- Definition: What is arthritis or joint inflammation?
- What are the most common types of arthritis?
- Best arthritis products
- What are the causes and risk factors for arthritis?
- Main symptoms that warn us that we have arthritis
- What treatments are available to improve the symptoms of arthritis?
- Which arthritis prevention methods are most effective?
- F.A.Q: Frequently asked questions
In this post you will learn about the disease that causes inflammation of the joints called arthritis. We will show you in detail which are the most common types of arthritis and what are the risk factors or causes that generate this ailment in patients.
We will also explain the main signs and symptoms that will help you to realise that you may be an arthritis patient. You will learn about the treatments that currently exist and that will help you to improve the symptoms of this ailment. Finally, we will talk about the most effective prevention methods that you should know.
Definition: What is arthritis or joint inflammation?
Arthritis is an inflammation of the joints caused by various diseases that can affect the muscles, bones or tissues that support the joints. Many people believe that arthritis occurs only in old age, which is completely wrong because it is also possible to find young people affected by arthritis.
The most common symptoms are stiffness, pain in the joint and swelling. To treat this type of disease it is possible to find different treatments that are applied according to the level of arthritis progression. There are many causes of arthritis, ranging from psoriasis, hepatitis, brucellosis and even Lyme (caused by ticks).
What are the most common types of arthritis?
We will show you below the most common types of arthritis that can be found in patients of both sexes. The pathological conditions that can cause arthritis are:
Rheumatoid arthritis
This disease is caused by the affected person's own immune system. The immune system attacks the defence cells, causing a disruption of the tissues and thus generating an inflammatory condition, usually in the hands and feet. The result is a progressive and systematic deformation of the small joints, causing stiffness and motor disability.
Diagnosis requires X-rays and laboratory tests, although in many cases the existence of rheumatoid arthritis can be detected by a physical examination by a doctor. Treatment for this set of symptoms is usually based on drugs, the most commonly used being corticosteroids, immune system suppressants and anti-inflammatory drugs.
Psoriatic arthritis
Psoriasis is a disease of autoimmune origin (generated by the immune system itself) and in some cases can be hereditary. This ailment produces inflammatory scales on the skin that cause itching. When it presents advanced and more complicated symptoms, it generates psoriatic arthritis.
For psoriatic arthritis to exist, it is necessary that no IgM antibodies or any other element suggesting rheumatoid arthritis are found, as in this case it will be diagnosed as in the previous point. It should be treated with physiotherapy, non-steroidal anti-inflammatory drugs, retinoids and cyclosporine (both immunosuppressants related to vitamin A). On the other hand, it is necessary to take habits for daily life to reduce the ailment.
Osteoarthritis
Although not true arthritis, osteoarthritis is known as osteoarthritis. It is a chronic condition that degenerates cells, affecting the structure of tissues and organs over time. It is slowly progressive and the microscopic and macroscopic lesions in the joints usually occur in older people.
Obesity and people over 60 years of age are the main risk factors for this inflammatory degenerative disease. Treatment requires a visit to a rheumatologist for anti-inflammatory drugs and analgesics, which is diagnosed by clinical analysis and physical examination.
Septic arthritis
The inflammation that occurs in this type of arthritis is caused by bacteria, a virus or a fungus, and can cause permanent damage to the joint. The infectious agent causes redness with increased temperature in the affected area, pain and swelling. These micro-organisms settle in the synovial fluid, causing the joint cartilage to be considerably affected.
These germs, which reach the joint, can use different types of dissemination. For example, blood or an infection in the bone that shares the synovial membrane. The diagnosis is made by means of a puncture of the synovial fluid, which is then cultured and studied by means of an antibiogram. In this way it is possible to know what type of bacteria is affecting the joint and to establish the most appropriate treatment.
Juvenile idiopathic arthritis
JIA, juvenile chronic polyarthritis or juvenile chronic arthritis is a disease that occurs in children between the ages of 2 and 16 years, with the female gender being more prone. The word idiopathic refers to the fact that the causes are not precisely determined, although it has been shown that the HLA-DR4 antigen in the immune system is more likely to develop the disease in patients.
Juvenile idiopathic arthritis causes inflammation of the synovial fluids and is treated with drugs, especially acetylsalicylic acid and methotrexate, which is a folic acid analogue. The use of corticosteroids is not recommended because they tend to affect the child's growth. It is possible to cure the disease completely and leave no sequelae in the patient for the future.
