- What is arthritis of the hip or inflammation of the hip joint?
- What are the causes and risk factors for osteoarthritis of the hip?
- Best products for hip arthritis
- Main symptoms that warn us that we have hip arthritis
- What treatments are available to improve the symptoms of osteoarthritis of the hip?
- Which methods of prevention for osteoarthritis of the hip are the most effective?
Osteoarthritis of the hip is a type of inflammation that is very painful for the patient, causing numbness and prolonged spasms. If you want to know in depth what this ailment originating in the joint between the femur and the pelvis is about, continue reading this post.
We will show you, in detail, the causes and risk factors of osteoarthritis of the hip. In addition, we will name the main signs and symptoms that will warn you about the presence of this ailment. Don't miss anything because you will learn about the treatments to improve the symptoms and the prevention methods that you should take into account.
What is arthritis of the hip or inflammation of the hip joint?
Osteoarthritis of the hip is an inflammatory disease that occurs in the joint between the head of the femur and the pelvis, causing deterioration of the articular cartilage, compression of the membrane and deficiency of synovial fluid.
The two most prominent symptoms of this pathology are pain and stiffness of the hip. Both are caused by the loss of function of the joint and occur especially after a night's rest. For treatment, it is necessary to see a rheumatologist as a matter of urgency to diagnose the progress of the disease and the applicable therapies. If you would like to know the causes, symptoms and treatments for this ailment, we invite you to read on.
What are the causes and risk factors for osteoarthritis of the hip?
Risk factors for osteoarthritis of the hip are the patient's own circumstances that increase the likelihood of contracting the disease. While the causes refer to the acts or events that the person has suffered in the past and that provoked activities in the immune system that increased the probability of becoming ill.
We will show you below what are the antecedents that influence the appearance of this type of joint deterioration, take a look:
- Trauma: injuries caused by blows are one of the main causes of wear and tear of the coxofemoral joint. This can lead to the intrusion of bacteria or viruses into the synovial fluid, thus generating a type of septic arthritis. On the other hand, if the injury is poorly healed, the joint will not function properly, causing deformities in the cartilage.
- Congenital disorders: another cause of osteoarthritis of the hip, especially in younger patients, is the development of growth disorders since pregnancy. Dysplasia and Perthes disease are the most frequent pathologies that cause inflammation in the joint. Dysmetry in the lower limbs is also a risk factor.
- Obesity: being overweight is an important risk factor that must be taken into account in order to avoid osteoarthritis of the hip. This is due to the strain on the joint to allow the leg and trunk to perform all natural movements. The squeezing between the pelvis and the femoral head causes great pain when the synovial membrane is compressed.
- Repetitive tasks: osteoarthritis of the hip can also be generated when the patient performs activities that require a great effort of the joint for a long time and do it permanently.
- Excessive heavy lifting: As with obesity, overloading is also a factor that can lead to inflammatory joint disease. The excessive weight placed on the hip cartilage when doing this task is too great, leading to future injuries.
- Sedentary lifestyle: Lack of exercise can also be a risk factor for osteoarthritis of the hip. Articular cartilage can be affected if it is not constantly functioning, causing loss of texture and stiffness.
- Age and gender of the patient: the disease recurs in people over the age of 50 and in women. This is why osteoarthritis of the hip is considered to be an idiopathic condition, as it is not possible to know precisely why it affects this group of people.
