- What is bursitis of the knee?
- What are the causes and risk factors for knee bursitis?
- Best products for knee bursitis
- Main symptoms that warn us that we have bursitis in the knees
- What treatments are there to improve the symptoms of knee bursitis?
- What are the most effective prevention methods for knee bursitis?
When there is excess synovial fluid in the bursae located in the knee, there is constant swelling in these bursae. Because of this it is necessary that you know why these symptoms appear and what are the causes that generate this disease in the joint. To do this, you will need to continue reading to the end.
We will explain in detail what bursitis in the knee is and what are the signs that will help you to notice the presence of this ailment. In addition, you will find information about the treatments currently used and a list of preventive methods.
What is bursitis of the knee?
There are three bursae in the knee that act to cushion shocks and soften friction during joint movements. They are located between the patella, the quadriceps femoris tendon, the patellar tendon and the lateral meniscus. The bursae, to do their job in this complex movement of muscles, bones and tendons, contain synovial fluid.
Knee bursitis occurs when there is an excess of synovial fluid in the bursae and the bursae enlarge in size, causing pain and inflammation in the affected area. When any of the bursae become inflamed, the disease is called suprarotellar, prerotellar or infrarutellar bursitis according to the synovial bursa affected.
What are the causes and risk factors for knee bursitis?
Knee bursitis is caused by different causes or risk factors that increase the risk of inflammation of the bursae located near the kneecap.
Pay attention to the following list in which we will show you all these constituent elements:
- Overweight: obesity or excess weight can cause the knee joints to become stiff due to the limited space they have to cushion movement. This causes the bursae located near the kneecap to swell, causing the joint to swell due to excessive synovial fluid in the joint.
- Gout disease: microcrystals are produced due to the abundance of sodium urate found in uric acid, which cannot be properly expelled from the body. This leads to inflammation of the synovial sacs, causing pain due to the excess joint fluid.
- Rheumatoid arthritis: This disease affects the soft tissues of the joints, causing deformation and wear and tear. This worsens the cushioning system of the knee causing irritation of the bursa.
- Congenital diseases: poor formation of the bones, muscles and tendons of the knee caused by birth syndromes lead to asymmetry of the body of the joint. This leads to the synovial bursa being overworked to keep movements protected.
- Spurs: these can be caused not only by congenital diseases but also by the appearance of microcrystals generated by excess uric acid.
- Repetitive movements: the knees are seriously affected when the person performs repetitive movements over a long period of time. This puts stress on the joint structure causing excess synovial fluid in the bursa.
- Fractures and dislocations: previous trauma can affect the normal level of synovial fluid in the bursa. This will benefit the development of inflammation in the synovial bursa, leading to knee bursitis.
- Inappropriate footwear: Shoes and other high-heeled footwear with heels higher than the toes usually put an overload on the knee. This will lead in the short term to the development of bursitis in the area.
- Nutrient-poor diet: It is common for patients to have a diet low in vitamins and minerals that help keep the soft tissues of the joint in perfect condition. For this reason, people who eat a diet rich in meat and fat are more likely to develop knee bursitis.
