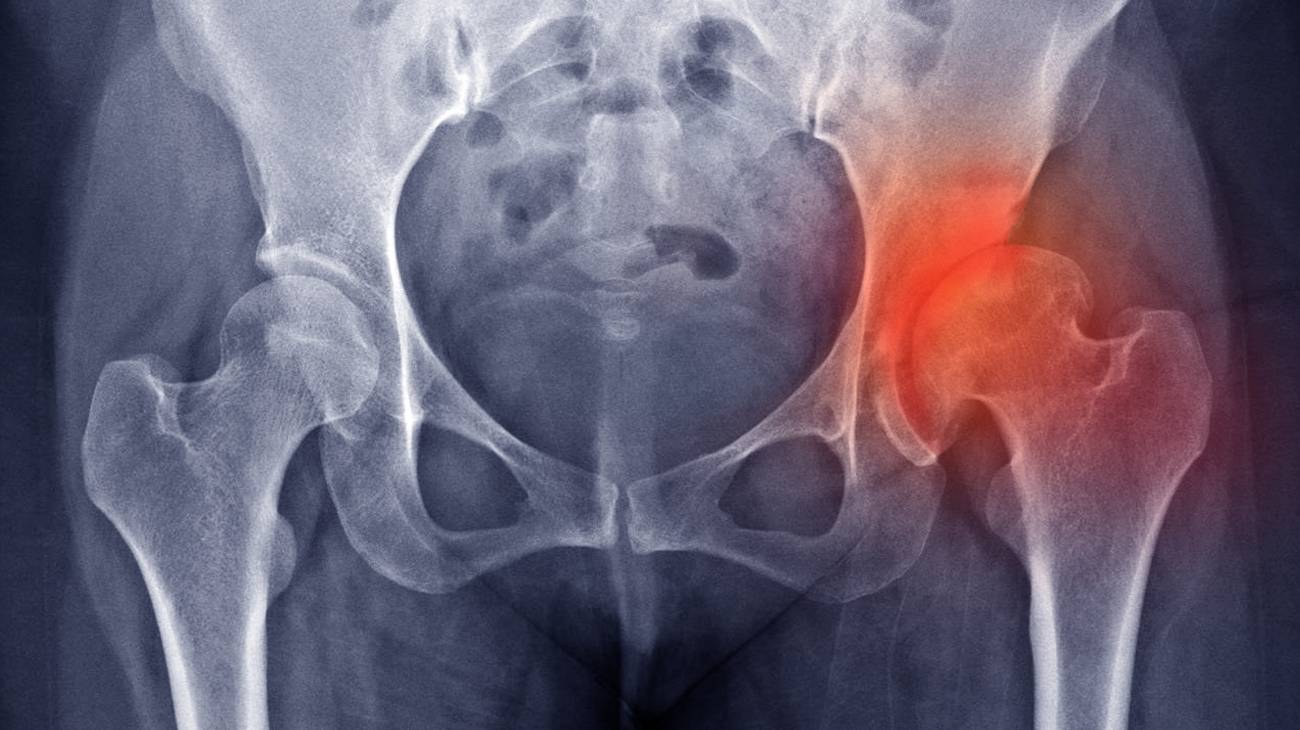
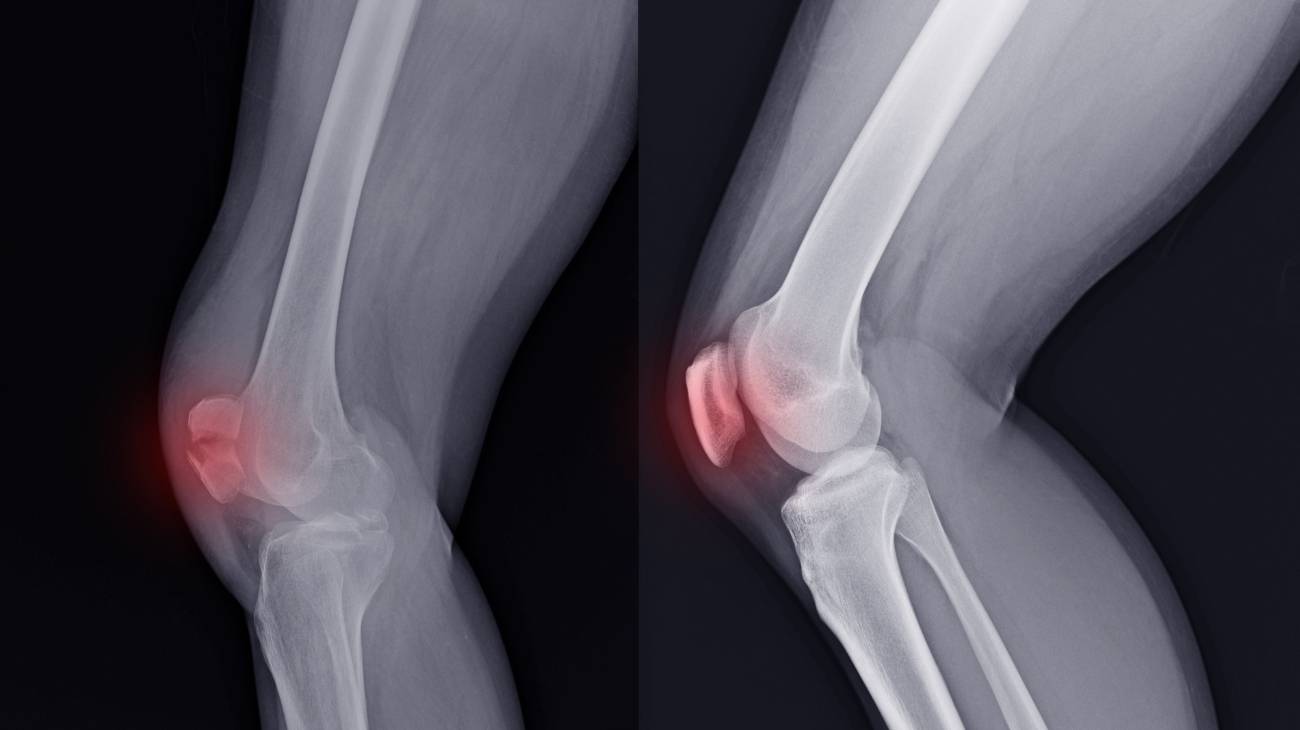
Shoulder dislocation occurs when there is a separation, partial or complete, between the head of the humerus bone and the glenoid socket of the scapula. Depending on the type of slippage, it can be classified as a posterior or anterior shoulder dislocation. The reference point is the approach of the humerus to the acromion or coracoid process, respectively.
It is one of the most common injuries among males aged 20-35 years and one of the most common dislocations. Recovery time will depend on physiotherapy treatment and the extent of the injury, but usually this dislocated joint is aligned or reduced within a month.
What are the causes and risk factors for shoulder dislocation?
Risk factors that increase the likelihood of a separation between the humerus and the glenoid socket of the shoulder blade include:
- Falls and hard impacts: Subluxation of the humeral head is very common when a person falls with the arm outstretched and receives blows from domestic, sports or traffic accidents.
- Lack of pre-stretching: Stretching the muscles and ligaments helps to keep the rotator cuff and shoulder in the correct range. When a demanding task needs to be performed, lack of preparation can lead to shoulder dislocation.
- Osteoarthritis: Autoimmune and degenerative diseases cause separation of the bony tissues in the glenoid socket.
- Previous dislocations: As the shoulder is a joint that suffers more dislocations, having a history of the same injury aggravates relapses in these traumas.
- Sports: Boxing, tennis, rugby and gymnastics are activities that tend to cause slippage of the humeral head on the scapula. Although these are not the only sports that cause this injury, they are considered high risk.
- Unbalanced diet: To help keep the ligaments in perfect condition, it is necessary to ingest potassium, calcium and other minerals. If this does not happen, the fibres weaken, helping to cause dislocations.
- Sedentary lifestyle: Lack of physical activity is an important risk factor to take into account in dislocated shoulder injuries and in many other pathologies, at least 45 minutes a day of moderate physical activity is recommended.
