- What is osteoarthritis of the foot or inflammation of the foot joint?
- What are the causes and risk factors for osteoarthritis of the feet?
- Best products for foot arthritis
- Main symptoms that warn us that we have arthritis of the feet
- What treatments are available to improve the symptoms of osteoarthritis in the feet?
- What methods of prevention for osteoarthritis of the feet are the most effective?
Both the muscles and the main ligaments in the foot are affected in their function due to the stiffness caused by osteoarthritis in this area. But this is not the only symptom of this degenerative disease; it is also possible to find swelling and loss of strength.
If you want to know everything about osteoarthritis of the foot and why the patient suffers from stress when suffering from this disease, you need to read on to the end. We will show you in detail the symptoms, the causes of the condition and the treatments available.
What is osteoarthritis of the foot or inflammation of the foot joint?
Osteoarthritis of the feet is a degenerative disease that occurs in the transverse tarsal and subtalar joints, causing erosion of the hyaline cartilage in the body of the joints. Over time, the wear and tear of the cartilage becomes chronic and may even lead to its complete disappearance.
This causes the patient to feel a lot of pain every time he or she wants to load the joint or move the foot. The disease causes swelling and restricts the natural movements of the foot due to stress on the calcaneonavicular, calcaneocuboid and plantar longus ligaments.
What are the causes and risk factors for osteoarthritis of the feet?
The risk factors that can lead to osteoarthritis of the foot and the causes that increase a person's chances of contracting this degenerative disease are as follows:
- Previous trauma: This is one of the most recurrent causes that occur in patients with osteoarthritis of the feet. The most healed breaks or blows suffered by the joints can cause deformations in the synovial capsule, causing the hyaline cartilage to lose its texture and begin to corrode.
- Body overweight: The overload that the feet receive due to excess weight generates that the joints have less space to cushion the movements, causing over time the cartilage to disappear.
- Hereditary factors: Genetics is another point to analyse when presenting patients with this degenerative disease. Between 3 and 5% of people with the disease have parents and siblings with the same symptoms.