Best products for knee bursitis
Bestseller
-
2 Knee Compression Sleeve (Black/Gray)
£17,50 -
2 Knee Compression Sleeve (Green/Navy)
£17,50 -
2 Knee Compression Sleeve (Pink/Bordeaux)
£17,50 -
2 Patella Knee Strap (Black/Gray)
£12,95 -
2 Patella Knee Strap (Green/Navy)
£12,95 -
2 Patella Knee Strap (Pink/Bordeaux)
£12,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Hearts)
£25,50 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Oxford)
£25,50 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Sport)
£25,50 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£17,50 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£17,50 -
Wheat Bag for Microwave Classic Bottle Shaped (Hearts)
£17,50 -
Wheat Bag for Microwave Classic Bottle Shaped (Oxford)
£17,50 -
Wheat Bag for Microwave Classic Bottle Shaped (Sport)
£17,50
Main symptoms that warn us that we have bursitis in the knees
In knee bursitis it is possible to find certain signs that announce the presence of this disease. Because of this we will introduce you to the signs and symptoms of this ailment:
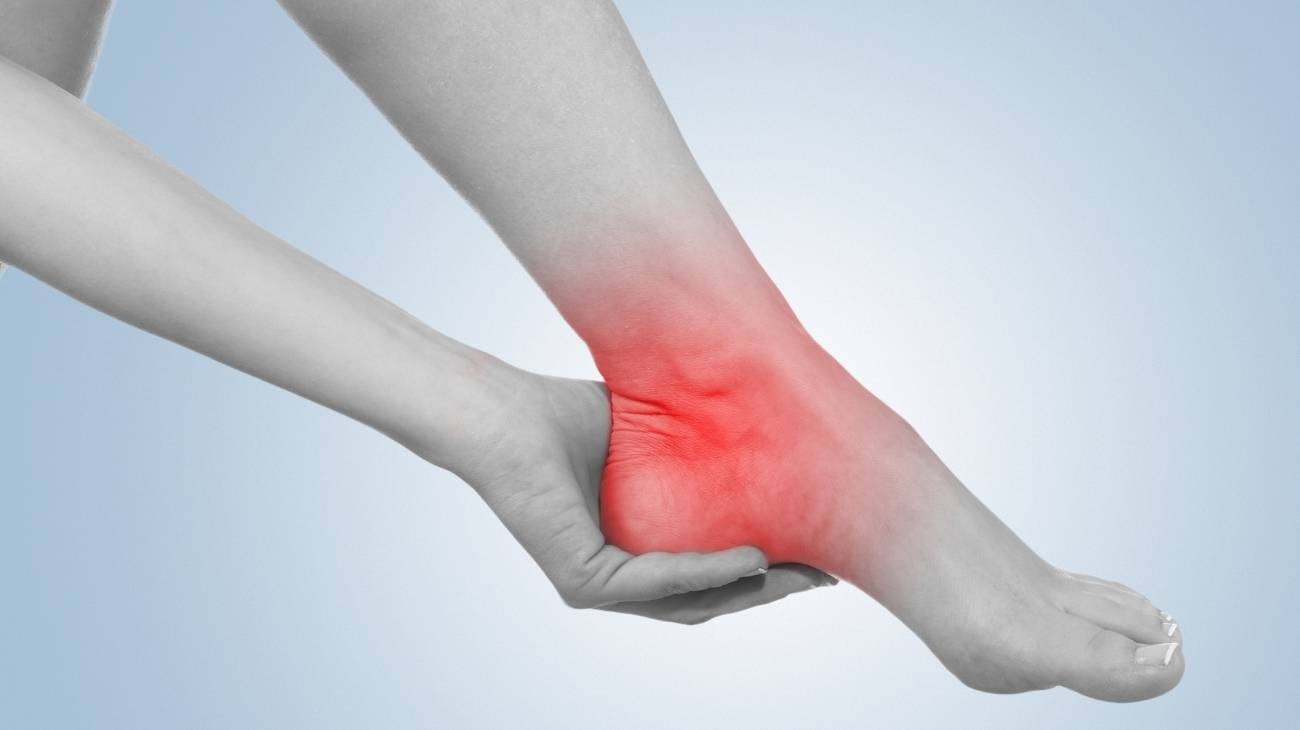
- Swelling: swelling in the knee is one of the most recurrent symptoms of patients with prepatellar bursitis or infrapatellar bursitis. This is due to enlargement of the bursae caused by excess synovial fluid.
- Pain: this symptom can be caused by the lack of space in the joint to perform movements, causing oppression of the nerves that pass through the joint capsule. This causes the muscles, tendons and bursae to be strained to perform their task.
- Appearance of lumps: nodules in front of the kneecap can be frequent in this type of disease. In this situation, it is advisable to visit the doctor so that the disease can be diagnosed correctly and so that it goes into remission as quickly as possible.
- Redness: in some cases, internal haemorrhages or accumulation of blood may occur due to the malfunctioning of the bloodstream in the joint area.
- Tingling sensation: paresthesia and loss of sensation are common symptoms in people suffering from prepatellar, suprapatellar or infrapatellar bursitis. This is due to the inflammation of these bursae, which leads to a reduced opening of the joint cavity.
- Loss of mobility: as there is a greater amount of synovial fluid in the bursae, they prevent the joint opening from functioning correctly, causing the patient to be unable to move.
- Numbness: the lack of mobility in the joint area causes the muscles and tendons to contract, resulting in unusual muscle stiffness.