- Electrical shocks: Repetitive manual activities and involuntary contractures resulting from receiving an electric shock are considered risk causes that often lead to humeral head displacement.
- Congenital diseases: A patient is more likely to be injured with a shoulder dislocation if the humero-glenoid joint is deformed due to spurs or lack of articular cartilage from birth or other diseases.
Best products for shoulder dislocation
Bestseller
-
Acupressure Mat and Pillow (Black/Gray)
$49.95 -
Acupressure Mat and Pillow (Green/Navy)
$49.95 -
Acupressure Mat and Pillow (Pink/Bordeaux)
$49.95 -
Acupressure Pillow (Black/Gray)
$29.46 -
Acupressure Pillow (Green/Navy)
$29.46 -
Acupressure Pillow (Pink/Bordeaux)
$29.46 -
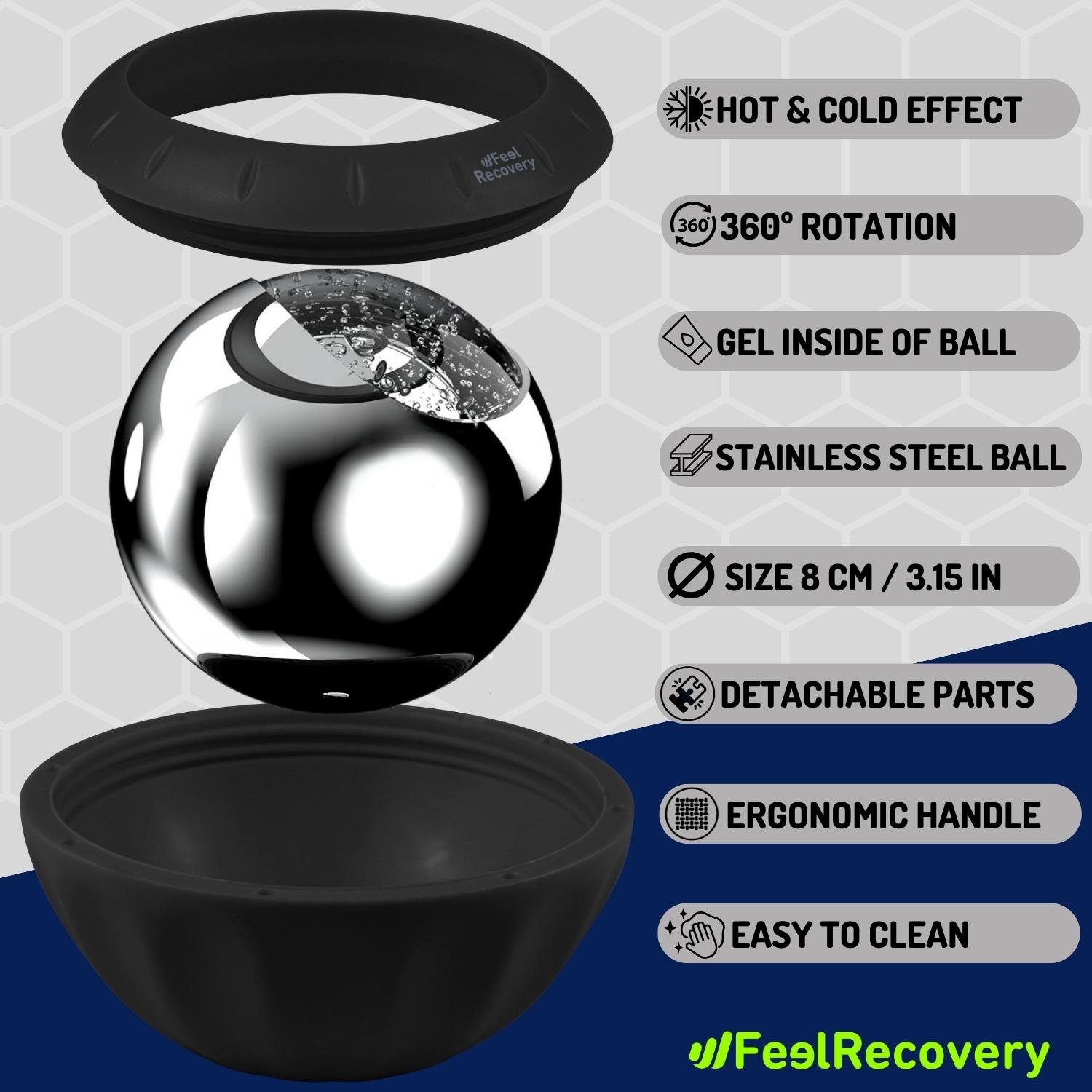
Ice Massage Roller Ball (Black)
$39.95 -
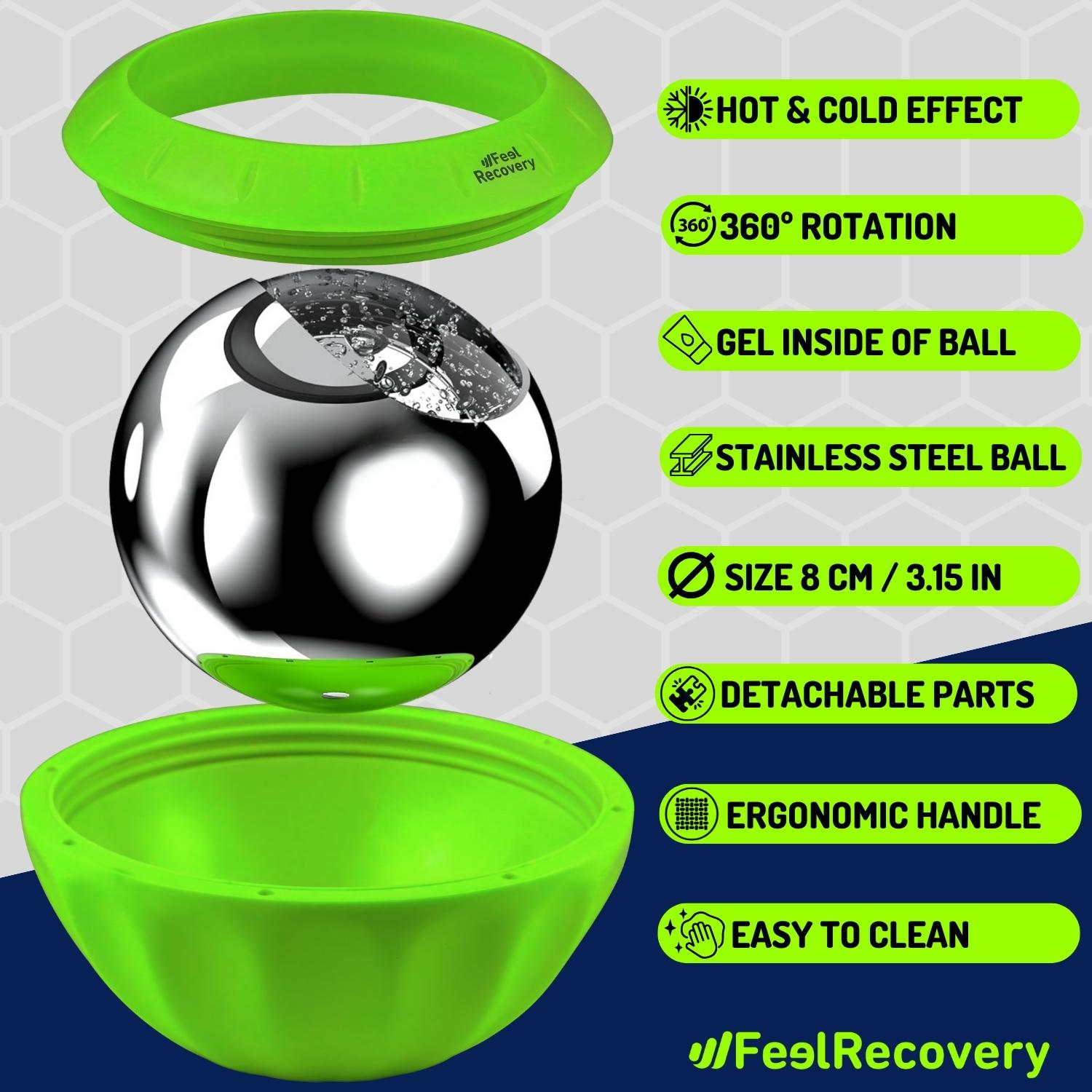
Ice Massage Roller Ball (Green)
$39.95 -
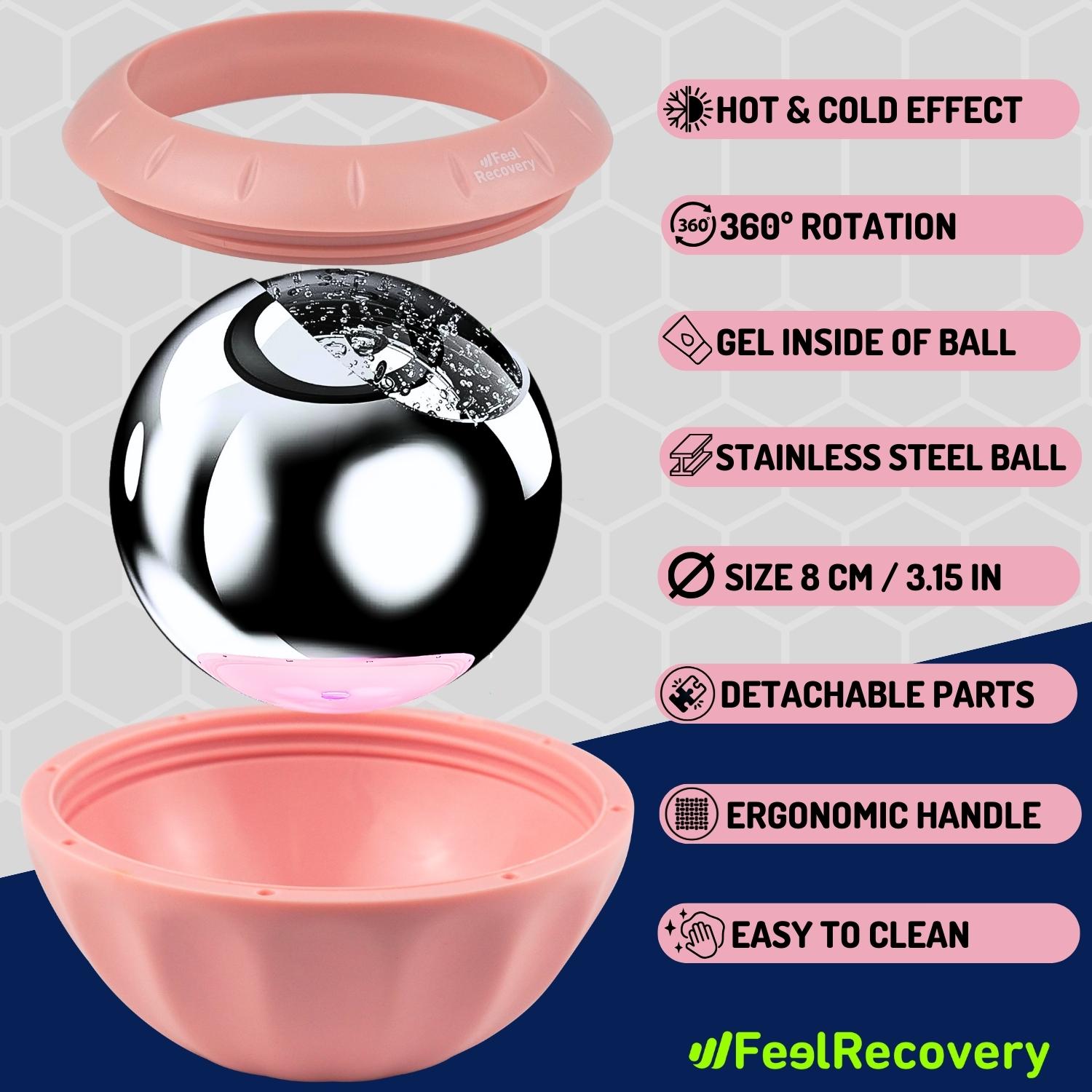
Ice Massage Roller Ball (Pink)
$39.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Hearts)
$24.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Oxford)
$24.95 -
Microwave Heating Pad for Neck & Shoulder Pain Relief (Sport)
$24.95 -
Microwave Heating Pad for Neck Pain Relief (Hearts)
$19.95 -
Microwave Heating Pad for Neck Pain Relief (Oxford)
$19.95 -
