- What is osteoarthritis of the knee or inflammation of the knee joint?
- What are the causes and risk factors for osteoarthritis of the knee?
- Best products for knee arthritis
- Main symptoms that warn us of arthritis of the knee
- What treatments are available to improve the symptoms of osteoarthritis in the knee?
- What are the most effective methods of prevention for osteoarthritis of the knee?
Inflammation in the knee is a progressive disease that causes muscle stiffness and pain when making bending movements. It is therefore a good idea to find out what osteoarthritis of the knee is and what causes it. To do so, read on to the end of this article.
We will help you to detect the main symptoms of osteoarthritis of the knee that may appear in your body. You will also find out about the treatments available to relieve the pain and put the disease into remission. Don't miss anything because there is much more to discover in this post.
What is osteoarthritis of the knee or inflammation of the knee joint?
Osteoarthritis of the knee is the wear and tear of the articular cartilage located inside the capsule with synovial fluid causing inflammation in the joint. The onset of this disease may be due to errors in the autoimmune system, although it is also possible to find precedents in other diseases.
The most common symptoms of osteoarthritis are pain, muscle stiffness, redness and swelling in the affected area. Although there is no cure for this degenerative disease, it is possible, with appropriate treatment, to make the symptoms disappear and go into remission, giving the patient a better quality of life.
What are the causes and risk factors for osteoarthritis of the knee?
Below is a list of all the circumstances and elements that increase the likelihood of osteoarthritis in the knee.
- Obesity: being overweight flattens the synovial membrane, making the space in the joint capsule with fluid smaller. This leads to wear and tear on the cartilage and, in some cases, the bones, causing severe pain and crunching when the knee is flexed.
- Sedentary lifestyle: this is another important cause of osteoarthritis in the joint. Lack of movement and exercise means that the knee does not work properly, so any effort can injure the joint.
- Poor diet: an unbalanced diet rich in uric acid causes the joint cartilage to function poorly. This is because the crystals that are generated are not eliminated in the urine, but lodge in the joint cavity.
- Hereditary factors: about 5% of people who suffer from osteoarthritis of the knee have a genetic background, although this relationship has not been fully proven as to whether it is a cause or not.
- Smoking: Smoking and drinking alcohol are two causes that increase the likelihood of developing osteoarthritis of the knee.
- Age and gender: people over the age of 50 and especially women are the most common age group for this type of ailment.
- Muscle overload: Lifting heavy objects can cause injuries that lead to osteoarthritis of the knee. This increases when repetitive movements are performed, periodically straining the joint.
- High-impact activities: sports and any other type of activity in which the person must constantly jump can cause crushing of the synovial membrane, which leads to erosion of the articular cartilage.
- Trauma: breaks or injuries can lead to osteoarthritis of the knee in the future. This may be related to tissue rupture or the effect of septic factors.
- Congenital malformations: People born with knee deformities can develop osteoarthritis, due to the appearance of nodes or protruding bones that misalign the femur with the knee.
Best products for knee arthritis
Bestseller
-
2 Knee Compression Sleeve (Black/Gray)
$19.95 -
2 Knee Compression Sleeve (Green/Navy)
$19.95 -
2 Knee Compression Sleeve (Pink/Bordeaux)
$19.95 -
2 Patella Knee Strap (Black/Gray)
$14.95 -
2 Patella Knee Strap (Green/Navy)
$14.95 -
2 Patella Knee Strap (Pink/Bordeaux)
$14.95 -
Heating Pad for Microwave Classic Bottle Shaped (Hearts)
$19.95 -
Heating Pad for Microwave Classic Bottle Shaped (Oxford)
$19.95 -
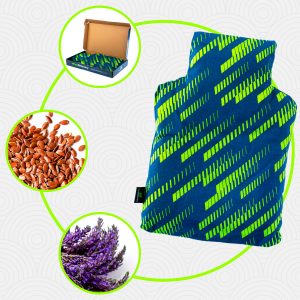
Heating Pad for Microwave Classic Bottle Shaped (Sport)
$19.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Hearts)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Oxford)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Sport)
$29.95 -
Microwaveable Heating Pad for Pain Relief (Hearts)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Oxford)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Sport)
$19.95
Main symptoms that warn us of arthritis of the knee
Pay attention to the following list because you will learn in detail the main symptoms and signs that warn you of the presence of inflammation in the knee joint that can cause osteoarthritis.
