The lower limbs are made up of a set of 4 bones and a variety of muscles and ligaments that allow biomechanical movements without great effort. The legs are responsible for supporting the entire body weight and articulating the hip, knee and feet. As a result, leg injuries are frequent due to the work they do.
We will show you below the most recurrent leg diseases and which complementary therapies are applied to reduce the pain. We invite you to read on because you will find the best products to alleviate leg discomfort.
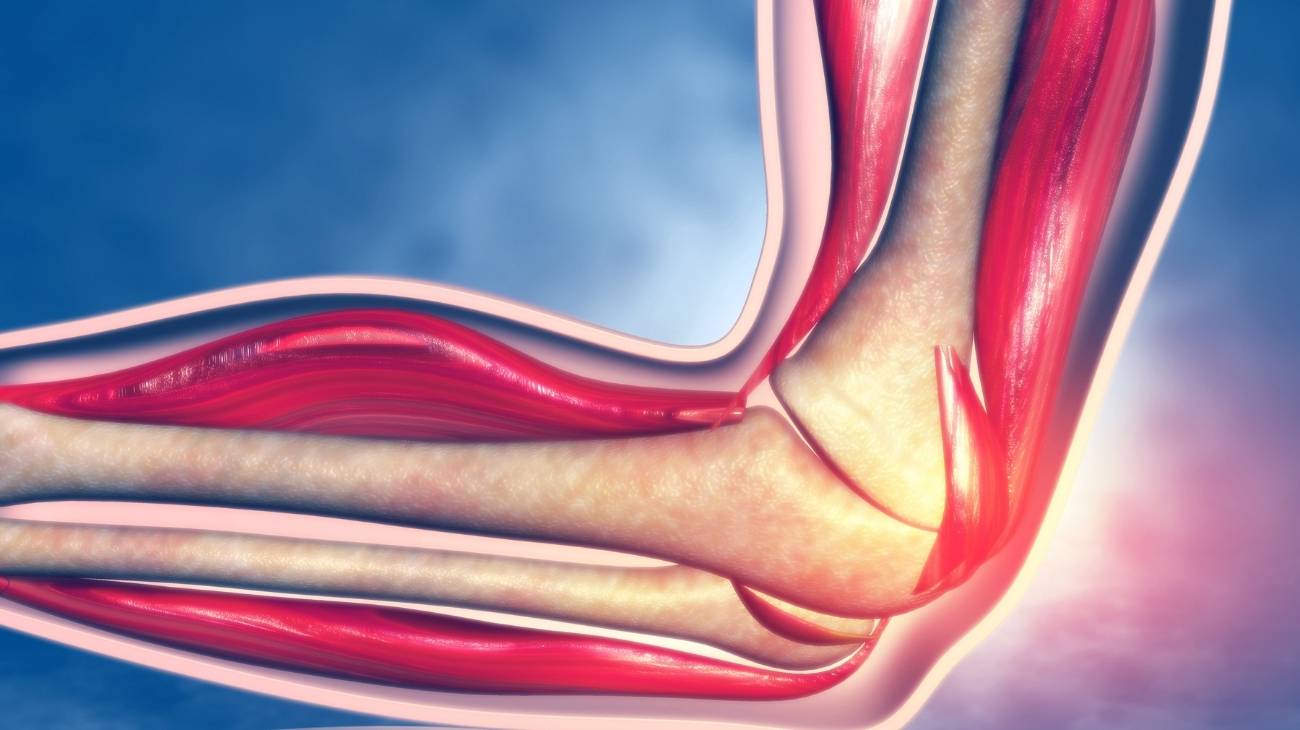
Parts and anatomy of the leg
The anatomy of the leg is made up of the following tissues:
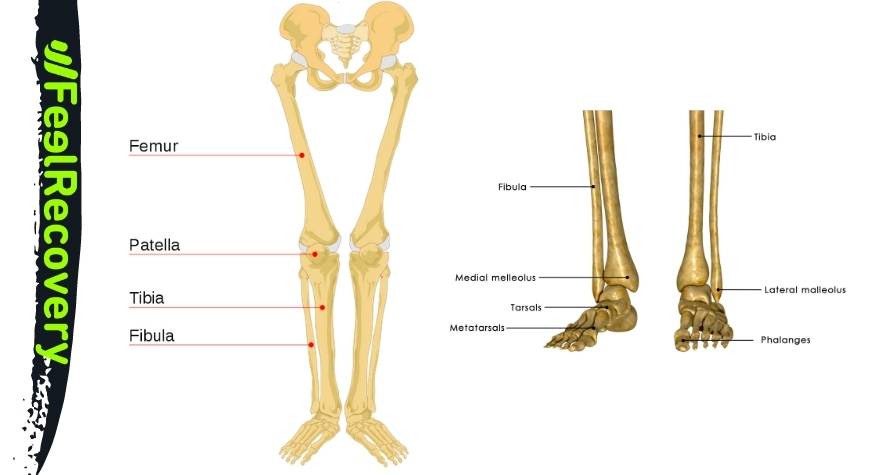
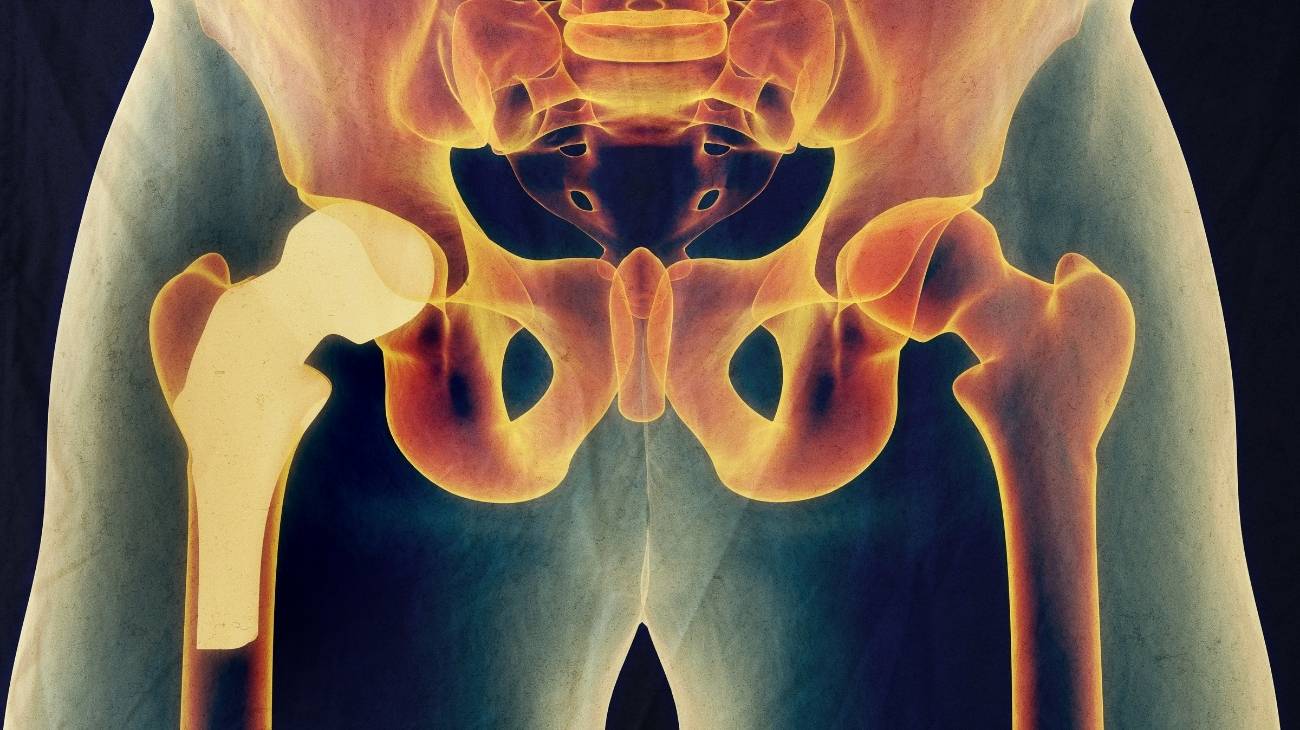
Bones and joints
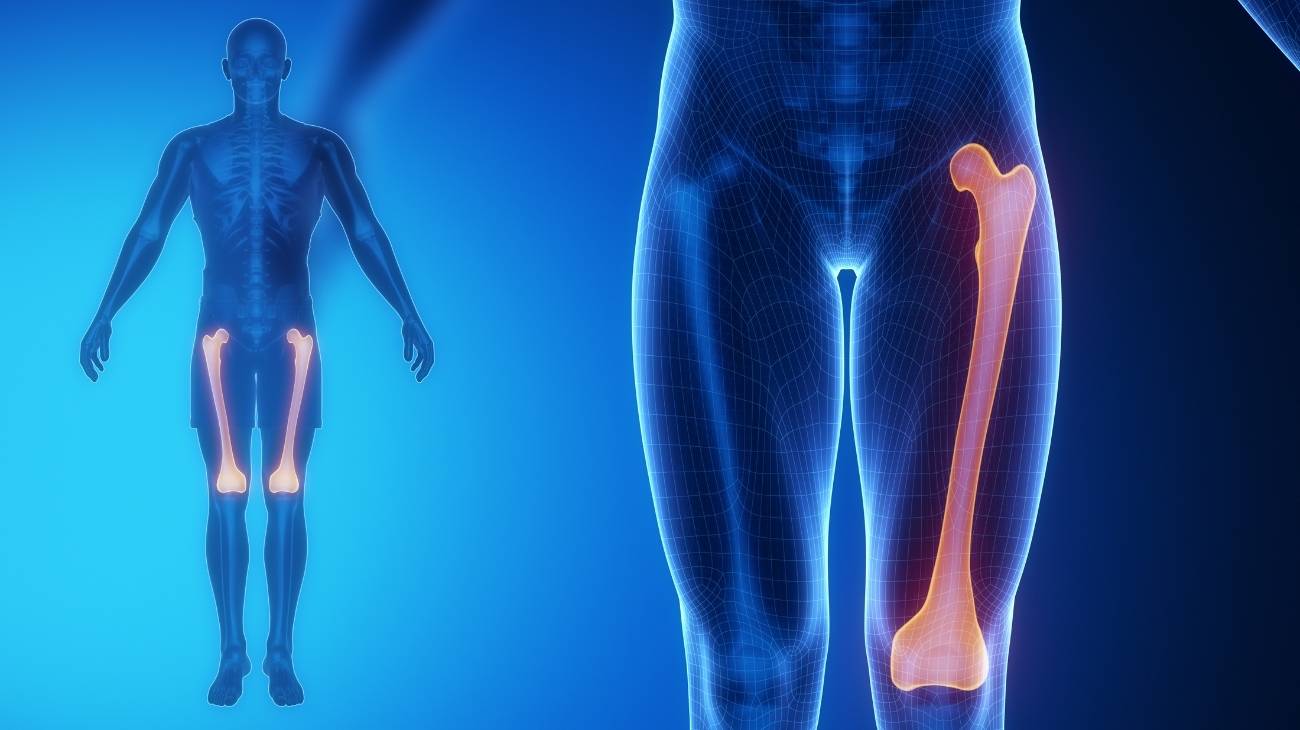
The bones that belong to the leg are:
- Femur: It is the longest and strongest bone in the human anatomy. It forms part of the coxofemoral joint, inserting itself into the acetabulum cavity by means of the femoral head and the knee joint by means of the trochlea of the tibia.