Best products for hip arthritis
Bestseller
-
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Hearts)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Oxford)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Sport)
£24,95 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Hearts)
£24,95 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Oxford)
£24,95 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Sport)
£24,95 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Hearts)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Oxford)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Sport)
£20,95
-
Back Support Belt (Black)
£39,95 -
Back Support Belt (Green)
£39,95 -
Back Support Belt (Pink)
£39,95 -
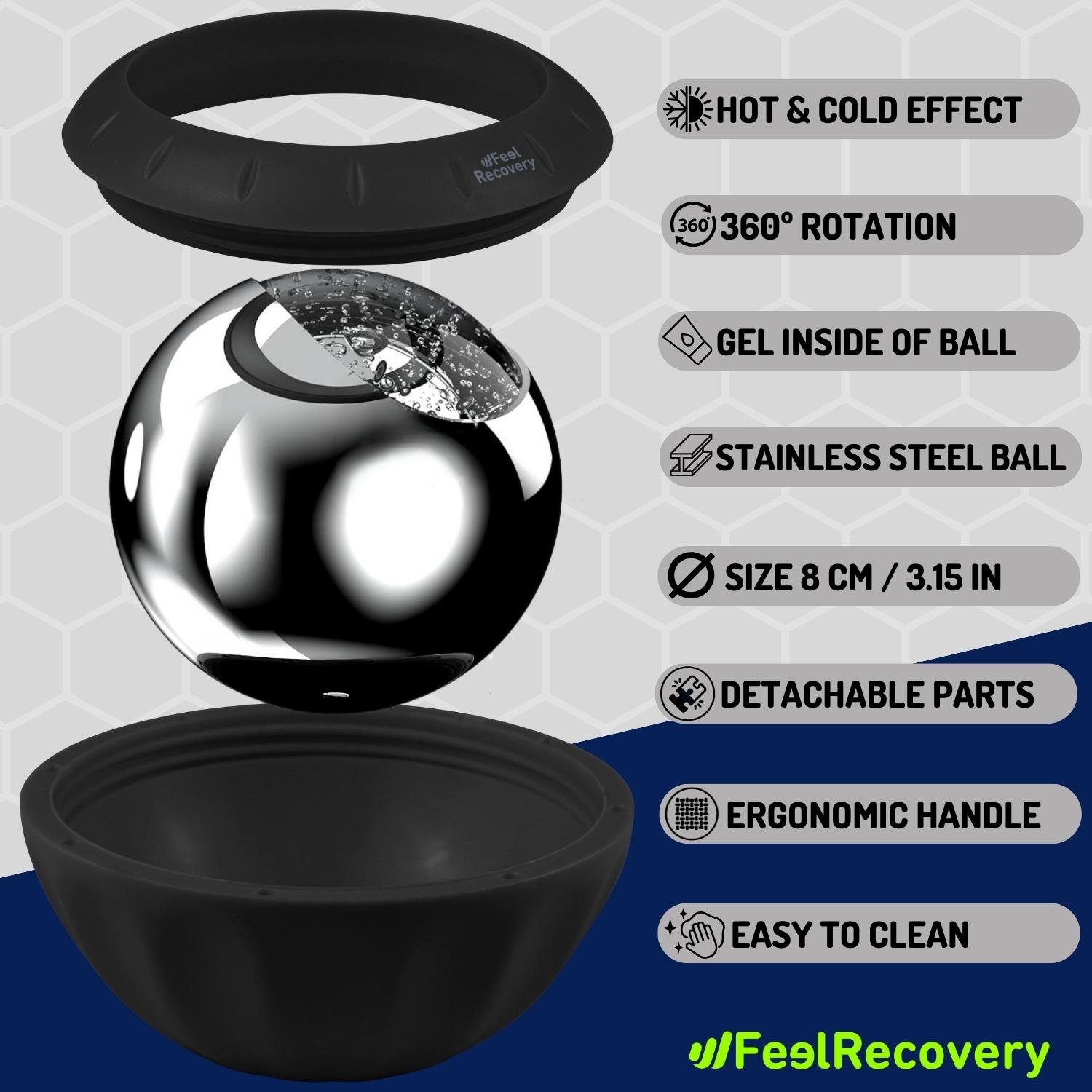
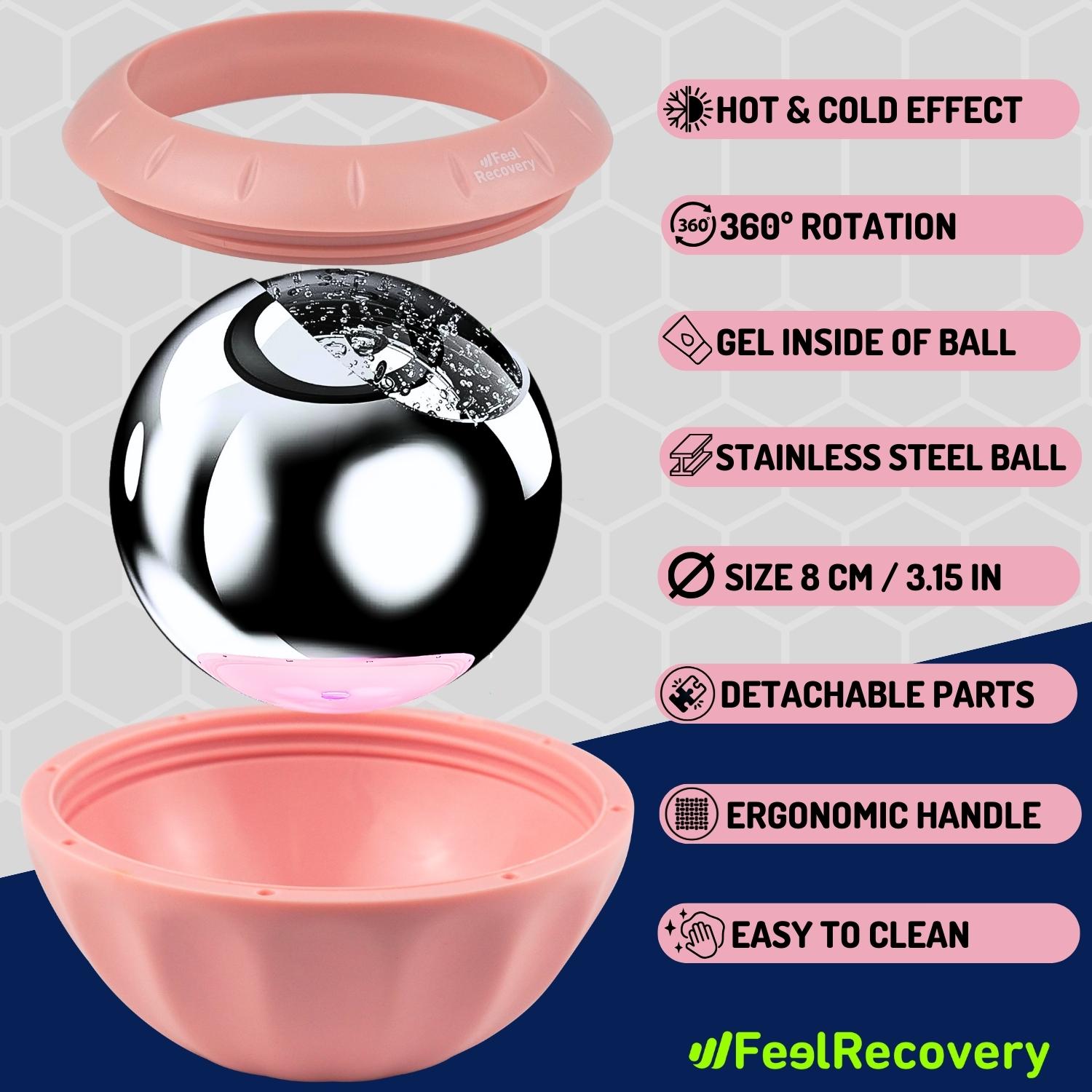
Ice Massage Roller Ball (Black)
£34,95 -
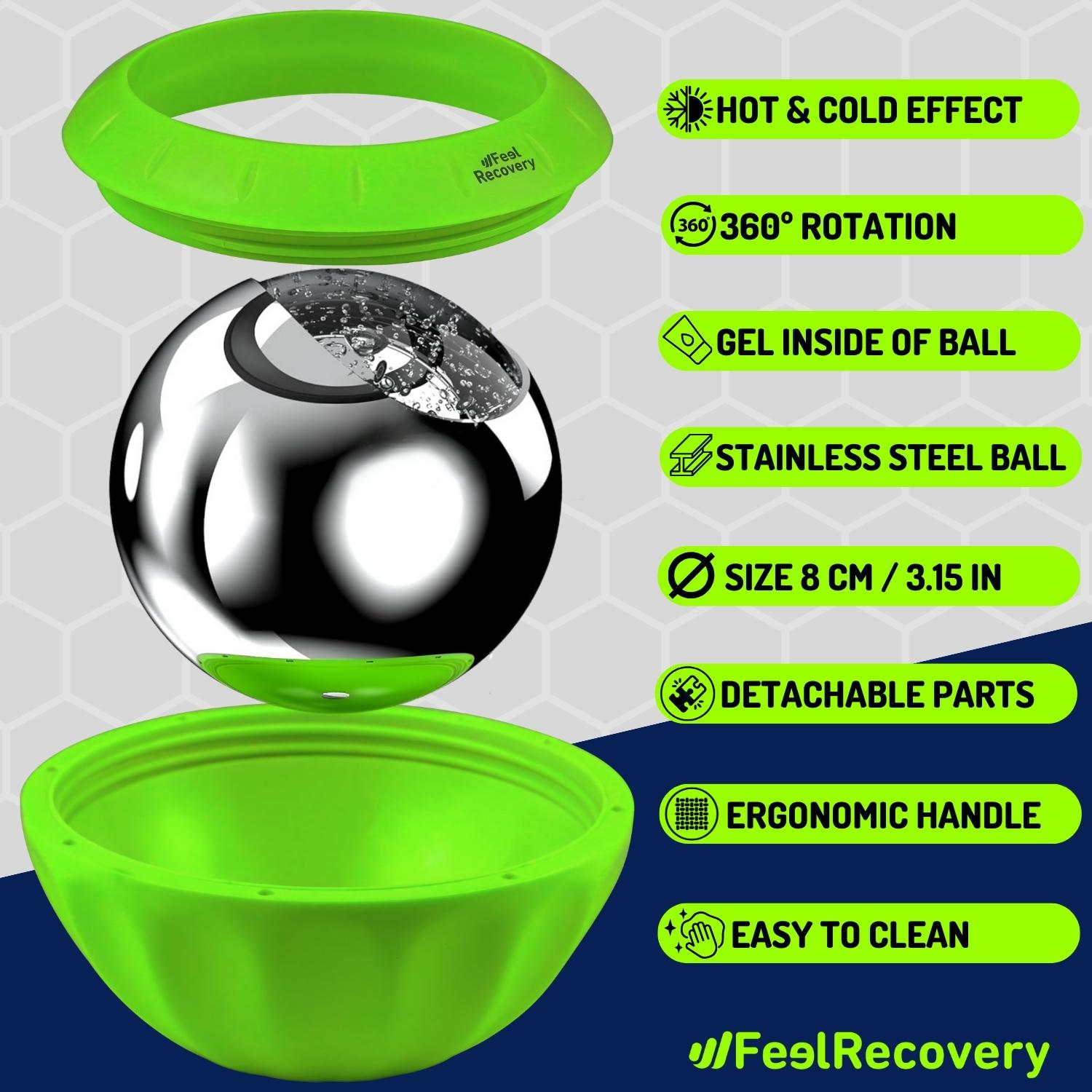
Ice Massage Roller Ball (Green)
£34,95 -
Ice Massage Roller Ball (Pink)
£34,95 -
Sacroiliac Support Belt (Black)
£24,95 -
Sacroiliac Support Belt (Green)
£24,95 -
Sacroiliac Support Belt (Pink)
£24,95 -
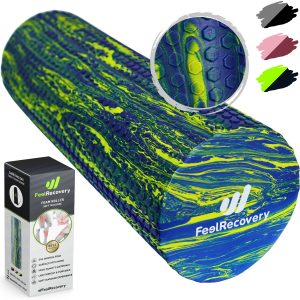
Soft Density Foam Roller for Recovery (Black)
£34,95 -