Degenerative arthritis
One of the characteristics of this type of arthritis is that the inflammation is minimal, but the articular cartilage is poorly formed. In this way, the bone hypertrophies, growing beyond the normal margins imposed by the cartilage. Metabolic diseases, obesity and some trauma can lead to the appearance of degenerative arthritis, causing globular sedimentation.
X-rays and an eye examination by a doctor can diagnose this numbness. Treatment consists of painkillers and anti-inflammatory drugs, as well as weight control with walking and special diets. In some cases surgical intervention is necessary.
Reactive arthritis
Reactive arthritis is a chronic disease caused by agents that attack the autoimmune system of the spine, including the sacroiliac joints and spine. These are the main differences with rheumatoid arthritis. In terms of symptoms, the urinary system and the digestive system are the main factors where the infection of this type of arthritis begins. Treatment for this type of arthritis is given by the specialised physician according to the patient's situation and disease progress, but usually involves drug therapy and complementary rehabilitative approaches.
Gouty or uric arthritis
Gout is a disease that attacks the soft tissues of the body, especially the kidneys and joints. The condition causes a build-up of salts derived from uric acid, mainly affecting the big toe. Gouty or uric arthritis, also called microcrystal arthritis, is the constant inflammation caused by the disease gout.
The drugs used for treatment are non-steroidal anti-inflammatory drugs, although colchicine and corticosteroids are also used to control swelling. It is possible to include drugs that remove uric acid. Don't forget that improving your lifestyle should be part of your treatment.
Best arthritis products
Bestseller
-
2 Elbow Compression Sleeve (Black/Gray)
£20,95 -
2 Elbow Compression Sleeve (Green/Navy)
£20,95 -
2 Elbow Compression Sleeve (Pink/Bordeaux)
£20,95 -
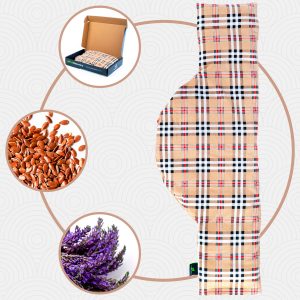
2 Mittens: Microwave Arthritis Gloves (Hearts)
£24,95 -
2 Mittens: Microwave Arthritis Gloves (Oxford)
£24,95 -
Ice Pack for Foot - Cold Therapy Socks (Black)
£20,95 -
Ice Pack for Foot - Cold Therapy Socks (Green)
£20,95 -
Ice Pack for Foot - Cold Therapy Socks (Pink)
£20,95 -
Microwavable Heated Slippers (Hearts)
£24,95 -
Microwavable Heated Slippers (Oxford)
£24,95 -
Microwavable Heated Slippers (Sport)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Hearts)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Oxford)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Sport)
£24,95 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Hearts)
£24,95 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Oxford)
£24,95 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Sport)
£24,95 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£20,95
-
2 Ankle Compression Sleeve (Black/Gray)
£20,95 -
2 Ankle Compression Sleeve (Green/Navy)
£20,95 -
2 Ankle Compression Sleeve (Pink/Bordeaux)
£20,95 -
2 Knee Compression Sleeve (Black/Gray)
£20,95 -
2 Knee Compression Sleeve (Green/Navy)
£20,95 -
2 Knee Compression Sleeve (Pink/Bordeaux)
£20,95 -
2 Patella Knee Strap (Black/Gray)
£12,95 -
2 Patella Knee Strap (Green/Navy)
£12,95 -
2 Patella Knee Strap (Pink/Bordeaux)
£12,95 -
2 Tennis Elbow Brace (Black/Gray)
£12,95 -
2 Tennis Elbow Brace (Green/Navy)
£12,95 -
2 Tennis Elbow Brace (Pink/Bordeaux)
£12,95 -
Back Support Belt (Black)
£39,95 -
Back Support Belt (Green)
£39,95 -
Back Support Belt (Pink)
£39,95 -
Foot Massage Roller for Plantar Fasciitis (Black)
£20,95 -
Foot Massage Roller for Plantar Fasciitis (Green)
£20,95 -
Foot Massage Roller for Plantar Fasciitis (Pink)
£20,95 -
Sacroiliac Support Belt (Black)
£24,95 -
Sacroiliac Support Belt (Green)
£24,95 -
Sacroiliac Support Belt (Pink)
£24,95 -
Shoulder Support Brace (Black)
£24,95 -
Shoulder Support Brace (Green)
£24,95 -
Shoulder Support Brace (Pink)
£24,95
What are the causes and risk factors for arthritis?