- Patella: lies in front of the femur and articulates with this bone by means of the terminal tendon, related to the quadriceps femoris.
- Fibula: This elongated bone has three sides and runs along the outside of the leg. The styloid process forms part of the knee joint, while the lateral malleolus forms part of the talus of the ankle.
- Tibia: Another elongated S-shaped bone. It is integrated into the knee joint through the proximal epiphysis, while the distal epiphysis is part of the ankle joint.
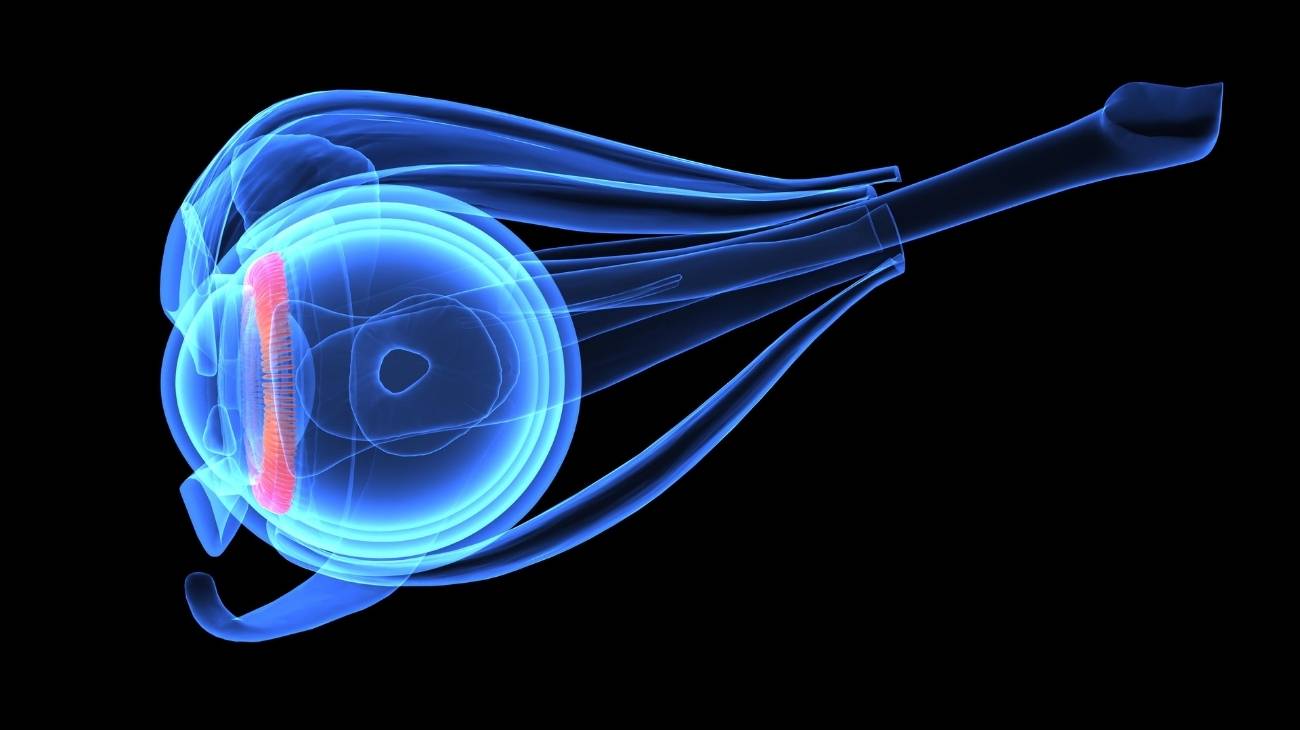
The joints that are in the leg are shown below:
- Knee: This joint joins the femoral condyles with the patella and the upper part of the tibia. It is possible to find the intercondylar fossa, the cruciate ligaments, the menisci and the transverse ligament.
- Tibioperonea superior: This articular body moves the lateral tuberosity of the tibia with the fibula, joined by ligaments.
- Intermediate tibioperoneal: The fibula is connected to the tibia by a membrane.
- Inferior tibioperoneal: This joint takes the lower part of the tibia and fibula.
- Tibioperoneoastotalar: The talus, malleoli and tibia join at this joint to give movement to the ankle. It can also be considered part of the foot.