Let's start:
- Decreased movement of the joint: this symptom is usually not detected by the patient himself. It is possible to realise the presence of the disease when the person begins to have difficulty walking.
- Deformity: the presence of crystals in the cartilage affects the synovial fluid which causes the membrane of the joint cavity to slip out of place and causes the bones to become misaligned in relation to the knee.
- Redness and swelling: blood flow is affected by the malfunctioning knee, causing more blood to concentrate in the affected area.
- Stiffness in the muscle-tendon structure: this is due to the tissues becoming stiffer and bulging in the knee. This symptom is usually common in the morning after a night's rest.
- Loss of strength in the knee: as the muscle structure is affected, the knee loses strength. So every time you want to carry a heavy item or climb a ladder, the joint bends involuntarily.
What treatments are available to improve the symptoms of osteoarthritis in the knee?
There are different therapies and treatments that help to improve the symptoms of osteoarthritis in the knee. Below, you can read about the techniques that exist today and that can be useful according to the progress of the disease.
The treatments are:
Alternative and complementary therapies
Complementary treatments are techniques that are used to mitigate the pain, reduce swelling and stiffness and find a mental balance for the patient. They must be accompanied by the pharmacological therapy prescribed by the doctor. We will show you what these treatments are about:
- Cold and heat therapy: the application of cold and heat to the affected area is a technique used to reduce inflammation in the joint. The aim of this treatment is for the patient to relax the muscle structure and thus prevent stiffness from damaging the synovial capsule. This therapy is ideal for use in patients with diabetes, high blood pressure or recent trauma. To use cold heat for osteoarthritis of the knee, it is necessary to place a hot water bottle for no more than 5 minutes, then a cold pack or gel and, finally, heat again. This treatment should not exceed 15 to 20 minutes.
- Compression therapy: Neoprene or rigid bandages and discharge clamps are alternative elements used in this type of compression treatment. This technique serves to stiffen or semi-rigidify the joint by improving blood flow and correcting the posture of the knee. This allows the cartilage to rest and the synovial membrane to regain its size. The short-term results are a reduction in pain and inflammation.
- Massage therapy: by means of rubbing and pressure on the soft tissues of the body, the aim is to stimulate the nervous system to produce mental relaxation and decompress the musculotendinous structure of the knee. There are different techniques that are used, which are at the discretion of the practitioner's choice, the best known being kneading, gliding and manual pressure.
- Acupressure therapy: this millenary oriental technique consists of pressing, with the fingers and palms of the hands, different areas of the body to produce a sensation of well-being, both physical and mental. By means of massage manoeuvres it is possible to make the Chi flow and reduce fatigue to improve the stretching of the muscles and thus obtain a greater opening of the joint. Please note that this practice should only be carried out by a professional and you should consult your doctor beforehand if it is advisable.
- Thermotherapy: heat is an element that can be used to activate blood flow and thus oxygenate the soft tissues. This results in the patient relaxing and moving the joint more normally, which helps to achieve a greater sense of wellbeing. Vasodilation and sedation can be generated by means of electric blankets, hot water bottles, baths and pads with silicate-type gels.
- Natural herbal remedies: Herbs also offer components that help reduce muscle stiffness and benefit the opening of the joint cavity with synovial fluid. This therapy can be used by means of baths, called footbaths, or by infusions to be taken by the patient. Among the most popular plants are lavender, boldo, thyme, laurel, rosemary, sage and ginger. To opt for this type of therapy, it is necessary to consult a doctor beforehand to avoid future injuries.