The causes and risk factors for arthritis are any exposure, situation or condition that increases a person's chances of contracting or developing the disease. This is not only due to a single circumstance, but can be a combination of complementary elements. Arthritis can also be generated as a consequence of the existence of previous diseases.
Therefore, we will show you below a list of the causes and risk factors for arthritis:
- Hereditary factors: In people with arthritis there are certain genetic factors that do affect the development of this pathology, but it must be taken into account that no more than 5% of sufferers have a direct ancestry of parents with RA. Therefore, a patient's children and siblings are unlikely to contract the disease, but genetics is considered a risk factor.
- Immune system disorders: The antigens created by the immune system serve to defend cells against pathogens. When this defence mechanism of the body does not detect infected tissues or microorganisms, it starts to attack healthy cells, causing arthritis, among other things.
- Trauma to the joint: Chondrocytes, macromolecules and synovial fluid are involved in the elasticity and lubrication of the joint. When some of the biomechanical functions are affected, they can lead to synarthrosis, diarthrosis or amphiarthrosis, which is an important antecedent for the development of RA. These can also be caused by problems in the development of articular cartilage.
- Bacteria, viruses and even fungi: which enter the joint cavity with synovial fluid through the blood or by other means. It can also be due to exposed trauma or after-effects of repetitive work.
- Obesity: is also a risk for developing gouty or uric arthritis, as well as a direct cause of osteoarthritis. Joint erosion is caused by excessive load on the joint, but also adipokines, present in fat, stimulate inflammation, which leads to the autoimmune system working overtime and in the long term self-generating arthritis.
- Wear and tear on the joint due to weak muscles: Lack of exercise can lead to myasthenia, which means that the muscles cannot support the joint socket properly, leading to deterioration of the synovial membrane and possible development of arthritis.
- Repetitive movements: over prolonged periods of time, also lead to joint erosion, causing the joint to become increasingly overloaded. It is therefore necessary to be alert to the appearance of tendonitis or carpal tunnel, among many other injuries, because they could be the prelude to RA.
- Other causes: Age, sex, smoking, prolonged exposure to the cold and playing sports that require frequent jumping, falling or striking with the hands or feet.
Main symptoms that warn us that we have arthritis
If something in the body is not working well, it is important to be alert and pay attention to signs of injury or illness so that a doctor can be consulted immediately. For this reason, it is necessary to know the symptoms and signs of arthritis in the patient's body.
We will show you below the main symptoms of this ailment:
- Pain in the neck, jaws, shoulders, hips, elbows, wrists, hands, knees, ankles or feet: In addition, it is possible to find patients with pain in the muscles and back. The pain is due, among other factors, to a possible eruption of the articular cartilage and deficiency of synovial fluid work.
- Numbness: The muscles in the affected area stiffen due to the tension generated by the patient every time he feels pain. This symptom is also caused by inflammation of the tendons that support the bones when a nearby nerve is pressed.
- Swelling: This symptom is caused by inflammation of the membrane, which is pushed by the synovial fluid that protects the cartilage and gives meaning to the joint. This may be accompanied by paraesthesia, a special numbness or tingling sensation in the affected area.
- Redness: Erythema on the skin is a very important symptom that can warn that the blood supply through vasodilatation occurs in excess in the joint area. This is a very important factor to take into account when detecting arthritis.
- Other symptoms to keep in mind: pleurisy, difficulty sleeping, blood in the stool, chronic conjunctivitis, dry eyes, fatigue for no reason, nodules and burning in the feet and hands.
What treatments are available to improve the symptoms of arthritis?
Once the disease and the type of arthritis the person suffers from have been detected, it is necessary for the doctor to establish a therapy by means of medication and treatment with general suggestions for life and also complementary suggestions for the patient. It must be taken into account that the treatment is prolonged and at present there is no definitive cure for arthritis, although the symptoms and effects can be attenuated or go into remission.
The treatments that currently exist to improve the symptoms of arthritis are:
Alternative and complementary therapies
Chiropractic treatments are complementary therapies that help to reduce the ailment, but in no case do they replace the administration of medication recommended by the doctor. It should be taken into account that for their implementation it is necessary to consult a health professional beforehand.
