- What is lumbar osteoarthritis or inflammation in the back and lower back?
- What are the causes and risk factors for lumbar osteoarthritis?
- Best products for lower back arthritis
- Main symptoms that warn us that we have back arthritis
- What treatments are available to improve the symptoms of osteoarthritis of the lower back?
- Which methods of prevention for lumbar osteoarthritis are the most effective?
The progressive process of lumbar osteoarthritis usually restricts physical movement. In addition, loss of strength and generalised pain in the back can be caused by this type of inflammatory disease. For this reason, it is a good idea to find out what this degenerative disease is all about.
You will find this information in the following paragraphs of this post. We will show you, in detail, how lumbar osteoarthritis can occur and what are the main signs and symptoms that will warn you of the presence of this ailment. We will also talk about the treatments and prevention methods available.
What is lumbar osteoarthritis or inflammation in the back and lower back?
Lumbar osteoarthritis is a degenerative disease that affects the cartilage of the back and lower back, causing pain, swelling and, in some cases, deformity. It is not to be confused with osteoarthritis of the spine or spondyloarthrosis, which includes lumbar osteoarthritis and cervical osteoarthritis.
As a degenerative pathology, osteoarthritis of the lumbar spine cannot be cured and, as time goes by, the disease progresses progressively. It is possible to find cases in which the symptoms are not so severe, but patients suffer episodes of relapse every few years. The pain settles in the lower back and buttocks, although there are patients in whom the ailment is localised in the legs.
What are the causes and risk factors for lumbar osteoarthritis?
The onset of lumbar osteoarthritis can be caused by various risk factors or be caused by direct causes. We will show you below which external and internal circumstances surrounding the person increase the likelihood of contracting this degenerative disease.
Let's start:
- Congenital malformation in the patient: It is likely that the patient suffers from bony protrusions due to the formation of bone spikes in the vertebrae, this causes the spine not to move correctly which is an important factor for the appearance of lumbar osteoarthritis.
- Bulging discs: The pinched discs and the little space between two vertebrae can cause the synovial capsule to be affected in size, causing the articular cartilage not to work normally. This can also occur with a herniated disc.
- Bone fragility: The presence of degenerative osteoporosis anywhere in the lumbar spine can lead to osteoarthritis of the lower back.
- Immune system disorders: Osteoarthritis can also be caused by deficiencies in the body's protective system. This is because the immune cells attack the tissues in the wrong way, causing wear and tear on the cartilage and a decrease in synovial fluid.
- Genetic factors: osteoarthritis of the lower back is considered a hereditary disease that can be passed down through the parents.
- Body overweight: Obesity is also a very influential cause that must be kept under control because the joints of the spine bear a lot of weight and can crush the discs.
- Lack of physical activity: A sedentary lifestyle can also lead to the appearance of lumbar osteoarthritis, as the muscles and joints do not work properly, which can cause injuries and osteophytes.
- Practice of risky activities: This is the opposite case to the previous point, where excessive sports or forced work can also generate the appearance of lumbar osteoarthritis due to the over-demand that the joints of the spine receive.
- Trauma: Some factors related to blows, breaks or any other type of injury are causal factors to consider when assessing osteoarthritis.
- Age: People over the age of 50, especially women, are more prone to the disease due to wear and tear on the hyaline cartilage.
- Muscle stiffness: The appearance of tension in the muscle-tendon structure is a symptom of this disease. This effect is aggravated in the morning hours.
