- What is dislocation of the patella joint?
- What are the causes and risk factors for patellar dislocation?
- Best products for kneecap dislocation
- Main signs and symptoms that warn us that we have a dislocation in the patella
- What is the first aid for a dislocated kneecap?
- What are the most effective prevention methods for patellar joint dislocation?
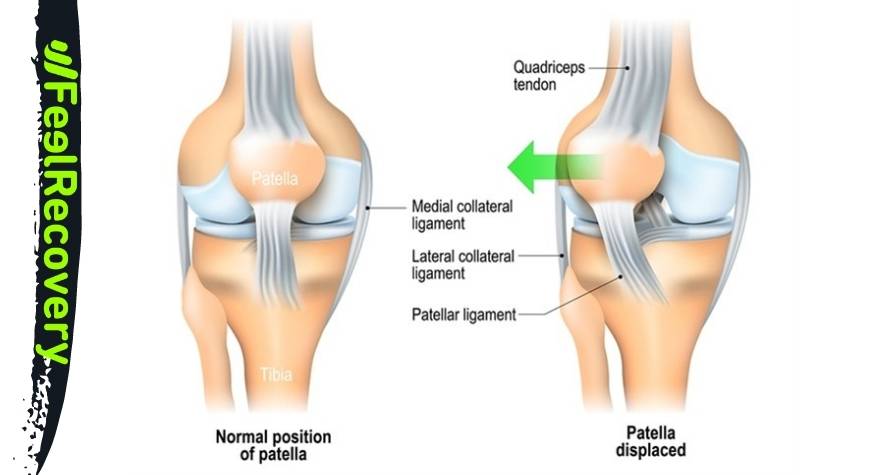
When there is a displacement of the patella from its natural position, this trauma is known as patellar dislocation. This dislocation can be complete or partial depending on the stretching of the quadriceps femoris tendons and the patellar ligament.
We will show you in detail what are the main causes of patellar dislocation and what are the most frequent symptoms of this trauma. Pay attention to the first aid steps that we will invite you to apply to a trauma patient. See below.
What is dislocation of the patella joint?
The patella is usually located almost in the centre of the knee, supported at the anterior superior part by the quadriceps femoris tendon and by the patellar ligament at the other end. In turn, the lateral and medial ligaments provide the force necessary to hold this flat bone in its natural position.
If for some reason these connective tissues become abnormal, the patella moves from its original place. This causes a trauma called patellar dislocation. The traumatized patient should see a doctor immediately for treatment to reduce the dislocated joint. The degree of injury will determine the recovery time, which can be between 6 to 12 weeks and, in very severe cases, up to 10 months.
What are the causes and risk factors for patellar dislocation?
The most common causes of patellar dislocation are as follows:
- Sports injuries: blows suffered when falling or in sudden contact of the leg with other objects or people, can dislodge the location of the kneecap in the knee. Overloading in training is also a risk factor that can lead to dislocation.
- Domestic falls: Falls sustained in the home are also risk factors to consider when preventing patellar dislocation. This is because all the weight of the body is transmitted to the joint at the moment of falling.
- Sedentary lifestyle: It should not be forgotten that the patella is supported, among other ligaments, by the patellar ligament and the quadriceps femoris tendon. If these connective tissues do not work on a regular basis, they will stiffen and under any demand will not stop the patella from moving.
- Sudden movements: Flexion, extension and rotation of the knee are limited by the ligaments and tendons. If for some reason the joint suddenly slips out of place, the kneecap can slip out of place.