Microwave Heating Pad for Neck Pain Relief (Sport)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Hearts)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Oxford)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Sport)
$19.95 -
Shoulder Support Brace (Black)
$24.95 -
Shoulder Support Brace (Green)
$24.95 -
Shoulder Support Brace (Pink)
$24.95 -
Trigger Point Massage Stick (Black)
$14.95 -
Trigger Point Massage Stick (Green)
$14.95 -
Trigger Point Massage Stick (Pink)
$14.95
Main signs and symptoms that warn us that we have a shoulder dislocation
The main symptoms that will alert you to the presence of a dislocated shoulder are as follows:
- Great effort to move the arm: Performing biomechanical movements of adduction and flexion in the upper limbs will be difficult to do due to the malfunctioning of the shoulder joint.
- Pain: This is one of the main symptoms that appears when there is a shoulder dislocation. This is generated by the large number of nerve roots that are affected if there is a partial or total displacement in the glenoid cavity.
- Asymmetry: When a shoulder dislocation occurs, it is possible to see with the naked eye the lack of symmetry between the two shoulders of the trauma patient.
- Inflammation: The large amount of blood that is generated due to the work done by the immune system causes the shoulder area to swell and in some cases redden.
- Muscle weakness: This is caused by spasms in the muscle tissues resulting in loss of strength in the arm and hands.