These therapies include:
- Cold and heat therapy: depending on the patient's tolerance, a cold and heat therapy can be useful to reduce pain and muscle tension in the affected area, and the application should not exceed 15 minutes. Warm water bags, hot water baths or a blanket designed for this purpose can be used to distribute heat, while ice packs, ice and frozen towels can be used to apply cold and reduce swelling. This technique consists of a combination of both methods, starting with heat, then cold and ending with the application of high temperature.
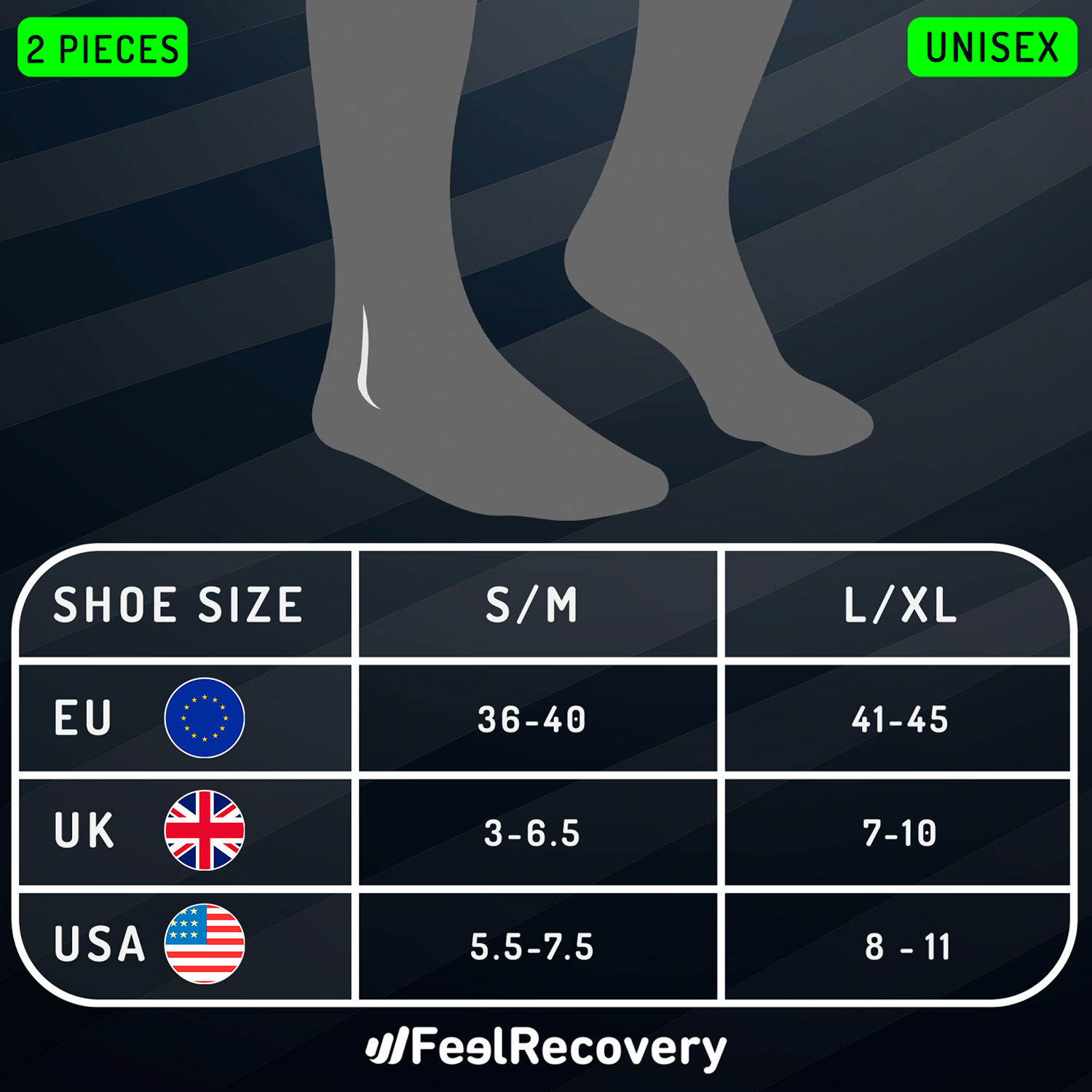
- Compression therapy: This technique is based on the use of supports made of different materials to support the joint affected by arthritis. In this way it is possible to protect the knees, limit natural movements to avoid re-injury and reduce synovial membrane stiffness to obtain smoother movements. To apply this treatment it is necessary to be directed and observed by a doctor, as there are different sizes and designs that can affect the symptoms of the disease.