Soft Density Foam Roller for Recovery (Green)
£34,95 -
Soft Density Foam Roller for Recovery (Pink)
£34,95
Main symptoms that warn us that we have hip arthritis
The signs and symptoms that will warn you if you have osteoarthritis of the hip are listed below, which means that they are not all of them, as you may suffer from other very specific symptoms that are not on this list. For this reason, it is advisable to visit your doctor if you have any symptoms.
See below:
- Intense pain: this is the main symptom of the disease, it occurs especially in the morning hours when the person gets up from their night's rest. Pain may be felt in the groin, although it is also possible to find patients with pain in the thigh and buttock. In minor cases, the pain may extend to the knee and waist.
- Lack of mobility: loss of mobility to perform everyday tasks, such as dressing or crossing the legs, is a characteristic symptom of this joint complaint.
- Asymmetry in walking: the stiffness that occurs in the muscles can cause limping, but this symptom is also caused by wear and tear on the articular cartilage of the hip.
- Tight muscles: contractures can occur in the hip area, leading to more intense low back pain caused by the lack of natural movement of the joint.
- Lack of rest at night: in advanced cases it is possible to find patients with intense pain in different parts of the body and the impossibility of correct flexion and extension of the lower limbs.
What treatments are available to improve the symptoms of osteoarthritis of the hip?
There are different treatments that can be applied to improve the symptoms of osteoarthritis in the hip area. Pay attention to each one, but keep in mind that their implementation must be prescribed by a doctor.
Complementary and alternative therapies
Complementary and alternative therapies are methods used to alleviate the symptoms of hip arthritis. We will show you below which additional rehabilitative approaches to drug therapy are available to you and can be chosen with the prescription of the rheumatologist.
These are:
- Heat and cold therapy: this type of therapy can be applied to the affected areas by means of a hot water bottle, or heating mat, and then ice. This allows the muscle-tendon structure to relax, preventing the inflammatory outbreak in the joint. The technique of use is heat-cold-hot and should not exceed 15 to 20 minutes.