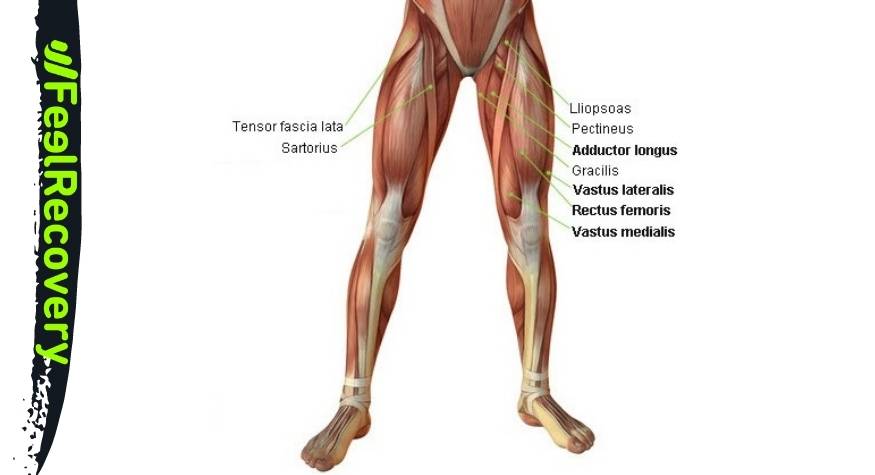
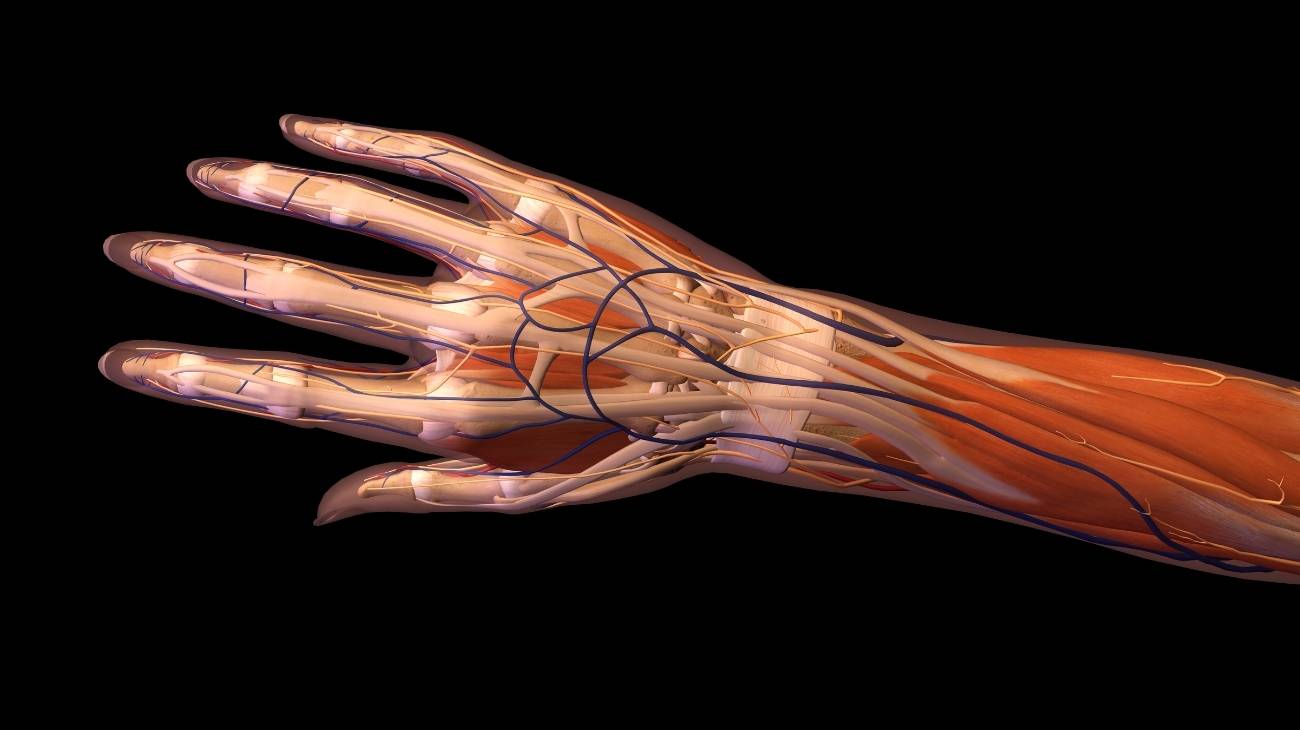
Muscles
Next, we will show you the muscles that are part of the leg:
- Sartorius: The longest muscle in the body, originating from the anterior superior iliac spine and ending on the upper surface of the tibia. Its action is to flex the hip and knee, taking into account the position of the femur.
- Vastus lateralis: It is part of the muscles called quadriceps femoris together with vastus medialis, cruralis and rectus femoris. It arises from the fibrous membrane of the greater trochanter of the femur to the quadriceps tendons. Its action is to stabilise the knee in extension.
- Rectus femoris: It runs from the iliac spine to the quadriceps tendon to allow coordinated knee extension and hip flexion.
- Vastus medialis: Its pathway is from the intertrochanteric line of the femur to the patellar tendon. This allows extension of the knee.
- Crural: From the lateral anterior part of the femur to the patellar ligament, this muscle can be seen. It is an extensor of the leg.