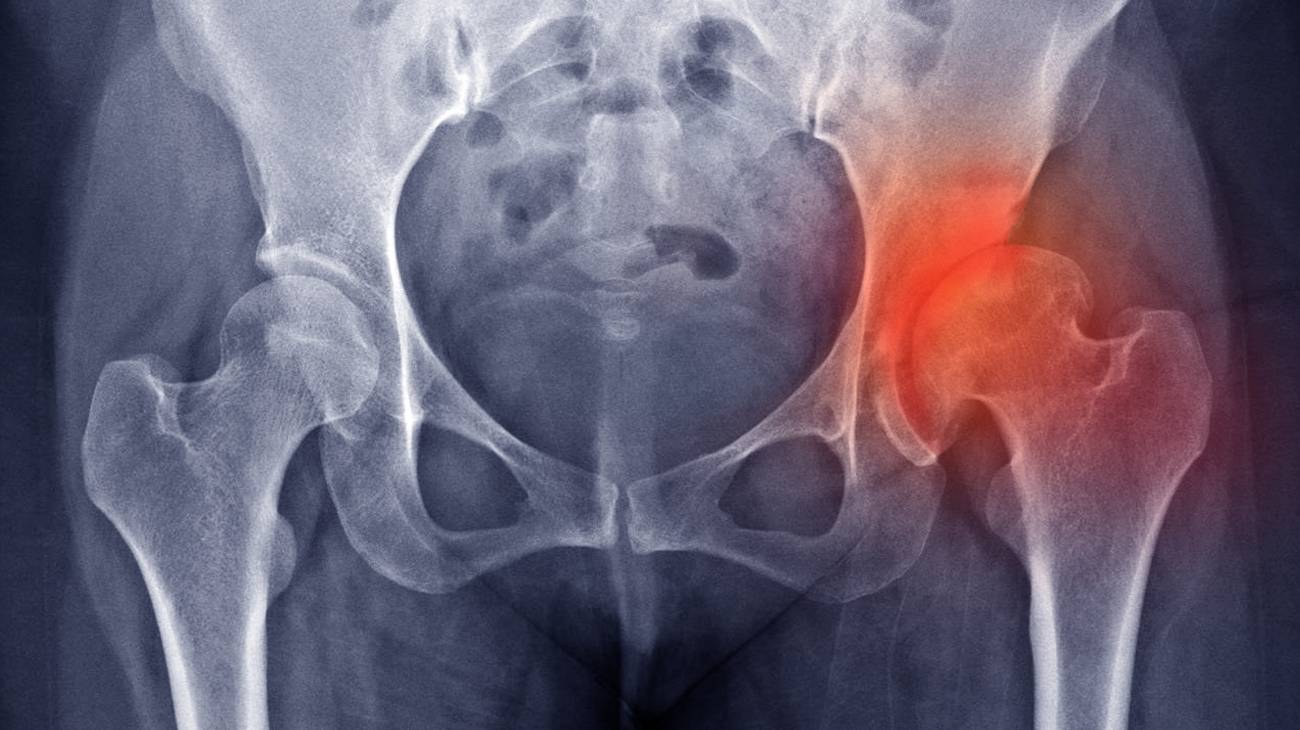
- Bursitis: Inflammation of the patellar bursa is an important cause of dislocation of the patella, which can lead to dislocation of varying degrees of severity.
- Degenerative diseases: Osteoarthritis, osteogenesis and Paget's syndrome are some of the ailments that cause bone weakness, thus increasing the possibility of patellar dislocation.
- Lack of protection: Compressive clothing is ideal for holding the knee joint in place and preventing patellar displacement. Therefore, every time you decide to play a sport or do an activity that puts the kneecap at risk, it is advisable to use a patellar tendonitis strap or a sports knee brace.
- Lack of warm-up: It is important to get the knee used to the action with undemanding exercises. This will help to avoid straining the ligaments and muscles located in this area. If this does not happen, the kneecap is likely to be dislodged.
- Road traffic accidents: Such accidents on the road often cause patellar dislocations due to the strong impact on the knee in the impact.
Best products for kneecap dislocation
Bestseller
-
2 Knee Compression Sleeve (Black/Gray)
£17,50 -
2 Knee Compression Sleeve (Green/Navy)
£17,50 -
2 Knee Compression Sleeve (Pink/Bordeaux)
£17,50 -
2 Patella Knee Strap (Black/Gray)
£12,95 -
2 Patella Knee Strap (Green/Navy)
£12,95 -
2 Patella Knee Strap (Pink/Bordeaux)
£12,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Hearts)
£25,50 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Oxford)
£25,50 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Sport)
£25,50 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£17,50 -
Wheat Bag for Microwave Classic Bottle Shaped (Hearts)
£17,50 -
Wheat Bag for Microwave Classic Bottle Shaped (Oxford)
£17,50 -
Wheat Bag for Microwave Classic Bottle Shaped (Sport)
£17,50
Main signs and symptoms that warn us that we have a dislocation in the patella
A dislocated kneecap can be noticed by the signs:
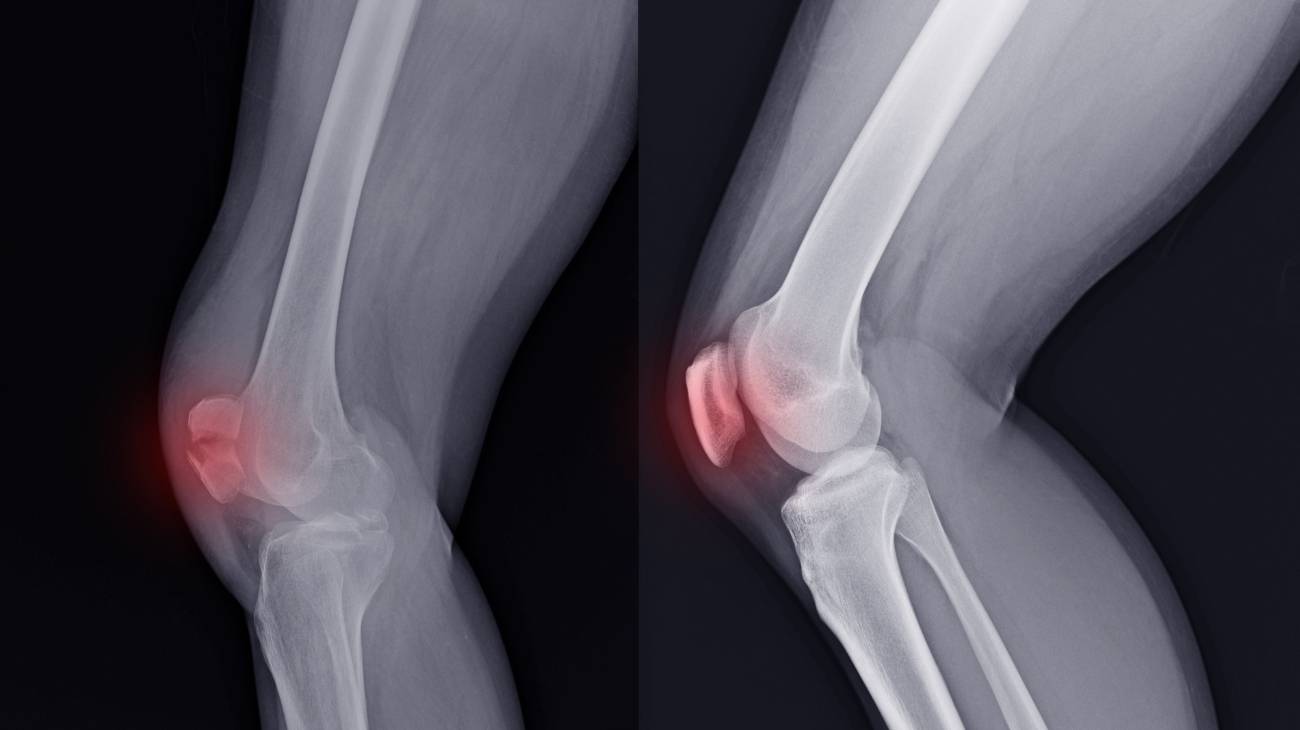
- Joint hypermobility: This is one of the most noticeable symptoms of patellar dislocation. This is generated due to the displacement of the patella from the centre of the knee.
- Inflammation: The quadriceps femoris tendon and patellar ligament often swell when there is a dislocation of the patella. The cruciate and lateral ligaments may also be involved in this trauma.
- Pain on flexion and extension of the knee: The lack of communication between the bones of the joint means that biomechanical movements cannot be performed normally.