- Ultrasound: in this treatment, energy is transmitted to the affected area by means of equipment that emits mechanical waves at a very high sound frequency. This causes the tissues to become more flexible - thanks to the collagen - and reduces the pain in the joint.
- Meditation and relaxation: body and mind are the two pillars on which this complementary treatment is based. The aim is to find mental strength to achieve balance and to be able to cope with the pain and the consequences of osteoarthritis of the knee. There are different techniques used in meditation, but the most commonly used for this disease is breathing control to reduce anxiety.
- Aromatherapy: vanilla, mint, lavender and rosemary are some of the aromatic materials used in this alternative therapy. This treatment seeks to mix essential oils with flowers, bark and seeds to produce relaxing scents. These aromas act on the patient's mental part to loosen the muscles and tendons of the knee, find emotional balance and reduce the pain.
- Acupuncture: Oriental medicine seeks to stimulate the central nervous system so that, by means of impulses produced by needles, it blocks the sensation of pain in the brain. This therapy also helps the blood flow by increasing the heat in certain areas in order to obtain the benefits of thermotherapy treatments. The main goal of this Chinese therapy is to improve the patient's daily activities.
- Biofeedback: the aim of this rehabilitative approach is to show the patient different medical parameters that occur in his body as a consequence of the disease. This helps the patient to learn more about osteoarthritis of the knee so that they can make better decisions in their daily life. In some cases, electronic equipment is used to monitor different variables in the body together with the patient.
- Healthy lifestyle habits: eating foods low in uric acid, walking, not doing exercises that strain the knee joint and giving up smoking are some of the criteria taken into account in this type of alternative and complementary therapies. It is necessary to consult a medical professional to achieve better results because, according to the progress of the disease, the patient will be able to do more or less activities.
Nutritional supplements
This type of therapy is responsible for reinforcing the patient's nutrition by means of syrups or tablets so that the body can assimilate nutrients that will reduce the symptoms of osteoarthritis of the knee. In other words, by means of selenium and other minerals it is possible to reduce the pain in the affected area.
In addition, the inclusion of extra vitamins and proteins will help the sufferer to have more energy to combat the fatigue caused by the inflammatory disease. The creation of collagen also benefits from this type of alternative treatment.
Physiotherapy treatments
In addition to protecting the joint, reducing pain and improving mobility in the knee, physiotherapy helps to keep the joint functioning so that the impact of the disease is lessened and the patient's life is significantly improved.
Various repetitive exercise techniques of short duration are used to achieve flexibility in the muscle-tendon structure and thus obtain a better opening of the synovial joint cavity. It is necessary to consult a doctor before undergoing this type of practice, as it can cause serious injury if not performed by a trained professional.
Medications
Drug therapy should be prescribed by the rheumatologist and should never be self-medicated as it could lead to serious complications in the development of the disease. Simple analgesics, anti-inflammatory drugs, cartilage builders and, in some cases, glucocorticoid and hyaluronic acid infiltrations are used in these treatments.
Nonsteroidal anti-inflammatory drugs are also included, but these have long-term side effects that affect the stomach, can lead to hypertension, liver disorders and heart disease. Therefore, their use is not recommended for a prolonged period of time.
Surgery
Osteotomy is the most common surgery performed in advanced cases of osteoarthritis of the knee. This surgical technique involves reconfiguring the shapes of the bones back into the correct position to improve the function of the joint.
It is also possible to find patients who have undergone arthroscopy and complete joint replacement. In the latter case, the knee is replaced with a prosthesis to improve its function.
What are the most effective methods of prevention for osteoarthritis of the knee?
Here are some tips to help you reduce the risk of osteoarthritis of the knee:
- Have a healthy lifestyle: regular physical activity, a balanced diet rich in vitamins D and E and Omega 3 will help prevent osteoarthritis of the knee. This is because the joint will have adequate collagen and texture to work properly.