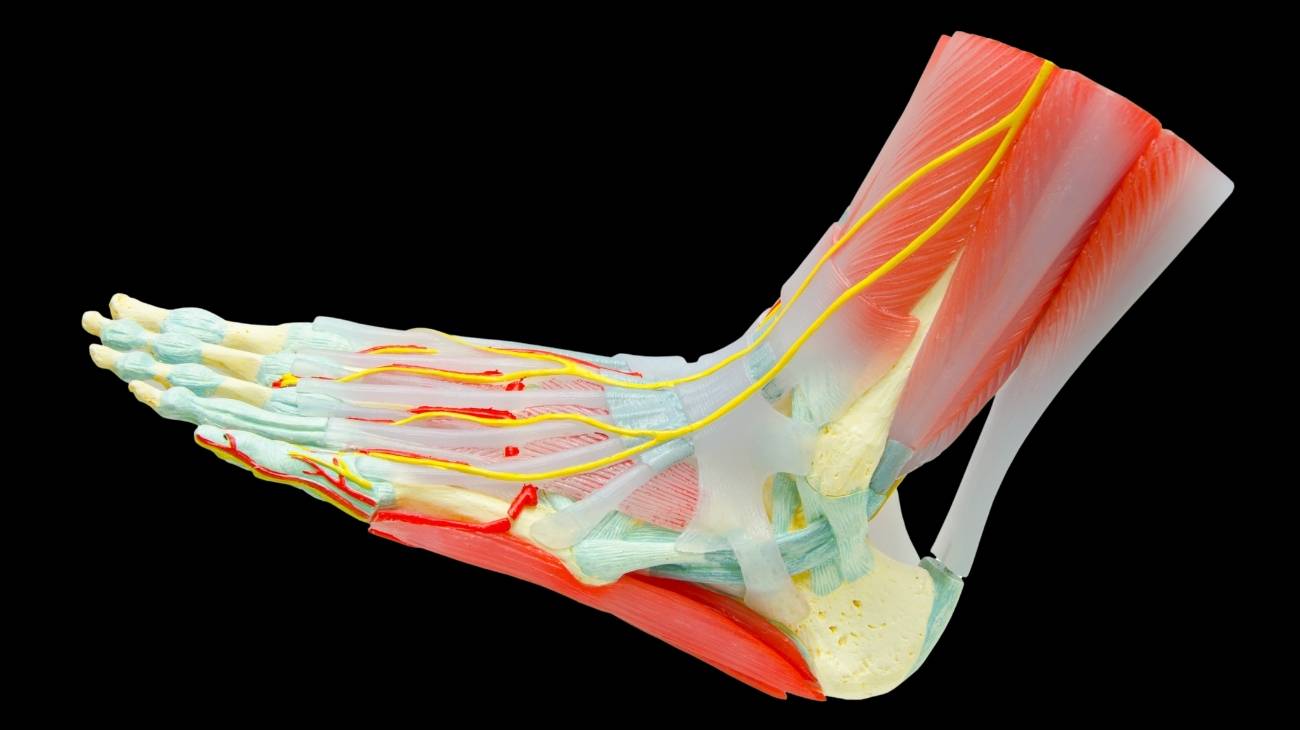
- Peroneus longus: The external tuberosity of the fibula gives rise to this muscle which inserts on the cuneiform plantar aspect and on the first metatarsal.
- Peroneus brevis: Located on the lateral side of the fibula, it arises below the knee and inserts on the external aspect of the fibula and on the fifth metatarsal. Rotation and abduction of the foot are generated by this muscle.
- Peroneus anterior: It arises from the fibula and inserts on the fifth metatarsal. Its function is to allow eversion of the foot and dorsal flexion.
- Tibialis anterior: located in the lower part of the leg, on the anterior side. Its course begins at the interosseous membrane and on the surface of the tibia to the medial underside of the medial cuneiform and the first metatarsal bone. Inversion and flexion of the foot is the action generated by this muscle.
- Posterior tibialis: Its elongated shape allows it to run from the tibia and fibula to the medial cuneiform and to the second, third and fourth metatarsal bones. Flexion, plantar adduction and foot stability are tasks of this muscle.
- Popliteus: Responsible for flexion of the leg at the knee. It arises from the condyle of the femur and inserts into the upper tibia.
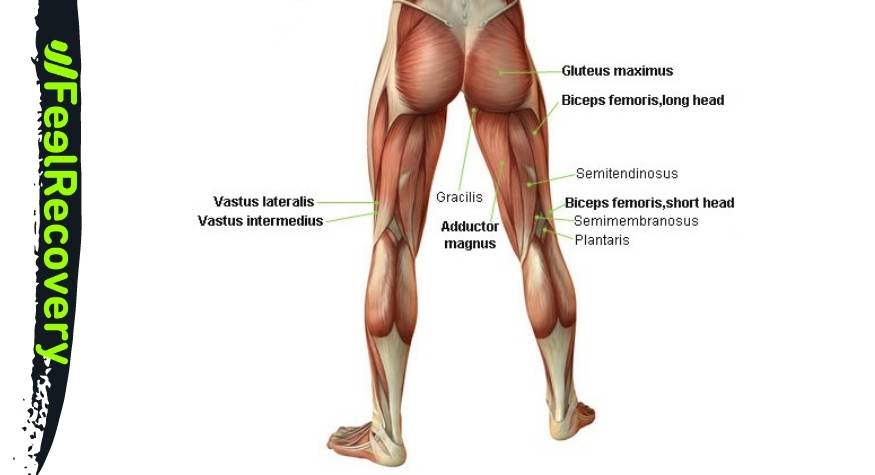
- Semimembranosus: Belongs to the hamstring group, together with biceps femoris and semitendinosus. It arises from the ischium and inserts on the medial condyle of the tibia bone. Its action allows extension of the hip and flexion of the knee.
- Semitendinosus: Its course begins at the tuberosity of the ischium and ends at the medial surface of the tibia, at its upper end. As it passes through the hip and knee, it allows the leg to flex and keep the hip extended.
- Biceps femoris: It runs from the ischial tuberosity to the fibula. It allows rotation and flexion of the knee and extension of the hip.
- Adductor: It arises from the ischium and inserts into the femur. It can be divided into three sections; major, medial and minor. Its function is related to the movement of the thigh.
- Inner gastrocnemius: Also known as the calf muscle, the condyles of the femur give rise to this muscle until it reaches the calcaneus of the foot.
- External gemellus: It has the same route as the previous muscle, but its action is to plantar flex the foot.
- Soleus: Together with the gastrocnemius, they form the so-called triceps suralis muscle. It is found at the back of the leg, as it arises from the fibula and tibia and fits into the calcaneus.
- Flexor hallucis longus: These muscles start at the tibia and insert into each of the phalanges of the toes to achieve flexion.
- Flexor hallucis longus: The origin of this muscle is the last part of the fibula and inserts into the posterior phalanx of the big toe. Its task is to allow flexion of this toe.