- Fever: in some people it is possible to find a higher temperature in the knee area due to the inflammation of the bursae in this area.
- Loss of strength: knee bursitis can change the strength in the knee joint, making the patient unable to perform certain actions. It is common to find people unable to climb stairs, stand or hit a ball.
What treatments are there to improve the symptoms of knee bursitis?
The symptoms of knee bursitis can be reduced and even disappear in a short time. But for this it is necessary to undergo different treatments that are currently available.
See below the different therapies that can be applied to people with inflammation in the bursae near the kneecap
Alternative and complementary therapies
The following treatments are available to reduce the symptoms of knee bursitis:
- Heat and cold therapy: it is possible to apply this complementary method by means of cold cloths or ice packs and then use heat-emitting elements on the knee joint area. This improves the dilation of the blood vessels, reduces inflammation and has an analgesic effect, causing the cavity with synovial fluid to decompress because the tension has decreased. To apply this technique, the session should not exceed 20 minutes, starting with heat compresses, followed by cold elements and ending again with heat. It must be supervised by the doctor to avoid injury.
- Compression therapy: Compression knee braces used on suprapatellar, prepatellar and infrapatellar bursae are efficient because they cause immobilisation of the joint. This enhances the arterioles with the venules allowing the blood vessels to have a greater blood flow, thus causing the swelling to start to decrease and improving the enlargement of the joint cavity. Knee braces and compressive bandages are generally used, without negatively influencing the capillary walls.
- Thermotherapy: The aim of this therapy is to obtain all the benefits of deep heat. Hot cloths, water bags, electrotherapy and ultrasound can be used, which promotes the development of fluid and gas exchanges between the blood and the joint tissues. This means that the affected area will have a greater blood supply, which will reduce the swelling of the knee and allow the bursae located in this area to have more space to lubricate the movements.
- Natural remedies using plants: it is possible to find in this type of therapy lavender, boldo, lemon balm, thyme, basil, lavender and chamomile in the preparation of infusions that allow the patient to benefit from the anti-inflammatory and analgesic properties of these herbs. In addition, according to medical criteria, it is recommended to combine them with aromatherapy to provoke a much greater sense of wellbeing.
- Healthy lifestyle habits: A patient suffering from knee bursitis should be educated so that the condition does not recur in the future. To do this, the treating physician interacts with the person so that he/she understands the causes and risk factors that lead to the condition. This will help them to know how to lift heavy objects, what type of food to eat and how to warm up the muscular structure beforehand so as not to put pressure on the bursae when they have to carry out a risky activity.
Dietary supplements
Both glucosamine and chondroitin sulphate help to improve the symptoms of knee bursitis. In addition, it is possible to incorporate vitamins, hyaluronic acid (when there is an excess of sodium urate in the uric acid) and minerals that will help to decompress the joint cavity with synovial fluid. In this way the patient will be able to regain movement within a few weeks.
Physiotherapy treatments
It should be noted that self-massage is not recommended for the treatment of knee bursitis, so physiotherapy should be carried out by a qualified physiotherapist. Various techniques can be used to reduce pain, muscle numbness and inflammation.
Among the most common treatments are hydrotherapy, based on non-impact exercises under water, and laser beams applied to the affected area to generate internal heat and provide the benefits of thermotherapy.
Medications
Drug therapy should be advised by a doctor and should never be self-medicated. This is due to the hepatic and gastrointestinal consequences, beyond the increase in knee bursitis symptoms, that this wrong decision can bring.
Among the most commonly used medications to reduce the symptomatology of knee bursa inflammation are non-steroidal anti-inflammatory drugs such as naproxen, ibuprofen and acetylsalicylic acid. Paracetamol or other opioid analgesics may also be prescribed to reduce inflammation and pain. In more advanced cases, some doctors use injectable antibiotics.
Surgery and fluid removal
Knee bursitis can also be treated with methods that are a little more invasive for the patient. Synovial fluid can be removed by means of needles that are placed by the practitioner. In more complicated cases, it is possible to remove the fluid sacs by means of a surgical intervention, called bursectomy. It should be noted that these two techniques are only used in cases where the disease has progressed significantly.
What are the most effective prevention methods for knee bursitis?