- Numbness: posterior numbness in the knee, lack of sensation in the gastrocnemius and soleus are common in this type of patellar trauma.
- Redness and bruising: The autoimmune system causes blood to accumulate in the patella area which cannot be distributed normally. This leads to bruising and redness further away from the knee.
- Loss of body symmetry: If both knees are compared, it is notorious to find a deviation in the joint line, caused by bone separation in the joint
- Bulging: Deformity is another characteristic symptom of patellar dislocation caused by the movement of this bone in the joint.
What is the first aid for a dislocated kneecap?
In the event of a dislocated kneecap , it is possible to help the trauma patient by following protocols that benefit from the symptoms of the situation. It is important to clarify that the steps mentioned below are only applicable to minor trauma, as more serious cases require the intervention of a doctor.
Pay attention to the steps you will need to take to provide first aid to a person with a dislocated patella:
- Protection: Protect your leg and knee. The first thing to do is to clear away all objects that could cause a major injury to this part of the body. If possible, it is advisable to move the patient to a clean and tidy place.
- Rest: Try to rest the patient's knee as much as possible. What you will need to do at this stage is to get the person into a position that does not affect the movement of the knee joint. To do this, it is advisable for the patient to remain still and not do any activity.
- Ice: Apply the principles of cryotherapy. It is advisable to use cold directly on the affected area. This will improve the exchange of nutrients between the blood and the tissues and reduce pain. Cold gel packs can be applied for this purpose.
- Compression: It is important to stimulate blood flow and keep the knee away from vibration and movement. A sports compression knee brace or elastic bandages, among other items, can be used for this step.
- Elevation: Keep the knee elevated above the level of the heart until you transport the patient to a medical facility. This will keep swelling from developing and prevent clots that could lead to thrombosis.
Once the patient is stable , the ideal thing to do is to take him/her to a hospital so that the specialist doctor can perform a technique to reposition the kneecap after the dislocation, this type of technique is usually quite painful and can only be performed by specialised healthcare personnel.
