- Definition: What are bone dislocations?
- What are the most common types of joints dislocations?
- Best joint dislocations products
- What are the causes and risk factors for dislocation?
- Main signs and symptoms that warn us of a dislocated joint
- What first aid methods are available to treat a joint dislocation?
- What are the most effective prevention methods to avoid a dislocated bone?
- F.A.Q: Frequently asked questions
There are a large number of joint injuries that can occur in the human body, with dislocations being the most recurrent bone contusions in these anatomical areas. A dislocated joint causes the patient pain, immobility, swelling and joint deformity.
As this important bone slippage is very recurrent nowadays, we invite you to read about what a dislocation is all about. We will show you what types of dislocations there are and what are the risk factors that cause this ailment. You will also learn the main symptoms of a dislocated joint and how to help someone with a dislocation.
Definition: What are bone dislocations?
A dislocation is a type of musculoskeletal injury that occurs when two bones in the same joint are partially or completely separated (if the latter situation occurs, it is called a subluxation). If the bone passes through the skin, it is called an external or exposed dislocation, otherwise it is known as a closed dislocation.
To reduce and align the dislocation, it must be treated by the physician with mechanical treatments or special surgeries, although in some patients, the injury goes into natural remission. Among the most recurrent symptoms are pain, internal deformity and joint swelling.
What are the most common types of joints dislocations?
In addition to the classification of open or closed dislocations, they can also be classified according to other parameters. Take a look.
According to the type of dislocation
If the origin of the pathology is taken into account a dislocation can be:
- Incomplete or subluxated dislocation: This injury occurs when there is a partial separation of the bone taking into account its diameter in relation to its axis.
- Dislocation by inflection: This pathology occurs when the separated bone is in an angular position, breaking its convexity or concavity.
- Traumatic: The degree of injury in this condition is severe. It consists of the separation of two diaphyseal bones (in some cases it is accompanied by the breakage of the other bone tissue in the joint). It is commonly found in the hips, arms and knees.
- With trabecular crushing: This is a type of injury that consists of the separation of the surfaces of the spongy and short bones, generating a prominent deformity in the contour of these tissues.
- Dislocation of the articular impeller or "Bankart's lesion": This dislocation occurs when there is an abnormal movement between the diaphysis of one bone and the spongy metaphysis of another. It is commonly found in the head of the humerus and in the lower part of the labrum of the scapula.
- Complete dislocation: This is the total separation between two bones, with some of the bony tissues remaining perpendicular or oblique in relation to the longitudinal axis of the bone.
- Spiroid fracture: This type of injury occurs when there is a twist between two long bones, usually caused by a fracture.
According to the type of recurrence
If the patient's history is taken into account, dislocations can be classified as follows:
- Habitual: Dislocations of this type occur when they are caused by a previous joint disease (arthritis, osteoporosis, etc.) in a trauma patient.
- Recurrent: These are injuries that occur in articular bodies that have already suffered a dislocation.
- Acute dislocations: This type of condition occurs when there is no previous history of dislocation in the joint. The causes can be varied, but the most common are blows and traumatisms.
- Chronic: Also known as inveterate dislocation. This type is caused by failure of a previous dislocation to heal or reduce properly, which prevents the bones from returning to their normal position.