- Plantar: The external supracondylar crest of the femur, which inserts on the Achilles tendon (on the inside). Plantar flexion of the foot and knee are the actions performed by this muscle.
- Extensor longus: Pure work to allow dorsiflexion of the foot dorsally and extension of the big toe. It arises from the medial area of the fibula and inserts into the distal phalanx of the big toe.
- Extensor digitorum: The action of this muscle is to produce extension of the toes, except for the big toe. The tibia and fibula are the bones from which it originates.
- Gracilis muscle: Also known as rectus internus. It originates in the ischium and ends in the tibia. Its action controls the movements of the hip.
Ligaments
The ligaments found in the leg are as follows
- Lateral collateral: It is located on the outer side of the knee joint and connects the femur to the fibula bone.
- Medial collateral: This ligament runs along the inside of the knee, connecting the fibula to the femur.
- Patellar: It is located in the knee and is known to be the continuation of the quadriceps femoris muscle group. It runs under the patella, inserting into the patella and the tibia.
- Anterior cruciate: The job of this ligament is to prevent the tibia from moving forward, so it joins the femur on its upper lateral part with the medial section of the tibia, on its anterior side. It passes under the patella.
- Posterior cruciate ligament: Unlike the anterior ligament, this tissue prevents the tibia from moving backwards with respect to the femur. It is often torn during strenuous activity.
- Transverse: Also known as the jugal ligament due to its action of joining the menisci on their anterior sides.
- Meniscofemoral: It is possible to find this ligament under the name of Humphrey. It is responsible for joining the femoral condyle (on its inner side) to the external meniscus.