What are the most effective prevention methods for patellar joint dislocation?
Dislocation of the patella can be prevented by using the following methods:
- Common sense: Use common sense to avoid accidents during sport or at work. Do not put yourself or others at risk by making movements that could compromise the patella or other joints.
- Compression clothing: Wearing compression clothing improves the stability of the knee, which helps to prevent dislocation of the knee joint to a large extent. It is also possible to choose compression socks and stockings.
- Deflate the knee: It is important to apply cold after the sports practice if you feel any discomfort. This will help to keep the ligaments and muscles of the joint in good condition. Cold gel packs can be applied to the area.
- Massage the joint: This will also improve the blood circulation of the leg, prevent the occurrence of patellar dislocations. Different massage methods can be chosen, but the most effective are electric massagers and infrared heat massagers.
- Avoid overweight: Excessive body weight decreases the space between the femur and the glenoid cavity, which increases the risk of patellar dislocation. This is caused by weakness of the patellar ligament.
- Don't make sudden movements: The quadriceps femoris tendon and the patellar ligament can rupture if sudden actions or movements are made to which the knee is not accustomed. This will lead to immediate patellar dislocation.
- Try to play sports on a daily basis: This will help to avoid a sedentary lifestyle, which weakens the ligaments that support the kneecap centred on the knee.
- Pay attention: If you suffer from any illness or degenerative disease, it is advisable to pay attention to all the symptoms of a dislocation, as this will help you to avoid it or not to advance in the severity of the traumatism.
- Avoid falls: People who fall on their knees often suffer fractures and patellar dislocations. For this reason, it is advisable to take every precaution to avoid this type of domestic or sporting accident.
- Incorporate vitamins and minerals: A balanced diet accompanied by strategic training will help to improve joint opening and keep the kneecap in its normal position.
References
- Wascher, D. C., Dvirnak, P. C., & DeCoster, T. A. (1997). Knee dislocation: initial assessment and implications for treatment. Journal of orthopaedic trauma, 11(7), 525-529. https://journals.lww.com/jorthotrauma/Abstract/1997/10000/Knee_Dislocation__Initial_Assessment_and.11.aspx
- Howells, N. R., Brunton, L. R., Robinson, J., Porteus, A. J., Eldridge, J. D., & Murray, J. R. (2011). Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury, 42(11), 1198-1204. https://www.sciencedirect.com/science/article/abs/pii/S0020138310007552
- Yeh, W. L., Tu, Y. K., Su, J. Y., & Hsu, R. W. W. (1999). Knee dislocation: treatment of high-velocity knee dislocation. Journal of Trauma and Acute Care Surgery, 46(4), 693-701. https://journals.lww.com/jtrauma/Abstract/1999/04000/Knee_Dislocation__Treatment_of_High_Velocity_Knee.23.aspx
- Seroyer, S. T., Musahl, V., & Harner, C. D. (2008). Management of the acute knee dislocation: the Pittsburgh experience. Injury, 39(7), 710-718. https://www.sciencedirect.com/science/article/abs/pii/S0020138307004858
- SISTO, D. J., & WARREN, R. F. (1985). Complete knee dislocation: a follow-up study of operative treatment. Clinical Orthopaedics and Related Research®, 198, 94-101. https://journals.lww.com/clinorthop/Abstract/1985/09000/Complete_Knee_Dislocation__A_Follow_up_Study_of.14.aspx
- Shelbourne, K. D., Porter, D. A., Clingman, J. A., McCarroll, J. R., & Rettig, A. (1991). Low-velocity knee dislocation. Orthopaedic review, 20(11), 995-1004. https://europepmc.org/article/med/1749665
- Stayner, L. R., & Coen, M. J. (2000). Historic perspectives of treatment algorithms in knee dislocation. Clinics in sports medicine, 19(3), 399-413. https://www.sciencedirect.com/science/article/abs/pii/S0278591905702143
- Arendt, E. A., Fithian, D. C., & Cohen, E. (2002). Current concepts of lateral patella dislocation. Clinics in sports medicine, 21(3), 499-519. https://www.sportsmed.theclinics.com/article/S0278-5919(02)00031-5/fulltext
- Hawkins, R. J., Bell, R. H., & Anisette, G. (1986). Acute patellar dislocations. The American journal of sports medicine, 14(2), 117-120. https://journals.sagepub.com/doi/abs/10.1177/036354658601400204
- Garth JR, W. P., Pomphrey JR, M., & Merrill, K. (1996). Functional treatment of patellar dislocation in an athletic population. The American Journal of Sports Medicine, 24(6), 785-791. https://journals.sagepub.com/doi/abs/10.1177/036354659602400614