According to the joint affected
On the other hand, a dislocation can be classified according to the joint affected. See below:
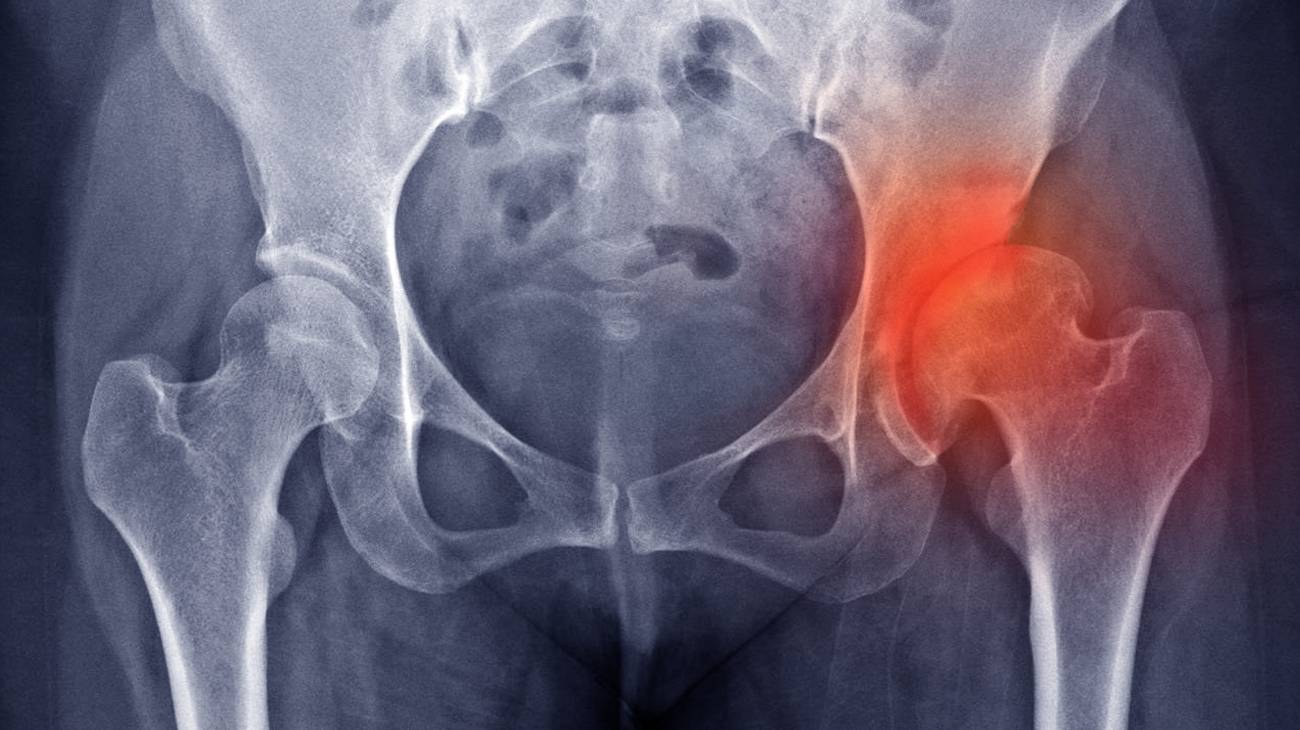
- Hip dislocation: This type of dislocation occurs when there is a separation between the femoral head and the acetabulum of the pelvis. This causes difficulty walking, joint stiffness and severe pain. It can be caused by falls, blows or previous illness.
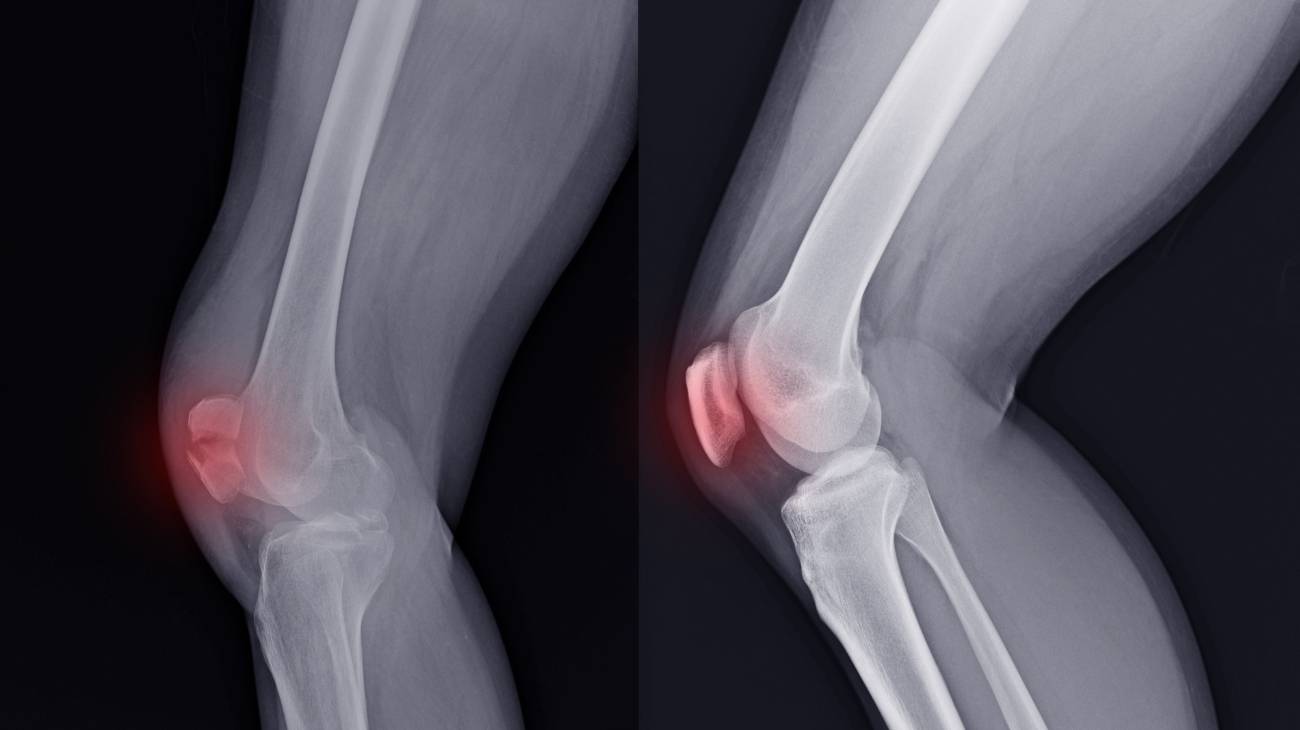
- Elbow dislocation: This is a trauma caused by a lack of contact between the lower area of the humerus with the head of the ulna and the radius. The most common injury is posterior elbow dislocation, in which there is displacement of the lower bones to the distal humerus.
- Shoulder dislocation: This injury occurs when there is a separation between the junction of the humerus, clavicle and scapula. Classification depends on the bones involved. It is possible to find subcoracoid dislocation (humerus - coracoid process of the scapula), subglenoid (humerus - glenoid cavity of the scapula) and subclavicular (humerus - ribs).