Best products for lower back arthritis
Bestseller
-
Acupressure Mat and Pillow (Black/Gray)
£44,95 -
Acupressure Mat and Pillow (Green/Navy)
£44,95 -
Acupressure Mat and Pillow (Pink/Bordeaux)
£44,95 -
Acupressure Pillow (Black/Gray)
£21,52 -
Acupressure Pillow (Green/Navy)
£21,52 -
Acupressure Pillow (Pink/Bordeaux)
£21,52 -
Back Support Belt (Black)
£29,95 -
Back Support Belt (Green)
£29,95 -
Back Support Belt (Pink)
£29,95 -
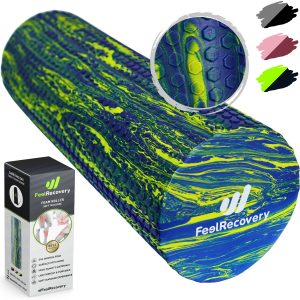
High Density Foam Roller for Muscle (Black/Gray)
£24,95 -
High Density Foam Roller for Muscle (Green/Navy)
£24,95 -
High Density Foam Roller for Muscle (Pink/Bordeaux)
£24,95 -
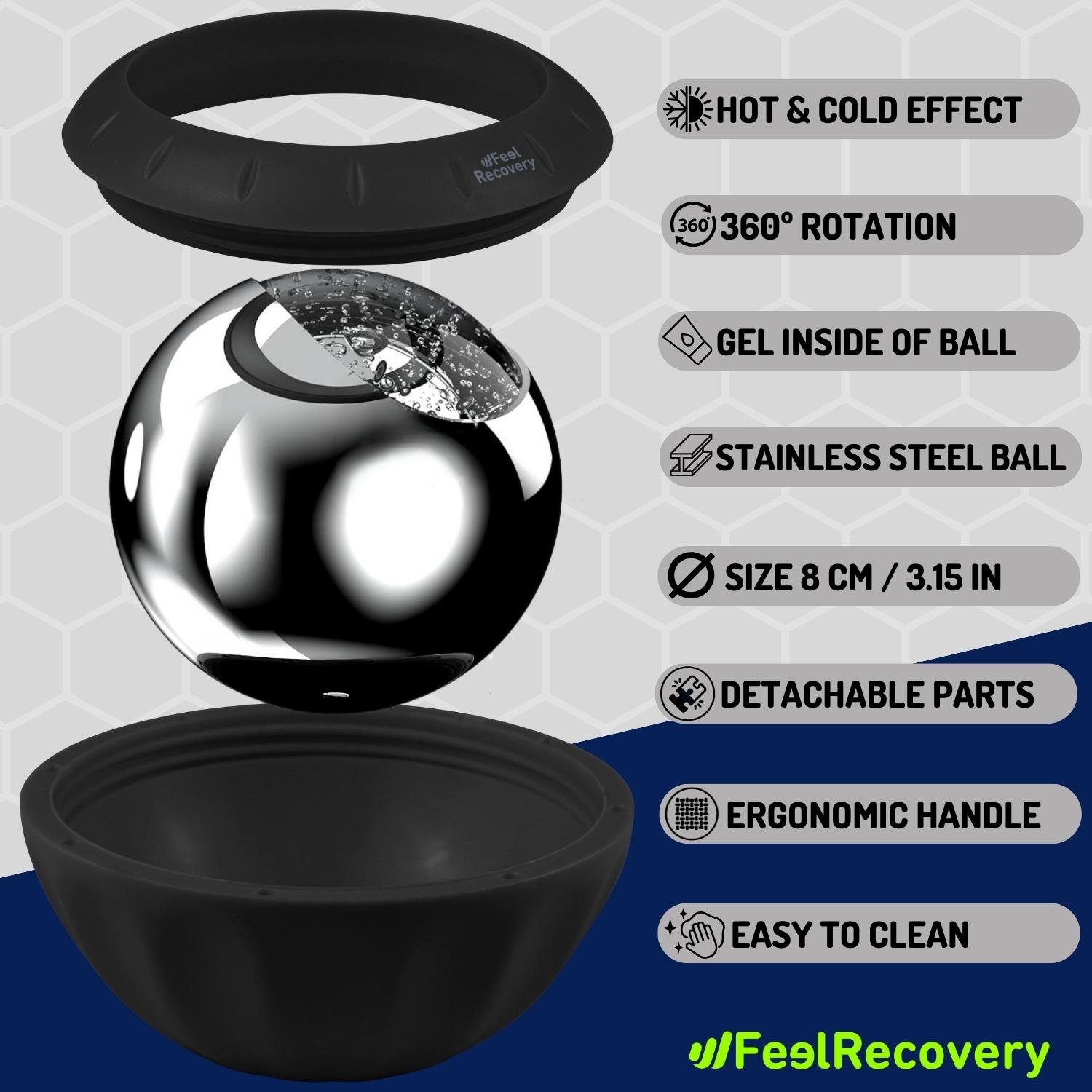
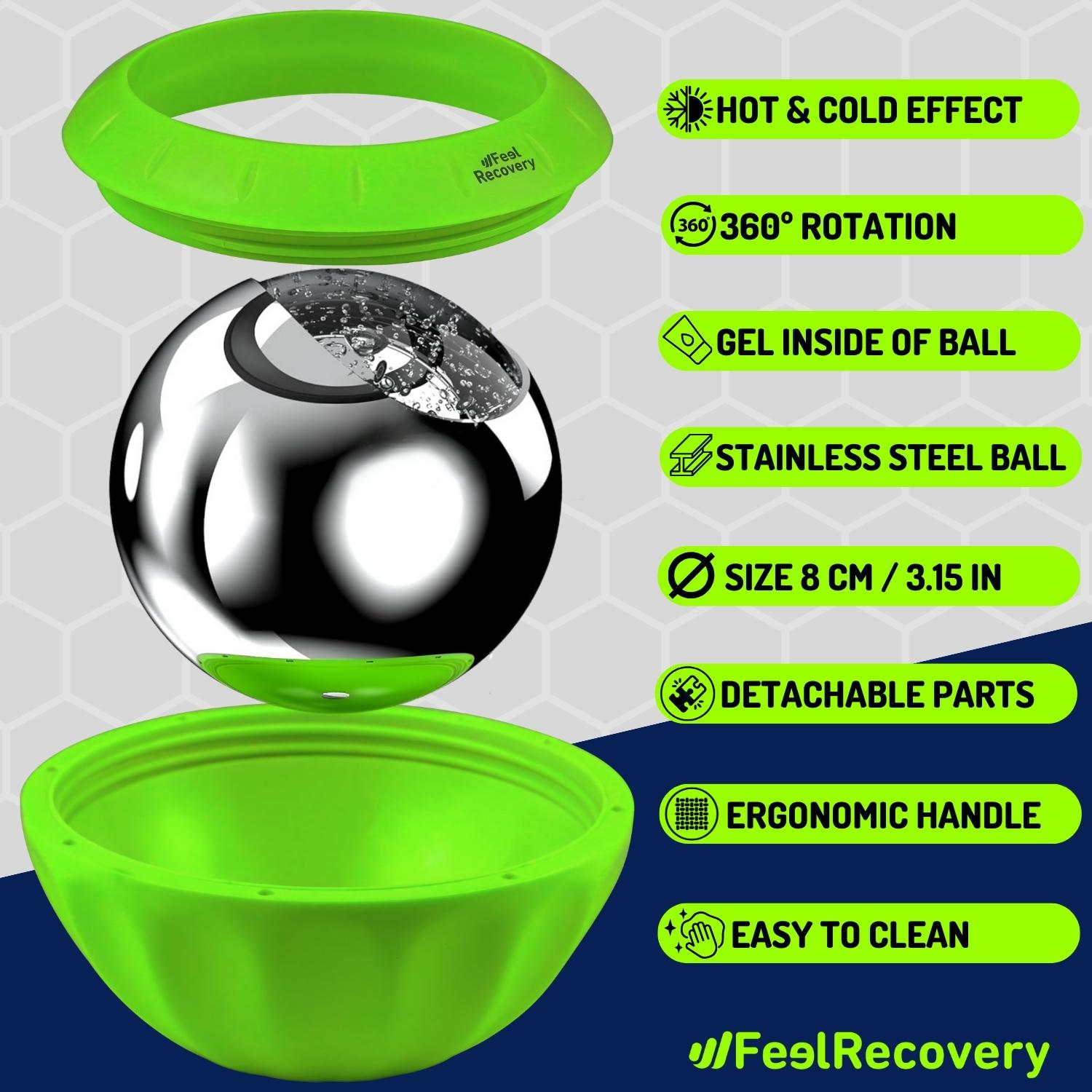
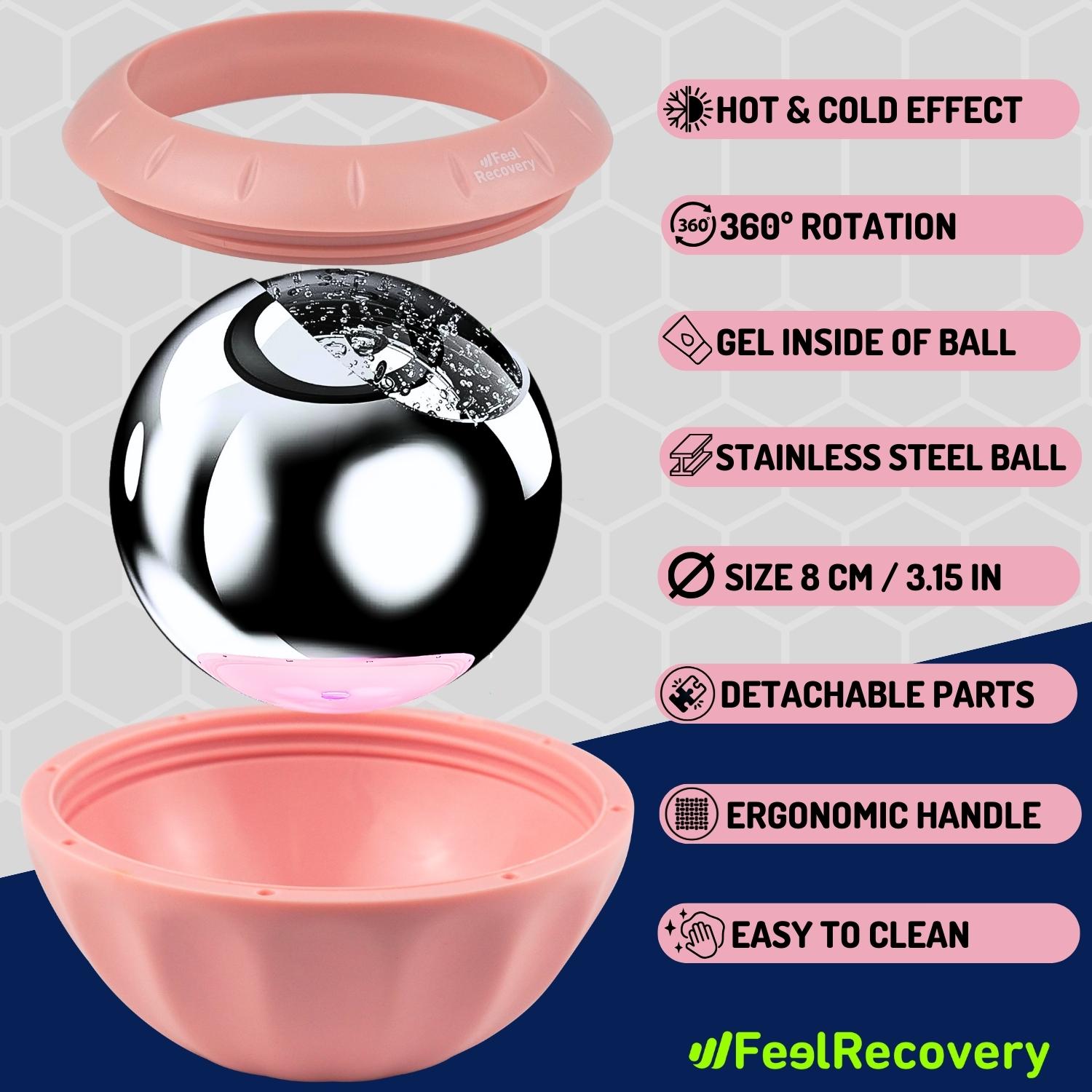
Ice Massage Roller Ball (Black)
£34,95 -
Ice Massage Roller Ball (Green)
£34,95 -
Ice Massage Roller Ball (Pink)
£34,95 -
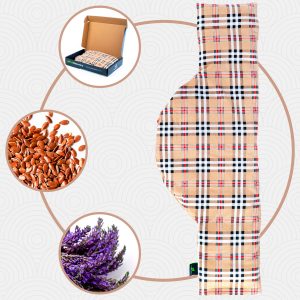
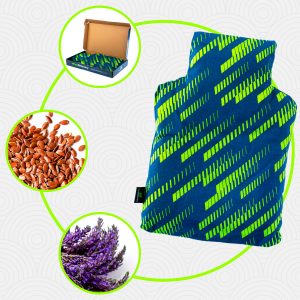
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Hearts)
£25,50 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Oxford)
£25,50 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Sport)
£25,50 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Hearts)
£21,50 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Oxford)
£21,50 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Sport)
£21,50 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£17,50 -