- Sedentary lifestyle: Lack of physical activity or spending too much time sitting increases the risk of contracting this degenerative foot disease.
- Joint overload: High-performance athletes or people who work with high demands on the joints of the foot may suffer from overbones that can lead to osteoarthritis.
- Congenital deformities: Bone spurs or osteophytes can occur due to malformations of the foot, which lead to osteoarthritis. An example of this is flat feet.
- Older age: People over the age of 50 are more likely to suffer from this degenerative disease. In addition to this, the likelihood increases in women who are going through menopause.
- Repetitive overloaded foot movements: If you lift heavy things on a permanent basis, you should be aware that this is a risk factor that can increase the likelihood of the onset of osteoarthritis of the foot.
- Previous diseases: Rheumatoid arthritis and osteoporosis are diseases that can lead to osteoarthritis of the feet.
Best products for foot arthritis
Bestseller
-
2 Ankle Compression Sleeve (Black/Gray)
£17,50 -
2 Ankle Compression Sleeve (Green/Navy)
£17,50 -
2 Ankle Compression Sleeve (Pink/Bordeaux)
£17,50 -
Acupressure Mat and Pillow (Black/Gray)
£44,95 -
Acupressure Mat and Pillow (Green/Navy)
£44,95 -
Acupressure Mat and Pillow (Pink/Bordeaux)
£44,95 -
Acupressure Pillow (Black/Gray)
£21,52 -
Acupressure Pillow (Green/Navy)
£21,52 -
Acupressure Pillow (Pink/Bordeaux)
£21,52 -
Foot Massage Roller for Plantar Fasciitis (Black)
£17,50 -
Foot Massage Roller for Plantar Fasciitis (Green)
£17,50 -
Foot Massage Roller for Plantar Fasciitis (Pink)
£17,50 -
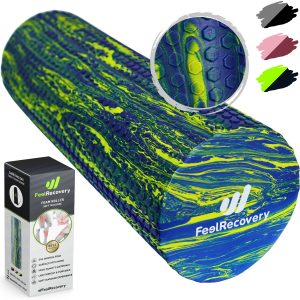
High Density Foam Roller for Muscle (Black/Gray)
£24,95 -
High Density Foam Roller for Muscle (Green/Navy)
£24,95 -
High Density Foam Roller for Muscle (Pink/Bordeaux)
£24,95 -
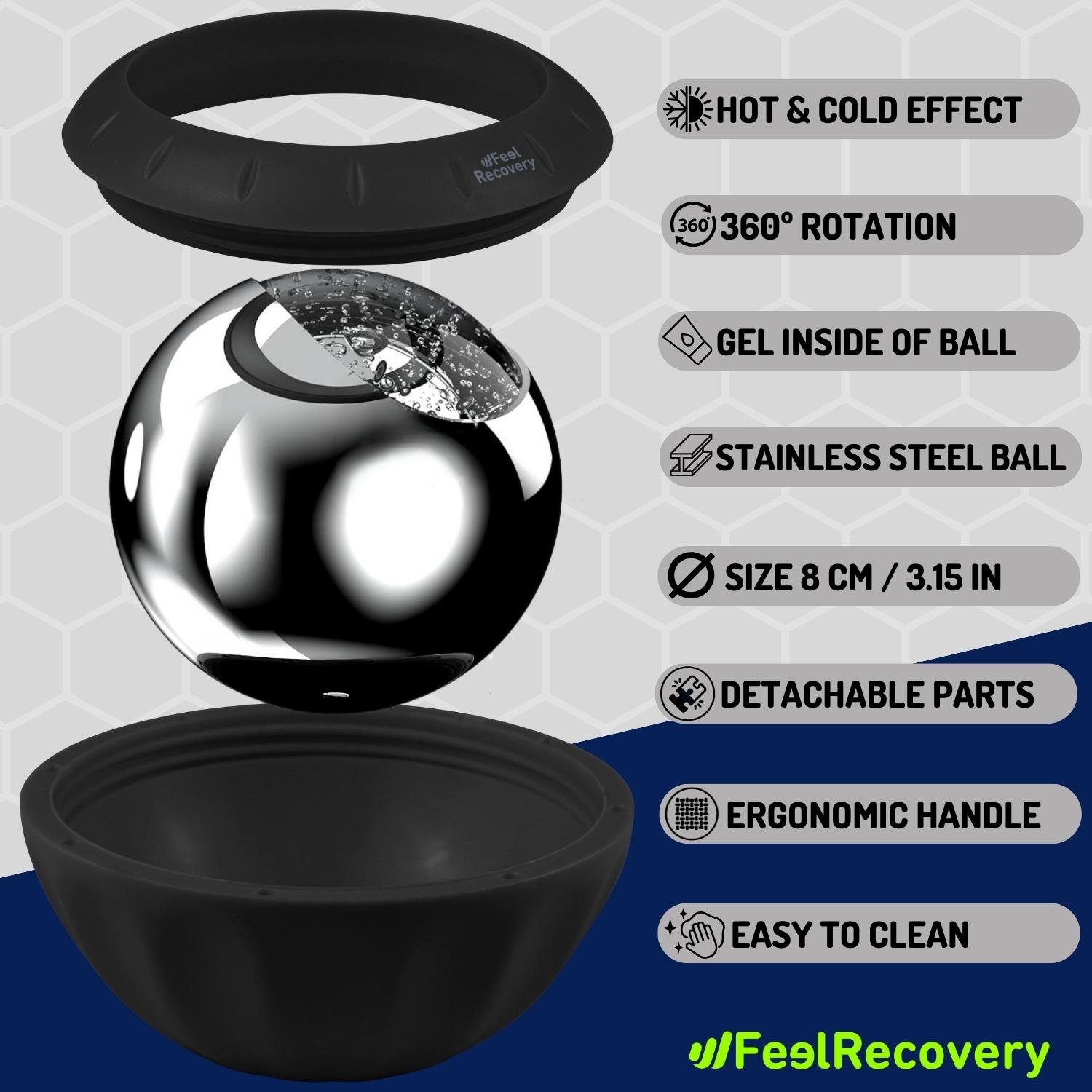
Ice Massage Roller Ball (Black)
£34,95 -
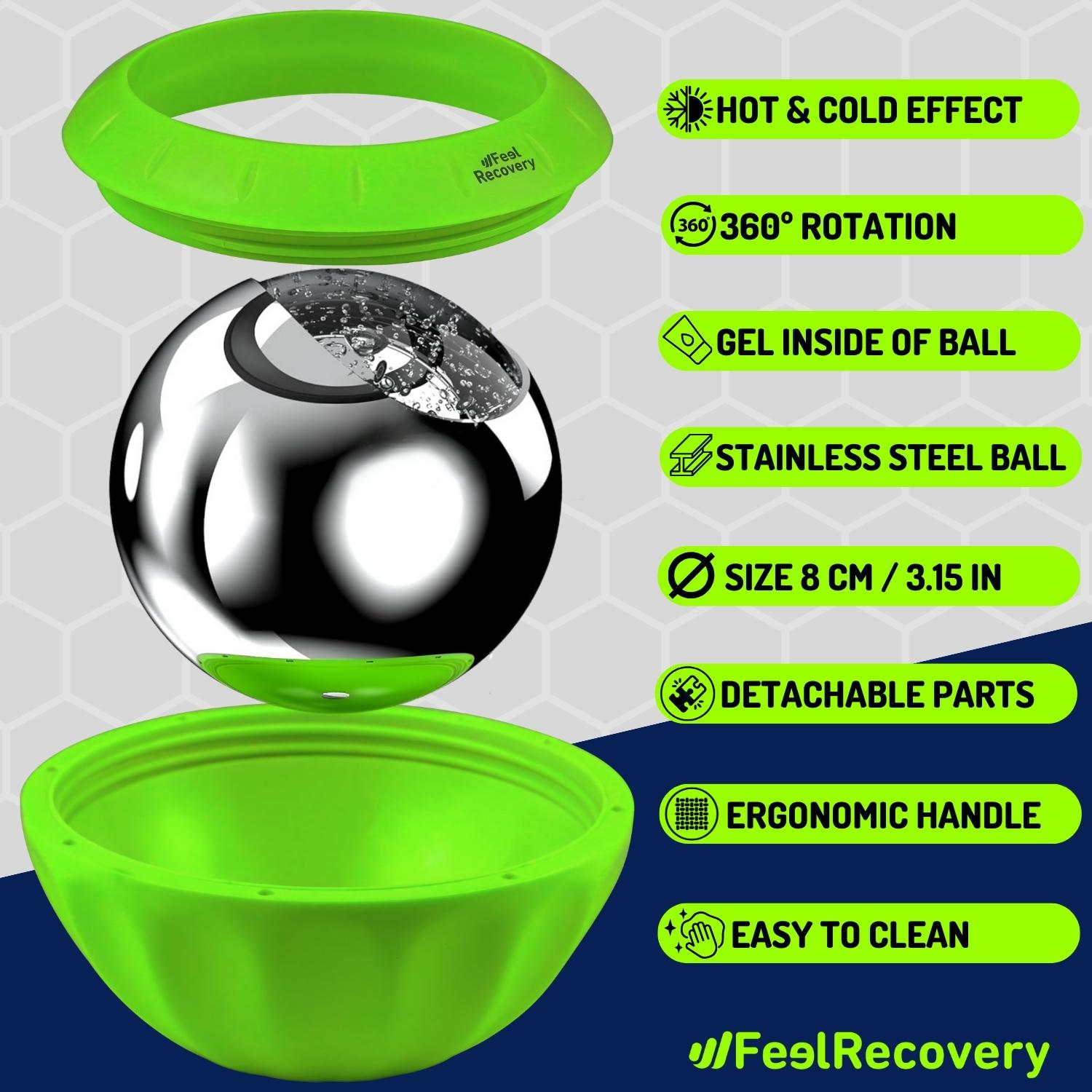
Ice Massage Roller Ball (Green)
£34,95 -
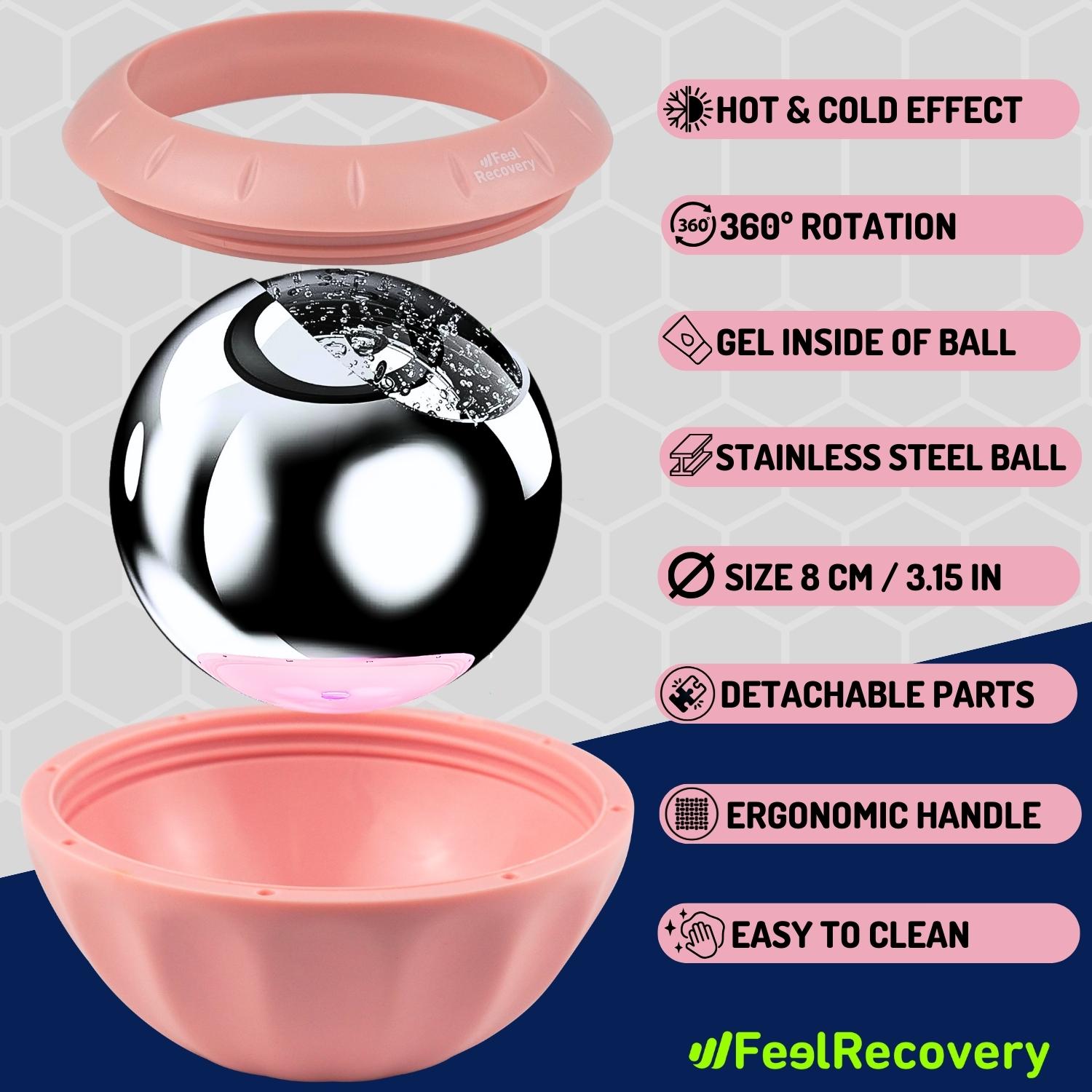
Ice Massage Roller Ball (Pink)
£34,95 -
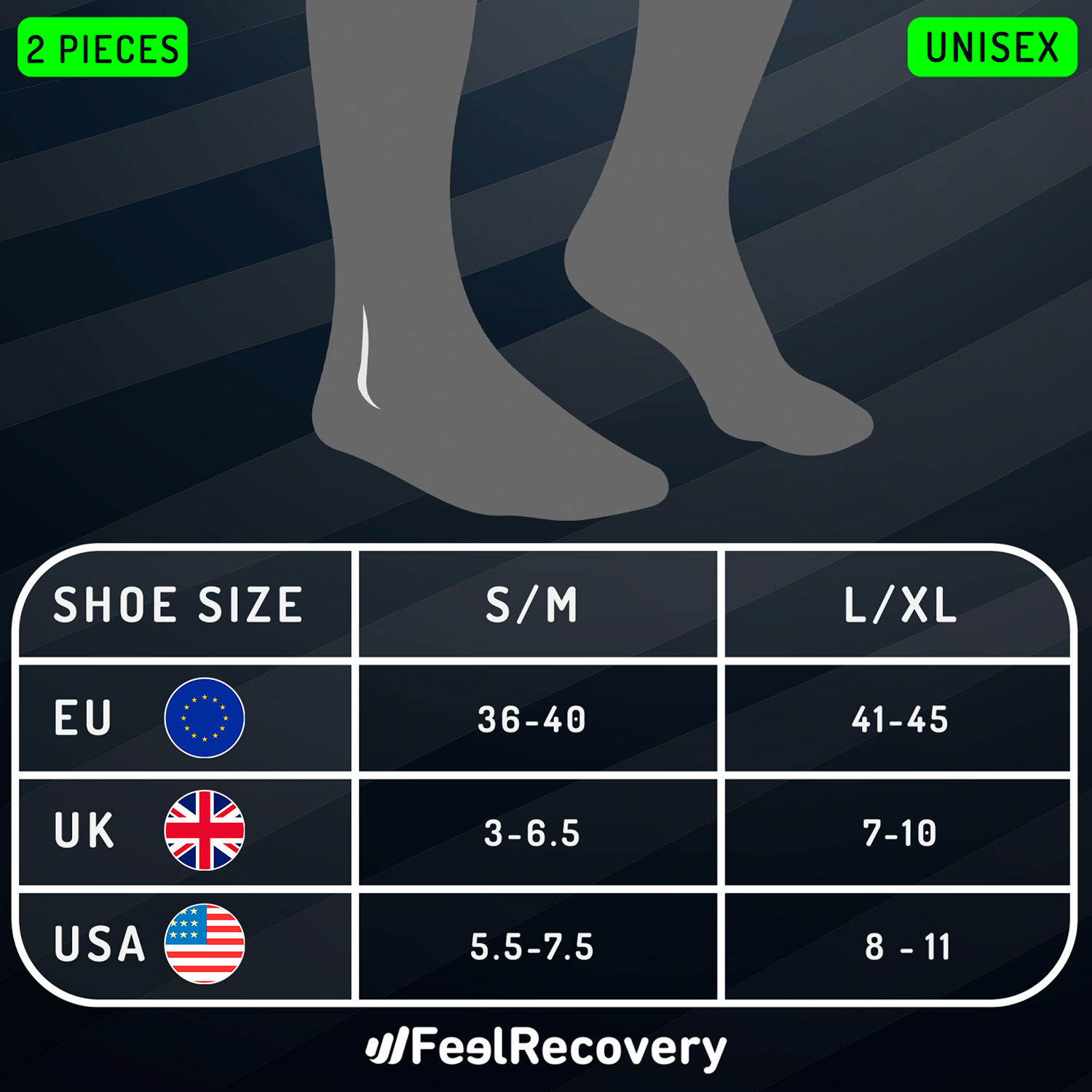
Ice Pack for Foot - Cold Therapy Socks (Black)
£21,95 -
Ice Pack for Foot - Cold Therapy Socks (Green)
£21,95 -
Ice Pack for Foot - Cold Therapy Socks (Pink)