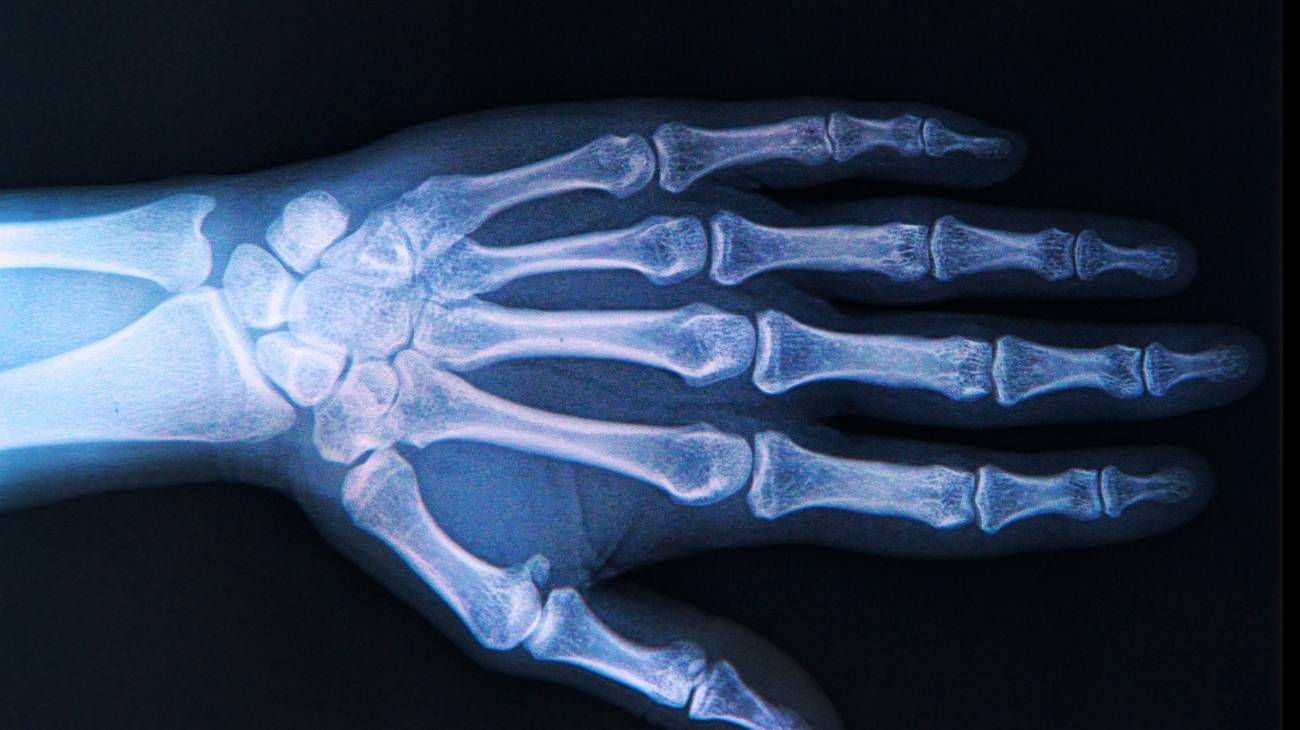
- Wrist dislocation: Among the most common dislocations occurring at the wrist are between the lunate and ulna (lunate dislocation) and between the large bone, scaphoid, 2nd, 3rd and 4th metacarpal, hook, trapezoid and lunate (perilunate dislocation). They are usually caused by falls.
- Knee dislocation: In this case, the injury consists of loss of contact between the condyles of the femur and the glenoid sockets of the tibia. This causes joint stiffness, swelling and permanent pain.
- Patellar dislocation: When there is a displacement of the normal location of this flat, rounded bone, stability is lost due to malpositioning of the joint. For this to occur there may be tears in the collateral and lateral ligaments and in the tendons that derive from the quadriceps femoris or patellar tendons.
Best joint dislocations products
Bestseller
-
2 Ankle Compression Sleeve (Black/Gray)
£17,50 -
2 Ankle Compression Sleeve (Green/Navy)
£17,50 -
2 Ankle Compression Sleeve (Pink/Bordeaux)
£17,50 -
2 Elbow Compression Sleeve (Black/Gray)
£17,50 -
2 Elbow Compression Sleeve (Green/Navy)
£17,50 -
2 Elbow Compression Sleeve (Pink/Bordeaux)
£17,50 -
2 Knee Compression Sleeve (Black/Gray)
£17,50 -
2 Knee Compression Sleeve (Green/Navy)
£17,50 -
2 Knee Compression Sleeve (Pink/Bordeaux)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£17,50 -
Sacroiliac Support Belt (Black)
£21,95 -
Sacroiliac Support Belt (Green)
£21,95 -
Sacroiliac Support Belt (Pink)
£21,95 -
Shoulder Support Brace (Black)
£21,95 -
Shoulder Support Brace (Green)
£21,95 -
Shoulder Support Brace (Pink)
£21,95 -
Wrist Brace (Black/Gray)
£17,50 -
Wrist Brace (Green/Navy)
£17,50 -
Wrist Brace (Pink/Bordeaux)
£17,50
What are the causes and risk factors for dislocation?
There are different risk factors or causes that can lead to dislocation. Here are the most common ones:
- Sudden movements: Any type of movement that is carried out quickly can cause the ligaments that support the bones to be unprepared, thus causing them to shift. The shoulders suffer the most from these factors.