Pack 2 in 1: Foam Roller High + Soft Density (Black/Gray)
£24,95 -
Pack 2 in 1: Foam Roller High + Soft Density (Green/Navy)
£24,95 -
Pack 2 in 1: Foam Roller High + Soft Density (Pink/Bordeaux)
£24,95 -
Sacroiliac Support Belt (Black)
£21,95 -
Sacroiliac Support Belt (Green)
£21,95 -
Sacroiliac Support Belt (Pink)
£21,95 -
Soft Density Foam Roller for Recovery (Black)
£24,95 -
Soft Density Foam Roller for Recovery (Green)
£24,95 -
Soft Density Foam Roller for Recovery (Pink)
£24,95 -
Trigger Point Massage Stick (Black)
£12,95 -
Trigger Point Massage Stick (Green)
£12,95 -
Trigger Point Massage Stick (Pink)
£12,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Hearts)
£17,50 -
Wheat Bag for Microwave Classic Bottle Shaped (Oxford)
£17,50 -
Wheat Bag for Microwave Classic Bottle Shaped (Sport)
£17,50
Main symptoms that warn us that we have back arthritis
It is possible to notice the progression of inflammatory disease in the back by signs and symptoms that appear in the patient's body.
See the list below to find out what these effects are:
- Pain in the back and buttock: This can be caused by muscle stiffness and also by joint defects in the lumbar spine. It is common to find patients suffering from the ailment when they stand up after prolonged sitting or in the first hours after a night's rest.
- Pain in the lower limbs: In some cases there may be pain in the legs and when the disease is advanced it is possible to find patients with little strength in the lower limbs.