£21,95 -
Microwavable Heated Slippers (Hearts)
£21,50 -
Microwavable Heated Slippers (Oxford)
£21,50 -
Microwavable Heated Slippers (Sport)
£21,50 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£17,50 -
Pack 2 in 1: Foam Roller High + Soft Density (Black/Gray)
£24,95 -
Pack 2 in 1: Foam Roller High + Soft Density (Green/Navy)
£24,95 -
Pack 2 in 1: Foam Roller High + Soft Density (Pink/Bordeaux)
£24,95 -
Soft Density Foam Roller for Recovery (Black)
£24,95 -
Soft Density Foam Roller for Recovery (Green)
£24,95 -
Soft Density Foam Roller for Recovery (Pink)
£24,95 -
Sport Compression Socks (1 Pair) (Black/Gray)
£17,50 -
Sport Compression Socks (1 Pair) (Green/Navy)
£17,50 -
Sport Compression Socks (1 Pair) (Pink/Bordeaux)
£17,50
Main symptoms that warn us that we have arthritis of the feet
Learn about the main signs and symptoms that will help to warn you of the presence of osteoarthritis in the feet:
- Swelling in the subtalar and transverse tarsal joints: Swelling is a very common symptom in this disease, due to the lack of blood circulation and the malfunctioning of the particular cartilage. For this reason, it is necessary to see a doctor urgently if this symptom appears.