- Posterior meniscofemoral or Wrisberg's ligament: In this case, this tendinous tissue joins the internal condyle of the femur bone with the meniscofemoral ligament.
- Popliteus obliquus: This is a ligament that runs from the external condyle of the femur to the semimembranosus.
- Popliteus arcuate: The origin of this ligament is the same as that of the oblique ligament, but it inserts on the head of the fibula.
- Alar patellar: It runs from the inner aspect of the femur to the patella.
- External patellar alar: The external condyle of the femur is attached by this ligament to the edge of the patella.
- Internal patellar meniscus: The internal meniscus is attached to the patella by this ligament.
- Internal lateral: Also known as the tibial collateral. Its function is to attach the femur to the tibia.
- External patellar meniscus: The function of this ligament is to attach the external meniscus to the patella.
- Patellofemoral: It is responsible for keeping the lateral displacement of the patella balanced. It develops in the middle part of the femur (from a distal view) to the patella.
- Iliofemoral: This ligament belongs to the hip joint, but attaches at the femur so it can also be considered a ligament of the leg. It is also known as Bigelow's ligament.
- Ischifemoral: As in the previous case, this tissue belongs to the hip, joining the ischium with the femur, so it is possible to place it within the group of ligaments of the legs.
- Femoral head or round: The femoral head joins the diaphysis of the pelvis by means of this ligament to form the hip joint.
Best products for leg pain relief
Bestseller
-
2 Knee Compression Sleeve (Black/Gray)
£20,95 -
2 Knee Compression Sleeve (Green/Navy)
£20,95 -
2 Knee Compression Sleeve (Pink/Bordeaux)
£20,95 -
2 Thigh Compression Sleeve (Green/Navy)
£20,95 -
2 Thigh Compression Sleeve (Pink/Bordeaux)