- Massage therapy: Stimulation of the affected areas by manual massage improves muscle tension and strengthens the muscles, thus decreasing the pressure on the joint quality with synovial fluid. This reduces the pain and swelling caused by arthritis. Common massages include Swedish, deep tissue, hot stone, Ayurvedic, Thai and rolfing.
- Acupressure therapy: This ancient technique is used to stimulate the central nervous system by applying pressure to specific areas of the body using only the therapist's hands. This reduces the stiffness of the body that is affected by arthritis. Pain signals are inhibited so that they do not reach the brain and in this way, through high stimulation, the body releases endorphins which act as a powerful painkiller.
- Thermotherapy: the thermal treatment used in this type of therapy is related to the temperature of the elements that are placed on the patient's affected area. Unlike hot and cold therapy, this technique involves only heat baths by means of wet compresses that generate a differential temperature.
- Natural remedies using plants: this type of treatment is based on plants that are obtained from nature and in which it is possible to find components that relieve the swelling, redness, pain and stiffness of the joint. It should be noted that this type of therapy must be accompanied by drugs prescribed by a rheumatologist. In addition, it is necessary to consult a doctor about its implementation and to know what benefits can be obtained with this alternative method.
- Ultrasound: In this technique, high-level sound waves are used to reach a high frequency so that they can be applied to joints suffering from arthritis. It should be borne in mind that special equipment is needed for its application, which is handled by suitable professionals in order to obtain a progressive relaxation over time.
- Meditation and relaxation: both meditation and relaxation are efficient techniques used to find peace and tranquillity in times of pain attacks caused by arthritis. In this way, muscle tension decreases, causing the synovial membrane to be less affected by the pressure, so that the patient, through breathing, concentration and other meditation practices, can find a psychological balance and face the disease from a happier point of view.
- Aromatherapy: the treatment based on aromas helps to calm the pain according to recent studies carried out by prestigious international medical centres. In this way it is possible to reduce anxiety, causing rapid relaxation, as well as relief and revitalisation of the patient. Vanilla, jasmine, lemon, orange, grapefruit, mint and green apple are some of the elements used to decrease cardiac rhythms and increase pleasant smells and combat arthritis.
- Acupuncture: this old oriental practice in which needles are inserted into areas affected by arthritis produces endorphins and acts as an analgesic to reduce arterial tension and pain. While it is true that acupuncture has not yet shown direct results, it is advisable to consult a doctor before starting this Chinese technique.
- Biofeedback: This treatment is aimed at explaining to the patient how their body acts when they feel pain from arthritis. To do this, the person is connected to specific electrical equipment with sensory plates that show blood pressure, muscle tension, heart rate and temperature when the patient is in pain or when their body is tense. Once the parameters are known, the doctor explains to the individual how to deal with stressful situations caused by pain and muscle tension.
- Healthy lifestyle habits: walking, exercising, having a correct posture when the patient works and lifting objects in an ideal way are some of the recommendations and practices that are carried out with this treatment of healthy lifestyle habits. It is necessary that the person learns to live with arthritis in order to reduce the ailment and improve the quality of life. For this, it is advisable to know the disease in depth, talk to the doctor openly and receive all the advice in an optimistic way in order to have more fun and not be limited by arthritis.
Dietary supplements
The therapeutic potential of some herbs helps to reduce arthritic complaints. Before administration, however, ask the doctor about the inclusion of these natural and synthetic components in the therapy for the patient. Glucosamine and chondroitin sulphate are two substances that are present in joint cartilage and are the most commonly used for this type of supplement therapy.
Physiotherapy treatments
Occupational physiotherapy is a type of treatment that involves the correction of certain movements that the patient performs in their daily activity, for example, sitting, lifting and posture when working. This is accompanied by techniques and exercises to reduce the pain in the inflamed joints.
Medications
The drugs used in arthritis therapy are non-steroidal anti-inflammatory drugs, analgesics, DMARDs and biological disease-modifying antirheumatics. In addition to these, gastric protectants are used to prevent stomach heaviness, vomiting, gastritis and ulcers.
It should be borne in mind that self-medication can lead to serious inconvenience and more severe disease disorders, so the amount and use of medication must be exclusively prescribed by the doctor.
Surgery
Surgical treatments are necessary only when indicated by the doctor and when the progression of the disease requires it. These techniques can range from arthroscopy to the implementation of a prosthesis; however, it is possible to find patients with surgical interventions such as synovectomy, arthroplasty, arthrodesis, osteotomy and tendon reconstruction.