- Muscle contracture in the trapezius: Incorrect position can lead to involuntary tensions in the muscle structure of the back, neck and arms.
- Numbness: The tingling sensation and loss of sensation are caused by a lack of normal blood supply.
What is the first aid for a dislocated shoulder?
There are different methods that can be applied to treat a trauma patient and perform first aid safely. This is the case of the PRICE protocol, which consists of a succession of steps that form the acronym mentioned above to act in the event of a dislocated shoulder.
The first aid protocol indicates these steps for treating a dislocated shoulder
- Cessation of activity: The first thing to do in the event of shoulder trauma is to stop the action that caused the dislocation of the joint. To do this, the affected area must be protected to avoid aggravating the displacement of the glenoid cavity.
- Rest: The patient should then calm down and rest until the next steps are taken or until the doctor arrives. To do this, the patient should lie still and avoid moving the neck, shoulder and arm.
- Cold therapy: It is important to include the application of cold to the affected area in the first aid. This will help to reduce inflammation and pain by using ice gel packs or ice packs. The session should not exceed 20-25 minutes and should be left to rest and reapplied at least 3-4 times a day.
- Use of compressive clothing: What should be done at this stage is to keep the shoulder joint as fixed as possible to prevent further subluxation and displacement of the dislocation from developing into a more serious injury. Compressive shoulder braces or elastic bandages can be used for this purpose.
- Elevation: It is important to keep the shoulder as high as possible in relation to the height of the heart to avoid increased blood flow and thus reduce swelling. A slightly lying position with the shoulder immobilised will help to prevent bruising and blood clots.
Once these steps have been completed, it is necessary to go to the doctor for a professional assessment of the situation and to choose the method for repositioning the shoulder, the most common techniques that can only be performed by a specialist are:
- Stimson's manoeuvre.
- Scapular manipulation.
- External rotation.
- Milch technique.
- Spaso technique.
- Davos technique.
- Traction-countertraction.
What methods of prevention are the most effective for shoulder dislocation?
Shoulder dislocation can be avoided if different preventive aspects are taken into account. We will show you the most important ones:
- Strengthen the bone structure of the shoulder: It is important to maintain a balanced diet rich in calcium and vitamin D, these nutrients will help to combat the appearance of shoulder dislocations.