- Lack of previous warm-up: Before doing an activity, it is necessary to warm up the muscle-tendon structure to avoid suffering injuries that can affect the lack of union of two bones. Knees and ankles are prone to injury for this reason.
- Trauma: Blows and falls can cause partial or total displacement of bones.
- Overweight: The stress placed on joints by obesity increases the likelihood of hip, knee and ankle dislocations.
- Physical inactivity: A sedentary lifestyle or constant lack of activity causes the body to become accustomed to a certain position. If for some reason the patient wishes to perform movements to which he or she is not accustomed, this can lead to dislocation.
- Previous joint diseases: Arthrosis is an important risk factor that can lead to dislocations due to wear and tear of the articular cartilage between the two bones of the joint.
- Age of the patient: While dislocations can occur at any age, it is common to find this type of injury in people who lose muscle strength, resulting in a weakening of the joint area.
- Osteophytes: The appearance of bone spurs or overbones in the joint can increase the risk of displacing bony tissues, causing dislocation by inflection, generated by unnatural leverage.
- Patient predisposition: Many people, due to their own anatomy, are more predisposed to suffer this injury due, in some cases, to the excessive elasticity of the ligaments that cover the joints.
Main signs and symptoms that warn us of a dislocated joint
The signs and symptoms that can warn of the presence of a dislocation in a joint are:
- Reddening: An accumulation of blood is caused in the affected area when there is a dislocation, which leads to the appearance of bruises or reddish-coloured skin.
- Joint stiffness: This is one of the main symptoms of a dislocation due to the inability of the bursae of the joint body to cushion movements.
- Continuous pain: When there is a partial or total displacement of the bones, it presses on the nerve roots, causing immediate pain from the moment of the injury. In some cases it causes headache and dizziness.
- Paresthesia: Numbness and tingling are also notorious symptoms in dislocations. This is caused by a lack of normal blood supply to the affected area.
- Weakness: The lack of contact between the two bones causes the muscles, tendons and ligaments to be out of place to do their job properly. This leads to weakness when carrying out everyday activities.
- Noticeable deformity: The separation of two bones causes very visible nodules or lumps in the injured joint.
- Swelling: Joint swelling is also caused by the accumulation of blood that is sent by the autoimmune system for immune cells to try to heal the injury.
What first aid methods are available to treat a joint dislocation?
It is important to clarify that not all emergency cases are the same. If there is severe polytrauma caused by a traffic accident or a fall from a considerable height, it is advisable to call a medical emergency so as not to cause other injuries.
But if you are dealing with a milder situation, you should perform the following first aid steps on the trauma patient:
- Immobilise the joint for transfer: The purpose of this task should not be lost, as it is the medical care of the trauma patient. For this reason, the joint can be total or partial, the latter being recommended, as no special splints or compressive clothing are used.
- Fixing the joint body: A clean bandage should be used to support both parts of the joint as well as possible (with adequate pressure). It is advisable to use a stretcher (or a surface as flat and sturdy as possible, e.g. a door) if the injury is on the lower limbs in order to achieve absolute rest of the joint.
- Apply cold to the affected area: Cryotherapy is a non-invasive treatment that is very important for reducing pain and inflammation because it stimulates blood flow. Ice packs or cold gel balls can be used to provide an analgesic effect.
- Transfer to a medical care centre: It is important to accompany the person at all times, especially when the doctor inquires about the causes that injured the joint and risk factors that the patient may have.
- Maintain rest at all times: Before and after medical intervention it is important that the affected area is kept immobilised and at absolute rest. This will prevent future injuries and complications because the joint body will not be strained.
It is important to clarify that the application of ointments, ointments and the consumption of drugs before medical diagnosis is not recommended in any situation.
What are the most effective prevention methods to avoid a dislocated bone?
In order to avoid a dislocation between two bones, the following aspects should be taken into account:
- Avoid high-risk activities: Contact sports and manual activities that involve repetitive movements can cause stress on the joints, which will lead to dislocation. If for some reason you decide to do these sports, make sure you wear protective compressive clothing.