- Lack of mobility: Pain and stiffness caused in the foot area are also effects to be taken into account. The musculo-tendinous structure is affected by the lack of stretching and movement due to malfunctioning of the calcaneocuboid, plantar longus and calcaneus navicular ligaments.
- Deformation of the cuboid, metatarsal, cuneiform and navicular bones: This can be caused by the presence of microcrystals in the joint that generate deviations in the bone structure.
- Disproportionately thick nails, reddening of the skin and the presence of calluses: these are some symptoms that may indicate the presence of osteoarthritis in the foot.
- Loss of strength in muscles and tendons: Osteoarthritis causes weakness in the structure that supports the bones and joints of the feet. It is therefore advisable to be on the lookout for this type of symptomatic effect.
What treatments are available to improve the symptoms of osteoarthritis in the feet?
Treatments used by modern medicine to alleviate the symptoms of osteoarthritis in the feet are as follows:
Alternative and complementary therapies
The actions applied in this type of treatment are aimed at reducing the symptoms of osteoarthritis of the feet, thus improving the patient's general well-being and quality of life.
The most commonly used techniques for this degenerative disease are:
- Heat and cold therapy: this is a treatment that takes maximum advantage of the opposite temperatures to improve the revascularisation of the malleolar branches in the joint of the foot. In this way it is possible for both the transverse tarsal and subtalar joints to reduce the swelling of the affected area and improve the tension of the plantar longus, calcaneocuboid and plantar calcaneonavicular ligaments. This allows for better movement of the foot and a much greater sense of well-being. To use thermotherapy and cryotherapy and it is necessary to consult with the doctor, as this application cannot exceed 15 to 20 minutes.
- Compression therapy: the aim of this type of zonal fixation is to prevent the foot from moving so that the subtalar, talocalcaneonavicular and calcaneocuboid joints remain immobile. In this way the forefoot and midfoot will not have the flexibility that allows the muscles and tendons to continue to stretch and generate more inflammation and pain. In this case, ankle braces, special bandages and splints are used according to the patient's situation and the progress of the disease.
- Massage therapy: there are different types of techniques used in this message therapy. It will depend on the level of inflammation, stiffness and pain to choose by rubbing, kneading or compression of the affected area. What is sought with this treatment is to generate heat to obtain the benefits of dilation in the blood vessels, causing analgesic effects that help the brain to better withstand the symptomatology of this degenerative disease.
- Acupressure therapy: this alternative therapy has its origin in China and seeks, by means of pressure exerted by the knuckles, palms and fingers of the hands, to stimulate the bloodstream to generate analgesic effects by releasing endorphins in the organism. It is possible to use this medicine on the foot so that the ligaments considerably improve flexibility and axial movements. This will reduce swelling, redness and pain in the affected area.
- Thermotherapy: can be applied by means of hot water bottles, electric blankets and special heat gels on the feet. This will help to decompress the tension in the muscle-tendon structure causing the ligaments and the transverse tarsal and subtalar joints to be more flexible and not generate pain when walking. This therapy can be accompanied by other treatments such as meditation and relaxation, which will help to increase the patient's sense of well-being.