- Warm-up exercises: If you have to practice a demanding sport for the shoulder, it is advisable to warm up the entire joint by means of movements that increase the degree of complexity. This is important in volleyball, gymnastics and tennis.
- Use compression clothing: The use of compression shoulder braces, lumbar supports and elbow braces help to keep the structure of the trunk and limbs in the right place. This will prevent displacement in the glenoid cavity.
- Reduce the likelihood of falls in the home: This will require you to consider uneven floors, slippery areas, the quality of lighting, objects that can cause tripping and the general condition of the building.
- See an ophthalmologist regularly: Knowing the state of your eyesight is important to avoid domestic falls and traffic accidents. Don't forget that these two causes are among the most common in shoulder dislocations.
- Control osteoporosis: This bone weakness disease is common in women of menopausal age. For this reason, it is advisable to control thyroid hormone replacement by means of bisphosphonate-type inhibitor drugs.
- Avoid "nursemaid's elbow" syndrome: This trauma occurs mostly in children because of the pulling of the elbow and shoulder that minors suffer when they start walking. It is caused by sudden movements made by parents or caregivers when the child loses stability.
- Work to make the joint more flexible: If you are an athlete, try stretching the muscles and tendons to improve the range of motion in the shoulder, as well as doing joint mobility exercises. This will help keep the joint less likely to get injured.
- Visit the doctor at the slightest symptom: If you hear a popping sound or feel pain in your shoulder, it is advisable to visit the doctor to rule out any type of shoulder dislocation by means of an X-ray.
References
- Cutts, S., Prempeh, M., & Drew, S. (2009). Anterior shoulder dislocation. The Annals of The Royal College of Surgeons of England, 91(1), 2-7. https://publishing.rcseng.ac.uk/doi/full/10.1308/003588409X359123
- Cunningham, N. J. (2005). Techniques for reduction of anteroinferior shoulder dislocation. Emergency Medicine Australasia, 17(5‐6), 463-471. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1742-6723.2005.00778.x
- Hovelius, L. (1982). Incidence of shoulder dislocation in Sweden. Clinical Orthopaedics and Related Research (1976-2007), 166, 127-131. https://journals.lww.com/corr/Citation/1982/06000/Incidence_of_Shoulder_Dislocation_in_Sweden.21.aspx
- Simonet, W. T., & Cofield, R. H. (1984). Prognosis in anterior shoulder dislocation. The American journal of sports medicine, 12(1), 19-24. https://journals.sagepub.com/doi/abs/10.1177/036354658401200103
- Beeson, M. S. (1999). Complications of shoulder dislocation. The American journal of emergency medicine, 17(3), 288-295. https://www.sciencedirect.com/science/article/abs/pii/S0735675799901274
- Krøner, K., Lind, T., & Jensen, J. (1989). The epidemiology of shoulder dislocations. Archives of orthopaedic and trauma surgery, 108, 288-290. https://link.springer.com/article/10.1007/BF00932317
- Hayes, K., Callanan, M., Walton, J., Paxinos, A., & Murrell, G. A. (2002). Shoulder instability: management and rehabilitation. Journal of Orthopaedic & Sports Physical Therapy, 32(10), 497-509. https://www.jospt.org/doi/abs/10.2519/jospt.2002.32.10.497
- Aronen, J. G., & Regan, K. (1984). Decreasing the incidence of recurrence of first time anterior shoulder dislocations with rehabilitation. The American journal of sports medicine, 12(4), 283-291. https://journals.sagepub.com/doi/abs/10.1177/036354658401200408
- Karatsolis, K., & Athanasopoulos, S. (2006). The role of exercise in the conservative treatment of the anterior shoulder dislocation. Journal of Bodywork and Movement Therapies, 10(3), 211-219. https://www.sciencedirect.com/science/article/abs/pii/S1360859205001300
- Handoll, H. H., & Al‐Maiyah, M. A. (2004). Surgical versus non‐surgical treatment for acute anterior shoulder dislocation. Cochrane Database of Systematic Reviews, (1). https://www.cochranelibrary.com/cdsr/doi/10.1002/14651858.CD004325.pub2/full