- Lack of mobility to perform daily tasks: e.g. bending, dressing and grooming properly.
- Presence of paraesthesia or tingling sensation in the affected areas.
- Swelling and redness in the lower back due to poor blood circulation.
- Stiffness in the lumbar spine caused by contracted muscles that the patient involuntarily tightens due to stress.
- Osteophytes, bone spurs or bone spikes: This can also cause the spine to become misaligned with the sacrum and head.
- Difficulty walking upright: Patients with lumbar osteoarthritis may have trouble straightening the spine and walking properly due to the presence of bone spurs or disc weakness.
- Frequent sciatica: If the nerve roots of the spinal cord have little space within the lumbar spine, the patient with low back osteoarthritis may suffer from this type of pain.
What treatments are available to improve the symptoms of osteoarthritis of the lower back?
In order for the disease to go into remission or for the symptoms to disappear for a while, it is necessary to implement treatments that help to improve the quality of life of the patient with low back osteoarthritis. For this reason, we will show you in the following paragraphs the most effective rehabilitation treatments currently available.
Take a look:
Alternative and complementary therapies
The alternative and complementary therapies that can be used to treat the degenerative process of osteoarthritis of the lower back are:
- Heat and cold therapy: both heat and cold have healing properties that work on the lumbar vertebrae, causing the interapophyseal joints and the entire vertebral body to deflate and widen the space for the intervertebral disc to open better. Hot and cold water bags are used and placed on the affected surface, although it is also possible to find gels and electric blankets that generate the desired temperature. The application cannot exceed 20 minutes and should begin with thermotherapy.
- Compression therapy: in this type of treatment, compresses are used to restrict the movements of the lumbar spine, allowing the vertebral body to be as expanded as possible so that the interapophyseal joint and the disc are lubricated by synovial fluid and thus improve the cushioning of back movements. Compression bands, bandages and back braces supports are used to keep the lumbar position fixed. This therapy may only be carried out by a medical specialist.
- Massage therapy: Massages on the lower back help the patient to relax the tissues in the affected area and thus decompress the space so that the joint capsule with synovial fluid has a greater opening and prevents the discs and bones of the spine from rubbing against each other. This also helps the patient's psychological harmony to cope better with the ailments of the disease.