- Natural remedies using plants: footbaths and infusions can be used to reduce the symptoms of osteoarthritis of the foot. For this it is necessary to make a preparation with medicinal plants that stimulate the energy and generate invigorating effects and help to improve the blood flow. Different types of flowers such as lavender, sage, laurel and mint can be used in this therapy.
- Ultrasound: it is possible to apply sound frequencies exceeding 20 gigahertz to stimulate the nerve branches located in the foot. It also improves the flexibility of the muscles and ligaments between the talus and the navicular, as well as the metatarsals and from the calcaneus to the cuboid. This therapy helps to reduce pain, as the patient indirectly receives internal heat generated by the ultrasound.
- Meditation and relaxation: osteoarthritis of the foot can be treated with complementary therapies such as meditation. In this case it is necessary for the person to reach high levels of relaxation to make the muscles located in the limb lose tension and thus provoke a feeling of wellbeing. On the other hand, meditation through breathing techniques can reduce stress and awaken the strength of the mind to face the degenerative disease.
- Aromatherapy: Scent therapy consists of including aromatic substances in the patient's main treatment. The aim of this rehabilitative method is to reduce stress in the person and to achieve a harmony that increases the patient's sense of wellbeing. This treatment can be accompanied by relaxation techniques and meditation therapies.
- Acupuncture: This Chinese medicine can be used to treat osteoarthritis of the foot, as special needles can be placed at various points on the patient's body to stimulate the nervous system. In this way, the musculature and the short plantar, long plantar and calcaneonavicular ligaments are stretched and the opening of the joints is improved. This increases axial movements and considerably reduces pain and swelling in the affected area.
- Biofeedback: For this rehabilitation method to be successful, it is necessary to show the patient different parameters and values obtained from studies carried out on his or her own body. In this way it is possible to know the heart rate, blood pressure and the level of tension in the muscles when suffering from a pain attack and at times of stress. This re-educates the patient to find an emotional balance in the face of the symptoms of the disease.
- Healthy lifestyle habits: one of the most important risk factors for osteoarthritis of the foot is walking, although it is also common to find patients with obesity. Because of this, it is necessary for the doctor to recommend changes in the patient's lifestyle so that the activities do not damage or injure the affected area. For this reason, it is advisable to consider the permanent incorporation of the practice of healthy exercises, eating healthy, not lifting heavy things that can damage the joints of the foot and also not smoking, among other acts. This will help to reduce the symptoms quickly.
Dietary supplements
This option is based on the inclusion of substances that can be found in the joint, especially in the soft tissues of the cartilage. For this reason, dietary supplements are prescribed to patients to support their diet and improve the symptoms of osteoarthritis.
In this case, hyaluronic acid, selenium, magnesium, glucosamine and chondroitin sulphate are included in capsules, powders or syrups. All these minerals and others are incorporated in different doses, so it is necessary to consult a doctor or nutritionist before taking these supplements.
Physiotherapy treatments
Physiotherapy involves repetitive localised exercises of short duration to stretch the muscles and ligaments in the area. The physiotherapist may include different techniques depending on the progression of the disease. For example, he may opt for the use of temperature, water, laser beams and electricity. With this treatment it is possible to increase the general well-being of the patient, stop or decrease the symptoms of osteoarthritis, especially the pain and inflammation in the musculo-tendinous structure of the foot.
Medications
The pharmacological treatment used in this type of ailment is based on opioid analgesics, e.g. paracetamol. In addition, non-steroidal anti-inflammatory drugs such as acetylsalicylic acid, naproxen and ibuprofen are included in this therapy. In some cases it is possible to find patients who are prescribed immunosuppressants to stop the immune cells from attacking the soft tissues.
You should be aware that self-medication is not at all advisable. This is because it can increase the symptoms and progression of the disease, as well as increasing the likelihood of liver and gastrointestinal damage. For this reason, it is always necessary to visit the doctor to receive the correct dosage and medication, according to each case.
Surgery
Only in very severe cases should surgery be considered to stop and alleviate the symptoms of osteoarthritis of the feet. Arthroplasty is one of the most commonly used practices in this type of ailment, as it allows bone remains to be removed and the state of the joint cartilage to be determined. It is also possible to find patients who have undergone surgery in which surgeons artificially join the joint.