- Get enough rest: it is proven that sleeping 7 to 8 hours a day improves muscle relaxation, so it also preserves the synovial membrane inside the joint capsule.
- Don't lift too much weight: if you decide to do weightlifting or any other sport, you should seek professional guidance and compression support for your knee and other joints that are affected by weightlifting. On the other hand, if you work somewhere where you have to lift heavy weights, try to use safety elements and rest for 10 to 15 minutes every 2 hours.
- At the slightest symptom, visit your doctor: early detection of the disease helps to halt its progression and put it into remission in the short or medium term.
- Don't smoke or drink alcohol: remember that smoking causes the immune system not to work properly, which can lead to autoimmune osteoarthritis in the knee.
- Control your postural hygiene: climbing or descending stairs, as well as sitting and standing in an inappropriate way, can cause injuries to the joint due to excessive stress on the cartilage. This will lead to osteoarthritis of the knee in the medium term.
- Avoid high-impact sports: As we have already mentioned throughout this post, high-intensity physical activities with a high impact on the joints can be harmful in the long term. If you practice running, try to do it on soft surfaces such as dirt or grass, avoiding the asphalt of the road.
References
- Neugebauer, V., Han, J. S., Adwanikar, H., Fu, Y., & Ji, G. (2007). Techniques for assessing knee joint pain in arthritis. Molecular pain, 3, 1744-8069. https://journals.sagepub.com/doi/pdf/10.1186/1744-8069-3-8
- Balabaud, L., Gaudias, J., Boeri, C., Jenny, J. Y., & Kehr, P. (2007). Results of treatment of septic knee arthritis: a retrospective series of 40 cases. Knee Surgery, Sports Traumatology, Arthroscopy, 15(4), 387-392. https://link.springer.com/article/10.1007/s00167-006-0224-5
- Cole, B. J., & Harner, C. D. (1999). Degenerative arthritis of the knee in active patients: evaluation and management. JAAOS-Journal of the American Academy of Orthopaedic Surgeons, 7(6), 389-402. https://journals.lww.com/jaaos/Abstract/1999/11000/Degenerative_Arthritis_of_the_Knee_in_Active.5.aspx
- Lange, A. K., Vanwanseele, B., & Fiatarone singh, M. A. (2008). Strength training for treatment of osteoarthritis of the knee: a systematic review. Arthritis Care & Research: Official Journal of the American College of Rheumatology, 59(10), 1488-1494. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.24118
- Ringdahl, E. N., & Pandit, S. (2011). Treatment of knee osteoarthritis. American family physician, 83(11), 1287-1292. https://pubmed.ncbi.nlm.nih.gov/21661710/
- Sibley, J. T. (1985). Weather and arthritis symptoms. The Journal of Rheumatology, 12(4), 707-710. https://europepmc.org/article/med/4057192
- SCHAIBLE, H. G., Ebersberger, A., & Von Banchet, G. S. (2002). Mechanisms of pain in arthritis. Annals of the New York Academy of Sciences, 966(1), 343-354. https://nyaspubs.onlinelibrary.wiley.com/doi/abs/10.1111/j.1749-6632.2002.tb04234.x
- Smolen, J. S., Aletaha, D., Koeller, M., Weisman, M. H., & Emery, P. (2007). New therapies for treatment of rheumatoid arthritis. The lancet, 370(9602), 1861-1874. https://www.sciencedirect.com/science/article/abs/pii/S0140673607607843
- Burmester, G. R., & Pope, J. E. (2017). Novel treatment strategies in rheumatoid arthritis. The Lancet, 389(10086), 2338-2348. https://www.sciencedirect.com/science/article/abs/pii/S0140673617314915
- Majithia, V., & Geraci, S. A. (2007). Rheumatoid arthritis: diagnosis and management. The American journal of medicine, 120(11), 936-939. https://www.sciencedirect.com/science/article/abs/pii/S0002934307003610