- Acupressure therapy: it is possible to apply massages generated by the palms of the hand and the pressure of the fingers to specific areas of the body. This is an oriental therapy widely used in China for hundreds of years and is similar to acupuncture, except that no needles are used. The main objective of this technique is to stimulate the nervous system so that, by means of sensory connections, it allows the patient's body to relax in order to obtain a better posture and thus make the lumbar vertebrae give more space to the interapophyseal joints.
- Thermotherapy: this medical treatment applies heat by means of gels, hot water or electric blankets. In this way it is possible to stimulate the dilator vessels so that blood flow can reach the affected area, reducing pain and inflammation. Thermotherapy improves the patient's quality of life, but it is necessary to consult a doctor before choosing this type of rehabilitation method.
- Natural remedies using plants: natural plants and herbs are alternatives that can be taken into account in this lumbar ailment. This involves applying different preparations through baths or infusions for the patient to apply to increase muscle relaxation and reduce inflammation in the lower back. Boldo, chamomile, rosemary and willow, among other herbs, are used in this therapy.
- Ultrasound: in this therapy, electronic devices are used that emit sounds at a high frequency, achieving the heat to reach the lumbar area internally, without the patient feeling the effects on the epidermis. This helps the tissue cells of the interapophyseal joints and intervertebral discs to stop the process of erosion of the hyaline articular cartilage, thus improving lubrication in the lumbar spine. It also helps to reduce inflammation and pain.
- Meditation and relaxation: through breathing techniques and positive thoughts it is possible to find a mental balance in the patient. This is the main objective of meditation and relaxation therapy. To put these exercises into practice, it is necessary for the person to know about the disease and the alterations it causes in their body. This helps to reduce stress levels and control the patient's emotions.
- Aromatherapy: different oils are used in this treatment to help reduce the patient's stress level and increase relaxation in the lower back. For this it is necessary to apply the aromatic solutions in cloths or in devices that emit the smell to reduce the anxiety of the person. It can be applied with different substances, but among the most popular are ginger, citrus fruits and mint.
- Acupuncture: what is sought in acupuncture is that the patient relaxes mentally and physically to reduce the pain in the back and does not affect the functioning of the discs or the intervertebral joints. This is done through impulses that are emitted to the nervous system so that the brain does not receive pain signals. In addition, it is possible to use different techniques of this Chinese medicine, in which electronic signals can be added to help generate heat.
- Biofeedback: this type of treatment is nothing more than letting the patient know how his or her body is reacting to the disease. For this reason, the person is connected to different medical equipment that helps to provide values on blood pressure and heart rate, among other things. Two different moments are compared, when the patient is calm and every time he/she gets nervous because of the pain.
- Healthy lifestyle habits: it is important that the patient not only takes medical and complementary treatments such as meditation or physiotherapy, but it is also necessary that the patient takes this degenerative disease seriously and re-educates his or her lifestyle habits so that they become healthier. For this it is important to visit the doctor who will include exercises, diets and recommend postures so that the lumbar region is not stressed when carrying out daily tasks.
Food supplements
The presentation of food supplements that you can find on the market is based on powders, syrups, liquids and tablets. The dosage and type of supplement must be prescribed by a nutritionist or specialised doctor. Practising this therapy without medical supervision can have the opposite effect, aggravating the symptoms of lumbar osteoarthritis.
In addition to minerals and salts, vitamins and proteins, these supplements incorporate components that are present in the articular hyaline cartilage. In other words, collagen, chondroitin sulphate, glucosamine and hyaluronic acid can be found to improve symptoms.
Physiotherapy treatments
There are different types of physiotherapy that can be applied by the practitioner. Some kinds of this therapy are related to repetitive and short time exercises, while in other techniques the presence of light is added to increase the positive effects on the tissues.
In this way it is possible to reduce muscular tension, improve the opening of the synovial cavity and provoke a feeling of well-being in the patient. This therapy is generally recommended in cases where the disease has a mild to medium degree of progression.
Medications
The drugs used in this type of therapy are based on opioid analgesics and non-steroidal anti-inflammatory drugs. Although it is also possible to find immune cell inhibitors because that disease can be considered as autoimmune.
It should be noted that the implementation of this treatment must be prescribed by a doctor, so it is never advisable to self-medicate. This could lead to serious consequences and impair the patient's symptoms.