- Compression therapy: Compression of the coxofemoral joint is possible by means of bandages, splints and elastic devices that help the cartilage to make regular movements in order to stimulate future repair. This also helps to keep the hip in alignment with the rest of the body, which improves the smoothness of the joint.
- Massage therapy: As the coxofemoral joint is a multi-axial joint, it is necessary for the joint to perform a variety of natural movements. Massage helps to traction the hip and relax the muscles in the affected area. This results in a reduction of pain and a feeling of well-being. To perform this therapy it is necessary to consult a doctor and to have it carried out by a professional.
- Acupressure therapy: this millenary Chinese technique consists of applying pressure with the palms of the hands and fingers on different areas of the body. This produces small electrical impulses in the nerves causing the patient to relax, reduce stiffness in the muscle-tendon structure and improve the functioning of the articular cartilage.
- Thermotherapy: the implementation of the analgesic properties of heat is also a good idea when seeking to relax the muscles and reduce the tightness in the joint. To perform this complementary therapy, it is necessary to consult a doctor beforehand to avoid epidermal and joint injuries. In addition, it is important to take into account the time of application, as it cannot exceed 20 minutes and 3 sessions per day.
- Natural remedies using plants: ginger, willow, peppermint, cayenne and dandelion are some of the medicinal herbs used to relieve the pain of osteoarthritis of the hip. The technique of this complementary treatment is usually to make an infusion with the chosen medicinal plant and then drink it in recommended doses. Please note that in order to avoid stomach and liver damage, it is necessary to consult your doctor before including this therapy in your treatment.
- Ultrasound: through frequencies higher than sound it is possible to produce heat by means of the holistic friction technique in different areas and can have a reach of up to 7 centimetres of penetration in the patient's body. This improves the synovial capsule so that its structure can work in a more convenient way.
- Meditation and relaxation: the aim of this type of complementary therapy is for the patient to control their breathing in order to achieve mental and physical balance. This helps to better withstand pain when it occurs intensely. The great advantage of this method is that it can be applied anywhere and at any time.
- Aromatherapy: essences and oils are used in this treatment to combat the pain of osteoarthritis of the hip through mental relaxation of the patient. These oils can be used in burners or evaporators so that their fragrances can be perceived by the patient. Among the best known oils are marjoram (also called white thyme), rosemary and juniper.
- Acupuncture: this oriental practice is used by inserting needles strategically in different parts of the body to act on the nerves. These emit signals that stimulate feelings of well-being and block pain, preventing it from reaching the brain. This results in relaxation of the muscles and tendons near the coxofemoral cartilage.
- Biofeedback: this type of therapy targets the cognitive behaviour of the patient so that he/she knows what is happening in the body when there are attacks of pain caused by coxarthrosis. This improves the patient's condition because it will prevent stress on the patient when he/she has to overcome stages of pain. One technique used is to stand the patient in front of a mirror so that, by means of visual stimuli, he or she can understand his or her current situation.
- Healthy lifestyle habits: daily exercises, avoiding heavy loads, eating healthy and regular visits to the doctor are some of the instructions used in this complementary treatment for osteoarthritis of the hip. This helps to improve the capsule containing the joint cartilage to prevent wear and tear on the cartilage and thus reduce pain and muscle-tendon stiffness.
Dietary supplements
The dietary treatment given to the patient is of vital importance to improve the overall condition of the person. This helps to reduce muscle stiffness and relieve joint pain. As a complement to the diet, different elements are applied that incorporate substances that are favourable to the immune system into the organism.
Among these food supplements are all those that improve the viscoelasticity of the cartilage, whereby vitamins E, C and D are indispensable for improving collagen and other joint components. Chondroitin sulphate, hyaluronic acid and glucosamine should also be included as supplements.
Physiotherapy treatments
Physiotherapy is a treatment that helps to reduce muscle spasm through professionally directed exercises to strengthen the hip musculature. This is done through stretching for a few seconds to obtain a better opening of the muscle-tendon structures. In order to carry out this treatment, the physiotherapist analyses the patient's conditions in order to know which types of exercises can be performed during the sessions. For this reason, physiotherapy should never be chosen without first consulting a doctor.
Medications
The first thing you should know is that self-medication is very dangerous for osteoarthritis of the hip, so before taking any medication you should consult your doctor to assess your personal situation. The pharmacological treatment applied in this type of joint ailment are non-steroidal anti-inflammatory drugs and paracetamol, which are chosen in mild to moderate cases. But in more advanced situations the patient may be given Duloxetine to mitigate the pain. In all these cases it is necessary to analyse the patient's hepatic and stomach tolerance in order to prescribe opioids.