Learn about all the preventive methods that will help you avoid inflammation of the bursa in the knee joint:
- Avoid excessive body weight: the knees are seriously affected when the patient is overweight. This is due to the demands placed on the prepatellar and infrapatellar bursae by the limited space in the joint.
- Choose a healthy diet: a balanced diet rich in minerals and proteins will help you to keep the joint tissues in perfect condition. In addition to weight control, you will benefit from the fact that the synovial sacs will not be under constant pressure.
- Protects the joint: Compression knee braces and supports will help you keep the whole body of the painful joint safe, so movements will always be safer and you will avoid bumps on the synovial bursae. This is recommended every time you have to play sports or do demanding work.
- Improve your posture: if for any reason you have to lift heavy objects, it is necessary to visit a physiotherapist for guidance on how to perform these actions. This will help you to avoid overstraining the joint and to improve the type of force you should apply.
- Warm up before lifting heavy things: it is very important to have the knee area prepared when you have to lift heavy things. For this reason, you should stretch the muscles surrounding the joint beforehand.
- If you feel pain, stop doing the activity: if you feel discomfort or notice that the knee area is swollen, you should visit the doctor urgently to diagnose what type of ailment you may be suffering from.
- Rest your knee: if you have to do demanding work with your knee, don't forget that every 2 hours or so, or whenever you feel fatigue, you should rest the joint so that the muscles and tendons can relax. This will prevent increased pressure in the synovial sacs.
References
- Le Manac’h, A. P., Ha, C., Descatha, A., Imbernon, E., & Roquelaure, Y. (2012). Prevalence of knee bursitis in the workforce. Occupational medicine, 62(8), 658-660. https://academic.oup.com/occmed/article/62/8/658/1439055
- Jensen, L. K., & Eenberg, W. (1996). Occupation as a risk factor for knee disorders. Scandinavian journal of work, environment & health, 165-175. https://www.jstor.org/stable/40966530
- Chatra, P. S. (2012). Bursae around the knee joints. Indian Journal of Radiology and Imaging, 22(01), 27-30. https://www.thieme-connect.com/products/ejournals/abstract/10.4103/0971-3026.95400
- LaPrade, R. F. (1998). The anatomy of the deep infrapatellar bursa of the knee. The American Journal of Sports Medicine, 26(1), 129-132. https://journals.sagepub.com/doi/abs/10.1177/03635465980260010501
- Price, N. (2008). Prepatellar bursitis. emergency nurse, 16(3). https://journals.rcni.com/emergency-nurse/prepatellar-bursitis-en2008.06.16.3.20.c8183
- Lustenberger, D. P., Ng, V. Y., Best, T. M., & Ellis, T. J. (2011). Efficacy of treatment of trochanteric bursitis: a systematic review. Clinical journal of sport medicine: official journal of the Canadian Academy of Sport Medicine, 21(5), 447. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3689218/
- Baumbach, S. F., Lobo, C. M., Badyine, I., Mutschler, W., & Kanz, K. G. (2014). Prepatellar and olecranon bursitis: literature review and development of a treatment algorithm. Archives of orthopaedic and trauma surgery, 134, 359-370. https://link.springer.com/article/10.1007/s00402-013-1882-7
- Aaron, D. L., Patel, A., Kayiaros, S., & Calfee, R. (2011). Four common types of bursitis: diagnosis and management. JAAOS-Journal of the American Academy of Orthopaedic Surgeons, 19(6), 359-367. https://journals.lww.com/jaaos/Abstract/2011/06000/Four_Common_Types_of_Bursitis__Diagnosis_and.6.aspx
- Shbeeb, M. I., & Matteson, E. L. (1996, June). Trochanteric bursitis (greater trochanter pain syndrome). In Mayo Clinic Proceedings (Vol. 71, No. 6, pp. 565-569). Elsevier. https://www.sciencedirect.com/science/article/abs/pii/S002561961164113X
- Alvarez-Nemegyei, J., & Canoso, J. J. (2004). Evidence-based soft tissue rheumatology IV: anserine bursitis. JCR: Journal of Clinical Rheumatology, 10(4), 205-206. https://journals.lww.com/jclinrheum/Abstract/2004/08000/Evidence_Based_Soft_Tissue_Rheumatology_IV_.7.aspx