Surgery
Although minimally invasive techniques such as injectable treatments and small incisions are available, surgical therapy is usually necessary when the disease has advanced significantly. The treatments used in surgery are based on the removal of bone remnants and the incorporation of lumbar disc prostheses. Arthroscopy is the most commonly used surgical practice.
Which methods of prevention for lumbar osteoarthritis are the most effective?
See below all the prevention methods recommended by experts that you should take into account so that lumbar osteoarthritis does not appear in your body:
- Practise sports or light physical activity: Don't forget that walking, swimming, cycling and low-impact physical exercise help to keep the lumbar vertebrae healthy. For this reason, it is advisable to consult your doctor about the type of activity you can do and the time required for each practice.
- Check your weight regularly: Obesity and excess weight are determining causes of the appearance of osteoarthritis in the lower back; therefore, it is necessary to maintain your ideal weight so as not to overload the lumbar area.
- Avoid heavy lifting: Heavy items can cause serious injury to the lower back, so it is advisable to avoid these kinds of tasks. But in case you have to do them due to the type of work you have to do, you will have to use all the safety elements.
- Always look for the best posture: Sitting with your back supported, lifting things from the floor and walking in the correct way are some techniques that you should incorporate into your daily actions. This will help the hyaline cartilage not to wear out and the joint to work properly.
- Don't drink alcohol or smoke: These types of addictions are not only harmful to the liver and lung tissues but can also lead to osteoporosis in the bones.
- Try to eat foods rich in vitamins D and Omega 3: Vegetables, fish and legumes will provide a balanced diet that will benefit you in combating this joint ailment.
- Choose hard or semi-hard beds to sleep on: This will help to improve the position of the spine when resting.
References
- Flor, H., & Turk, D. C. (1988). Chronic back pain and rheumatoid arthritis: predicting pain and disability from cognitive variables. Journal of behavioral medicine, 11(3), 251-265. https://link.springer.com/article/10.1007/BF00844431
- Helliwell, P. S., Zebouni, L. N. P., Porter, G., & Wright, V. (1993). A clinical and radiological study of back pain in rheumatoid arthritis. Rheumatology, 32(3), 216-221. https://academic.oup.com/rheumatology/article-abstract/32/3/216/1782050
- Keogh, A., Tully, M. A., Matthews, J., & Hurley, D. A. (2015). A review of behaviour change theories and techniques used in group based self-management programmes for chronic low back pain and arthritis. Manual therapy, 20(6), 727-735. https://www.sciencedirect.com/science/article/abs/pii/S1356689X15000673
- Chilibeck, P. D., Vatanparast, H., Cornish, S. M., Abeysekara, S., & Charlesworth, S. (2011). Evidence-based risk assessment and recommendations for physical activity: arthritis, osteoporosis, and low back pain. Applied Physiology, Nutrition, and Metabolism, 36(S1), S49-S79. https://cdnsciencepub.com/doi/full/10.1139/h11-037
- Caporali, R., & Smolen, J. S. (2018). Back to the future: forget ultrasound and focus on clinical assessment in rheumatoid arthritis management. Annals of the Rheumatic Diseases, 77(1), 18-20. https://ard.bmj.com/content/77/1/18.abstract
- Aletaha, D., & Smolen, J. S. (2018). Diagnosis and management of rheumatoid arthritis: a review. Jama, 320(13), 1360-1372. https://jamanetwork.com/journals/jama/article-abstract/2705192
- Firestein, G. S. (2003). Evolving concepts of rheumatoid arthritis. Nature, 423(6937), 356-361. https://www.nature.com/articles/nature01661
- Meenan, R. F., Gertman, P. M., & Mason, J. H. (1980). Measuring health status in arthritis. Arthritis & Rheumatism, 23(2), 146-152. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780230203
- Fries, J. F., Spitz, P., Kraines, R. G., & Holman, H. R. (1980). Measurement of patient outcome in arthritis. Arthritis & Rheumatism, 23(2), 137-145. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780230202
- McInnes, I. B., & Schett, G. (2011). The pathogenesis of rheumatoid arthritis. New England Journal of Medicine, 365(23), 2205-2219. https://www.nejm.org/doi/full/10.1056/NEJMra1004965