Surgery
Surgery is performed only in advanced cases of osteoarthritis of the hip, and different procedures may be applied according to the severity of the disease and the doctor's criteria. Among the most common surgical techniques is arthroscopy, which is used to remove pieces of cartilage or to check its general condition.
It is also possible to find patients who undergo osteotomy to realign the joint and, in some very complex cases, some femoral components are replaced by means of a prosthesis.
Which methods of prevention for osteoarthritis of the hip are the most effective?
The prevention methods you should take into account to avoid osteoarthritis of the hip are:
- Overweight: A person with obesity has a 25% chance of contracting osteoarthritis of the hip. Therefore, you should control your weight so as not to strain the coxofemoral multiaxial joint in every movement you make.
- Exercise regularly: Don't forget that a sedentary lifestyle is also a risk factor for this ailment, so a good preventive measure is to walk at least 30 minutes a day.
- Low-impact sports: Do not practice high-impact sports or activities, as this will prevent the joint cavity with synovial fluid from being affected by pressure. Sports such as swimming are a great alternative for keeping active and not damaging the hip.
- Have regular clinical and radiographic studies: to detect in advance any factor that may cause hip arthritis, especially if you have parents or siblings who suffer from this disease.
- Choose a healthy diet: A diet rich in vitamins and proteins, including Omega 3 and vegetables, is ideal for preventing this type of pathology. Avoid fatty foods.
- Visit the doctor: Do so if you have any of the symptoms mentioned in the previous paragraphs. This will help you to prevent the disease, as it can be controlled or go into remission quickly.
- Avoid smoking and alcohol: although not directly related to osteoarthritis of the hip, dependence on toxic substances affects the immune system in general and is best avoided.
- Sleep 7 to 8 hours a day: A good night's rest is a highly effective method of prevention, so you should try to get as many hours of rest as possible on a comfortable mattress.
References
- Cooper, C., Coupland, C., & Mitchell, M. (1995). Rheumatoid arthritis, corticosteroid therapy and hip fracture. Annals of the rheumatic diseases, 54(1), 49-52. https://ard.bmj.com/content/54/1/49.short
- Lavernia, C. J., & Villa, J. M. (2016). High rates of interest in sex in patients with hip arthritis. Clinical Orthopaedics and Related Research®, 474, 293-299. https://link.springer.com/article/10.1007/s11999-015-4421-8
- Hozack, W., Parvizi, J., & Bender, B. (2009). Surgical Treatment of Hip Arthritis: Reconstruction, Replacement, and Revision E-Book: Expert Consult-Online and Print. Elsevier Health Sciences. https://books.google.es/books?hl=en&lr=&id=xIGaC33lZ5gC
- Tsertsvadze, A., Grove, A., Freeman, K., Court, R., Johnson, S., Connock, M., ... & Sutcliffe, P. (2014). Total hip replacement for the treatment of end stage arthritis of the hip: a systematic review and meta-analysis. PLoS One, 9(7), e99804. https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0099804
- Banaszkiewicz, P. A. (2014). Traumatic arthritis of the hip after dislocation and acetabular fractures: treatment by mold arthroplasty: an end-result study using a new method of result evaluation. Classic papers in orthopaedics, 13-17. https://link.springer.com/chapter/10.1007/978-1-4471-5451-8_3
- Aletaha, D., & Smolen, J. S. (2018). Diagnosis and management of rheumatoid arthritis: a review. Jama, 320(13), 1360-1372. https://jamanetwork.com/journals/jama/article-abstract/2705192
- Firestein, G. S. (2003). Evolving concepts of rheumatoid arthritis. Nature, 423(6937), 356-361. https://www.nature.com/articles/nature01661
- Meenan, R. F., Gertman, P. M., & Mason, J. H. (1980). Measuring health status in arthritis. Arthritis & Rheumatism, 23(2), 146-152. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780230203
- Fries, J. F., Spitz, P., Kraines, R. G., & Holman, H. R. (1980). Measurement of patient outcome in arthritis. Arthritis & Rheumatism, 23(2), 137-145. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780230202
- McInnes, I. B., & Schett, G. (2011). The pathogenesis of rheumatoid arthritis. New England Journal of Medicine, 365(23), 2205-2219. https://www.nejm.org/doi/full/10.1056/NEJMra1004965