Which arthritis prevention methods are most effective?
Although there are some risk factors that cannot be avoided, as mentioned in previous paragraphs, it is possible to reduce or delay the onset of some types of arthritis by taking into account different methods of prevention.
For this reason, we will show you below an enunciative list of tips that will help you to preventively reduce the symptoms of this ailment:
Consult your doctor
The first thing you should do is visit your doctor and explain the ailments and complications you have in your joints. Keep in mind that arthritis is a chronic and progressive disease, so as time goes by the lesions may become worse if a doctor does not intervene at the right time.
Eat a healthy diet
A healthy, balanced diet will help delay the onset of arthritis and reduce joint pain. Certain fish, rich in Omega 3, reduce inflammation, while eating dairy products and green vegetables improves bone strength, as they contain vitamin D. On the other hand, specific foods help combat cystitis, such as green tea, citrus fruits, walnuts and extra virgin olive oil.
Exercise
Nutrition will benefit and be supported if you do not lead a sedentary life. This is because muscles weaken when you sit for too long, increasing the likelihood of arthritis. Keep in mind that aerobic, stretching and strength exercises are ideal for the prevention of arthritis.
Don't forget that sports injuries can cause damage to the articular cartilage within the synovial membrane, which is a major risk factor for arthritis. For this reason, you should be careful enough to avoid rapid wear and tear on your joints by using warm-up techniques and exercises prior to your sports routine.
Control overweight
If you eat a healthy diet and exercise regularly, you will avoid becoming overweight. People with obesity are prone to developing arthritis in the hips and knees, so it is necessary to control weight and blood pressure to avoid the development of joint inflammation. This will develop into potential arthritis in the future.
Avoid smoking
It has been shown that people who smoke are more likely to develop rheumatoid arthritis, so it is advisable to eliminate this unhealthy practice not only for the sake of joint care, but also to protect the respiratory system from COPD.
F.A.Q: Frequently asked questions
Below you will find a complete list of frequently asked questions that people ask, which will help you to differentiate concepts and get a deeper understanding of what arthritis is. Take a look.
References
- Aletaha, D., & Smolen, J. S. (2018). Diagnosis and management of rheumatoid arthritis: a review. Jama, 320(13), 1360-1372. https://jamanetwork.com/journals/jama/article-abstract/2705192
- Firestein, G. S. (2003). Evolving concepts of rheumatoid arthritis. Nature, 423(6937), 356-361. https://www.nature.com/articles/nature01661
- Meenan, R. F., Gertman, P. M., & Mason, J. H. (1980). Measuring health status in arthritis. Arthritis & Rheumatism, 23(2), 146-152. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780230203
- Fries, J. F., Spitz, P., Kraines, R. G., & Holman, H. R. (1980). Measurement of patient outcome in arthritis. Arthritis & Rheumatism, 23(2), 137-145. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780230202
- McInnes, I. B., & Schett, G. (2011). The pathogenesis of rheumatoid arthritis. New England Journal of Medicine, 365(23), 2205-2219. https://www.nejm.org/doi/full/10.1056/NEJMra1004965
- Sibley, J. T. (1985). Weather and arthritis symptoms. The Journal of Rheumatology, 12(4), 707-710. https://europepmc.org/article/med/4057192
- SCHAIBLE, H. G., Ebersberger, A., & Von Banchet, G. S. (2002). Mechanisms of pain in arthritis. Annals of the New York Academy of Sciences, 966(1), 343-354. https://nyaspubs.onlinelibrary.wiley.com/doi/abs/10.1111/j.1749-6632.2002.tb04234.x
- Smolen, J. S., Aletaha, D., Koeller, M., Weisman, M. H., & Emery, P. (2007). New therapies for treatment of rheumatoid arthritis. The lancet, 370(9602), 1861-1874. https://www.sciencedirect.com/science/article/abs/pii/S0140673607607843
- Burmester, G. R., & Pope, J. E. (2017). Novel treatment strategies in rheumatoid arthritis. The Lancet, 389(10086), 2338-2348. https://www.sciencedirect.com/science/article/abs/pii/S0140673617314915
- Majithia, V., & Geraci, S. A. (2007). Rheumatoid arthritis: diagnosis and management. The American journal of medicine, 120(11), 936-939. https://www.sciencedirect.com/science/article/abs/pii/S0002934307003610