- Warm up beforehand: To avoid dislocations, contractures and sprains, it is necessary to practice pre-competitive exercises to get the muscular bone structure used to the activity.
- Try not to make sudden movements: Don't forget that this is one of the main causes of joint injuries.
- If you are going to travel by motorbike or bicycle, avoid falls and try to keep your shoulder, knee and ankle joints especially protected.
- Choose to exercise regularly to avoid sedentary lifestyles and obesity and improve your overall quality of life.
- Incorporate calcium-rich foods into your diet and avoid saturated fats, as well as restricting foods that produce excess uric acid. In this way you will keep your bones and cartilage in perfect condition, avoiding the appearance of microcrystals that can act as a lever between two bones, leading to dislocation.
- Visit your doctor frequently if you have a degenerative bone disease or joint ailment for a more specific diagnosis.
F.A.Q: Frequently asked questions
We will show you below the recurring questions that exist on the subject of dislocations of bones. Have a look:
References
- Beitzel, K., Cote, M. P., Apostolakos, J., Solovyova, O., Judson, C. H., Ziegler, C. G., ... & Mazzocca, A. D. (2013). Current concepts in the treatment of acromioclavicular joint dislocations. Arthroscopy: The Journal of Arthroscopic & Related Surgery, 29(2), 387-397. https://www.sciencedirect.com/science/article/abs/pii/S0749806312018907
- Tauber, M. (2013). Management of acute acromioclavicular joint dislocations: current concepts. Archives of orthopaedic and trauma surgery, 133(7), 985-995. https://link.springer.com/article/10.1007/s00402-013-1748-z
- Tischer, T., Salzmann, G. M., El-Azab, H., Vogt, S., & Imhoff, A. B. (2009). Incidence of associated injuries with acute acromioclavicular joint dislocations types III through V. The American journal of sports medicine, 37(1), 136-139. https://journals.sagepub.com/doi/abs/10.1177/0363546508322891
- Josefsson, P. O., Johnell, O., & Wendeberg, B. (1987). Ligamentous injuries in dislocations of the elbow joint. Clinical Orthopaedics and Related Research®, 221, 221-225. https://journals.lww.com/clinorthop/Abstract/1987/08000/Ligamentous_Injuries_in_Dislocations_of_the_Elbow.27.aspx
- Arntz, C. T., Veith, R. G., & Hansen Jr, S. T. (1988). Fractures and fracture-dislocations of the tarsometatarsal joint. JBJS, 70(2), 173-181. https://journals.lww.com/jbjsjournal/Abstract/1988/70020/Fractures_and_fracture_dislocations_of_the.3.aspx
- Cooper, A. (1851). A Treatise on Dislocations and Fractures of the Joints. Blanchard and Lea. https://books.google.es/books?hl=en&lr=&id=EK99doHVY_AC
- Cotton, F. J. (1924). Dislocations and joint-fractures. Annals of Surgery, 80(2), 286. https://journals.lww.com/annalsofsurgery/Citation/1924/08000/Dislocations_and_Joint_fractures.13.aspx
- Richter, M., Wippermann, B., Krettek, C., Schratt, H. E., Hufner, T., & Thermann, H. (2001). Fractures and fracture dislocations of the midfoot: occurrence, causes and long-term results. Foot & Ankle International, 22(5), 392-398. https://journals.sagepub.com/doi/abs/10.1177/107110070102200506
- AITKEN, A. P., & POULSON, D. (1963). Dislocations of the tarsometatarsal joint. JBJS, 45(2), 246-383. https://journals.lww.com/jbjsjournal/Abstract/1963/45020/Dislocations_of_the_Tarsometatarsal_Joint.3.aspx
- Chen, C. H., Dong, Q. R., Zhou, R. K., Zhen, H. Q., & Jiao, Y. J. (2014). Effects of hook plate on shoulder function after treatment of acromioclavicular joint dislocation. International journal of clinical and experimental medicine, 7(9), 2564. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4211760/