What methods of prevention for osteoarthritis of the feet are the most effective?
Here are the prevention methods you should take into account to avoid osteoarthritis of the feet:
- Wear comfortable shoes: If you need to walk or run and thus demand the joints in your feet, it is advisable to always choose shoes that are appropriate for the activity you want to practise.
- Activate the dilation of the blood vessels: By means of footbaths or baths with warm water and medicinal herbs, you will reduce the chances of the disease appearing because you will improve circulation in the lower limbs.
- Protect your joints: If you are going to lift heavy things, it is advisable that you use special bandages or girdles to immobilise the joints so that they do not suffer injuries due to the effort they can make.
- Do moderate exercise: Don't forget that a sedentary lifestyle and obesity are risk factors that are present in a large proportion of patients with osteoarthritis of the foot. For this reason, walking 30 minutes a day, walking up and down stairs in a controlled and gentle manner or cycling help your body to prevent this degenerative disease.
- Incorporate healthy foods into your diet: You should avoid uric acid and high-fat foods, which can cause microcrystals to lodge in the joints of the foot. Choose foods rich in vitamin D, fibre and Omega 3.
- Try to walk on flat surfaces: This will help you avoid injuries and sprains in your ankles and feet, which could lead to osteoarthritis in the future.
- Massage your feet regularly: Massages and the use of special creams activate the joints and muscles, preventing the development of osteoarthritis.
- At the slightest symptom or sign go to the doctor: If you find deformities or any other characteristic of the presence of the disease you should visit the doctor urgently to prevent the progression of this ailment.
References
- Jaakkola, J. I., & Mann, R. A. (2004). A review of rheumatoid arthritis affecting the foot and ankle. Foot & ankle international, 25(12), 866-874. https://journals.sagepub.com/doi/abs/10.1177/107110070402501205
- Otter, S. J., Lucas, K., Springett, K., Moore, A., Davies, K., Cheek, L., ... & Walker-Bone, K. (2010). Foot pain in rheumatoid arthritis prevalence, risk factors and management: an epidemiological study. Clinical rheumatology, 29, 255-271. https://link.springer.com/article/10.1007/s10067-009-1312-y
- Vidigal, E., Jacoby, R. K., Dixon, A. S., Ratliff, A. H., & Kirkup, J. (1975). The foot in chronic rheumatoid arthritis. Annals of the Rheumatic Diseases, 34(4), 292-297. https://ard.bmj.com/content/34/4/292.short
- Hennessy, K., Woodburn, J., & Steultjens, M. P. (2012). Custom foot orthoses for rheumatoid arthritis: a systematic review. Arthritis care & research, 64(3), 311-320. https://onlinelibrary.wiley.com/doi/abs/10.1002/acr.21559
- Tenten-Diepenmaat, M., van der Leeden, M., Vliet Vlieland, T. P., & Dekker, J. (2018). Multidisciplinary recommendations for diagnosis and treatment of foot problems in people with rheumatoid arthritis. Journal of foot and ankle research, 11(1), 1-13. https://jfootankleres.biomedcentral.com/articles/10.1186/s13047-018-0276-z
- Aletaha, D., & Smolen, J. S. (2018). Diagnosis and management of rheumatoid arthritis: a review. Jama, 320(13), 1360-1372. https://jamanetwork.com/journals/jama/article-abstract/2705192
- Firestein, G. S. (2003). Evolving concepts of rheumatoid arthritis. Nature, 423(6937), 356-361. https://www.nature.com/articles/nature01661
- Meenan, R. F., Gertman, P. M., & Mason, J. H. (1980). Measuring health status in arthritis. Arthritis & Rheumatism, 23(2), 146-152. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780230203
- Fries, J. F., Spitz, P., Kraines, R. G., & Holman, H. R. (1980). Measurement of patient outcome in arthritis. Arthritis & Rheumatism, 23(2), 137-145. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780230202
- McInnes, I. B., & Schett, G. (2011). The pathogenesis of rheumatoid arthritis. New England Journal of Medicine, 365(23), 2205-2219. https://www.nejm.org/doi/full/10.1056/NEJMra1004965