£20,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Hearts)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Oxford)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Sport)
£24,95 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Hearts)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Oxford)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Sport)
£20,95
-
2 Calf Compression Sleeve (Black/Gray)
£20,95 -
2 Calf Compression Sleeve (Green/Navy)
£20,95 -
2 Calf Compression Sleeve (Pink/Bordeaux)
£20,95 -
2 Patella Knee Strap (Black/Gray)
£12,95 -
2 Patella Knee Strap (Green/Navy)
£12,95 -
2 Patella Knee Strap (Pink/Bordeaux)
£12,95 -
2 Thigh Compression Sleeve (Black/Gray)
£20,95 -
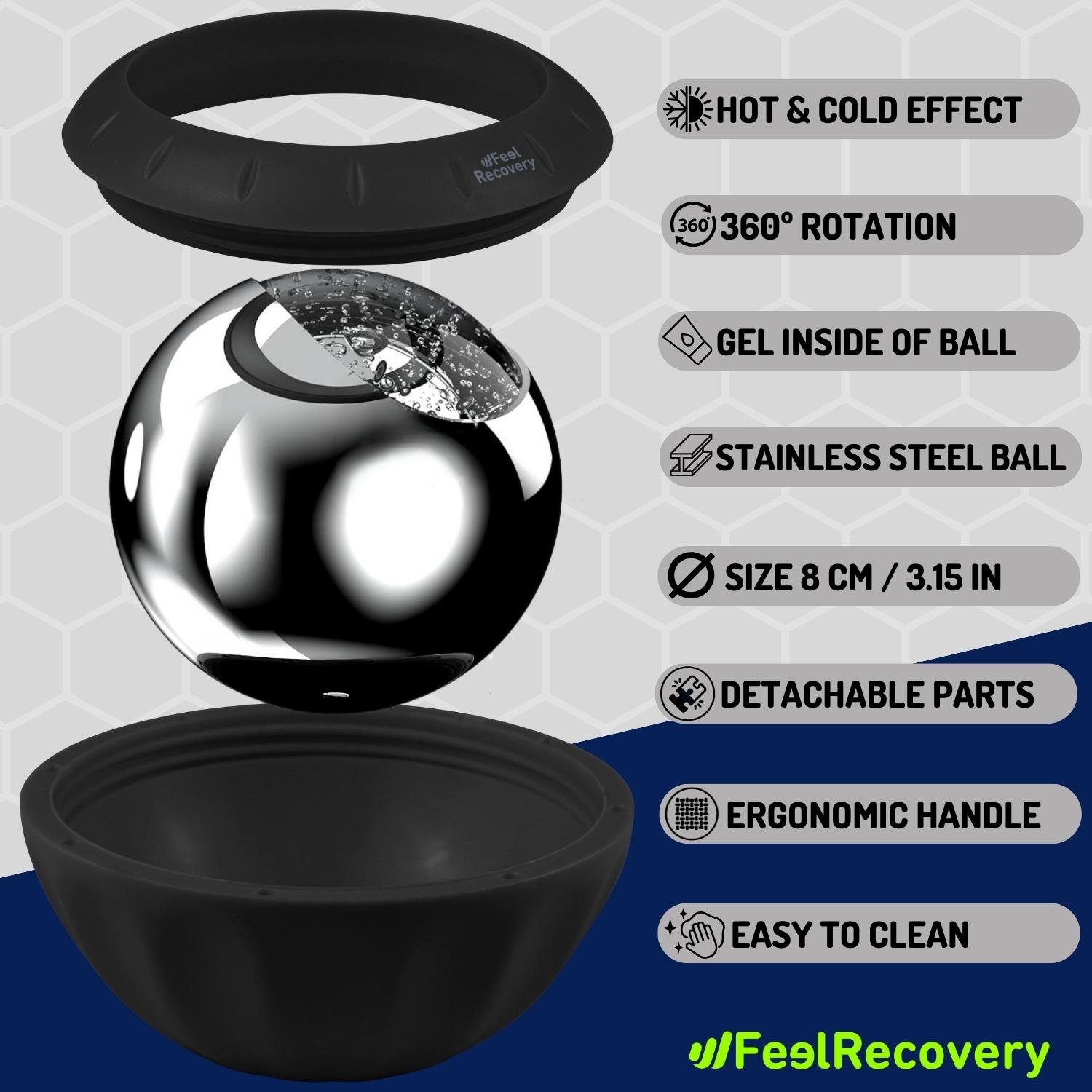
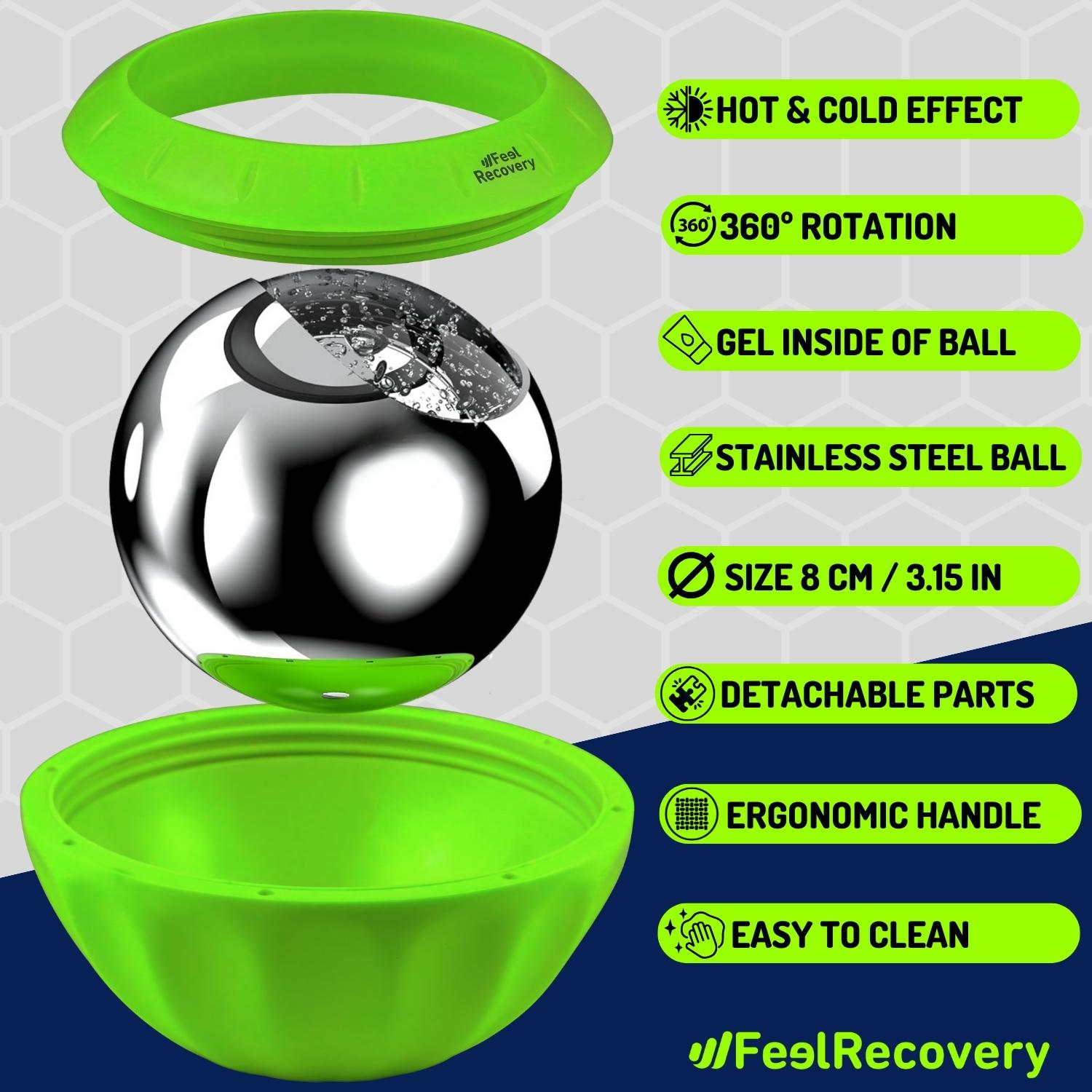
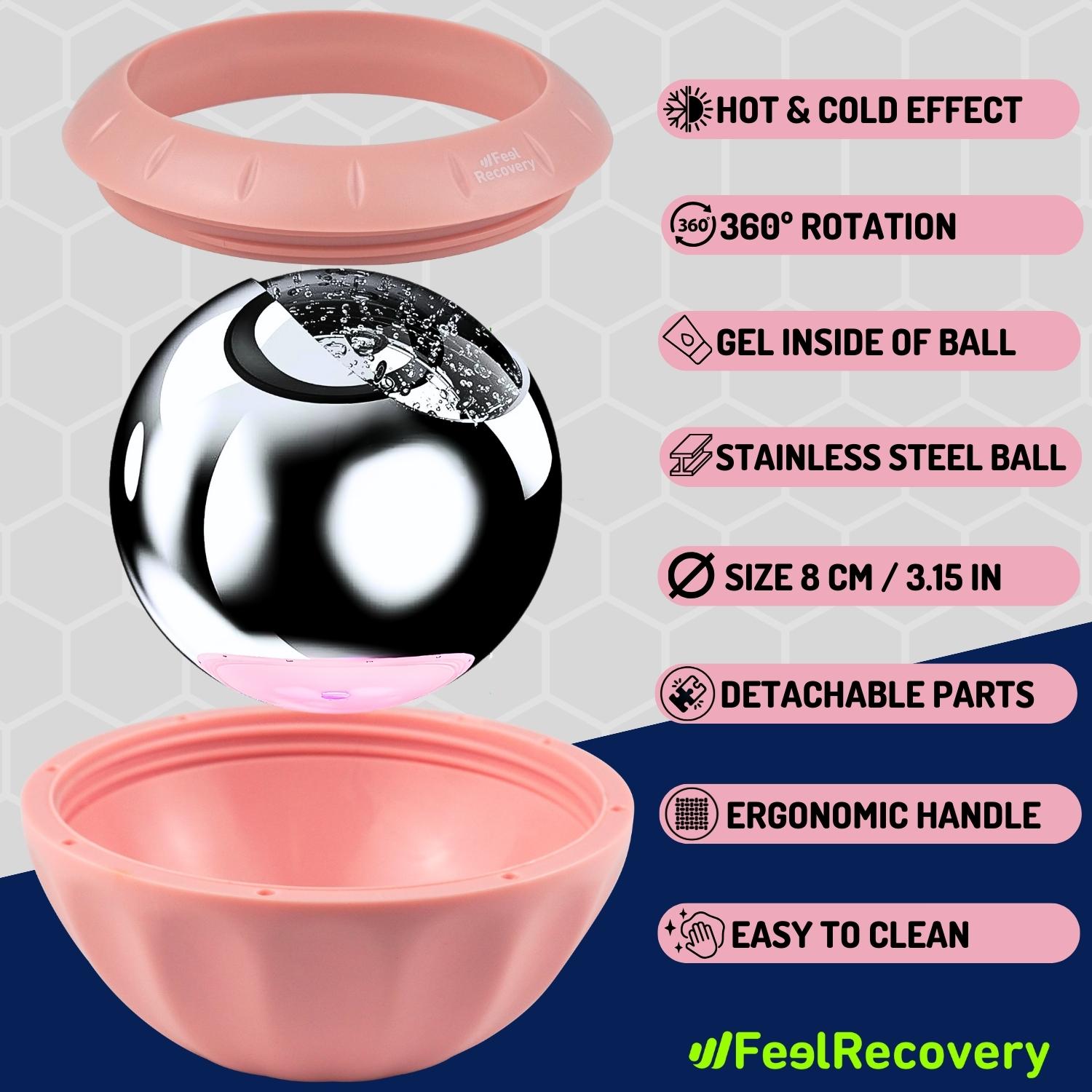
Ice Massage Roller Ball (Black)
£34,95 -
Ice Massage Roller Ball (Green)
£34,95 -
Ice Massage Roller Ball (Pink)
£34,95 -
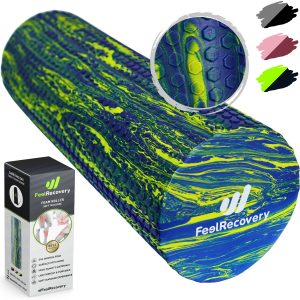
Soft Density Foam Roller for Recovery (Black)
£34,95 -
Soft Density Foam Roller for Recovery (Green)
£34,95 -
Soft Density Foam Roller for Recovery (Pink)
£34,95 -
Sport Compression Socks (1 Pair) (Black/Gray)
£20,95 -
Sport Compression Socks (1 Pair) (Green/Navy)
£20,95 -
Sport Compression Socks (1 Pair) (Pink/Bordeaux)
£20,95
Biomechanics of the leg
The biomechanical movements that the legs can perform are
- Flexion: Consists of lifting the knee to the trunk and keeping the knee extended or flexed. The maximum opening angle of this movement is around 110 to 130°. This is produced by the displacement of the condyles of the tibia and the menisci, maintaining the limit established by the posterior cruciate ligament.
- Extension: This is a movement that is performed when the leg is brought backwards. The opening does not exceed 30°.
- Abduction: Taking the external part of the pelvis as the axis, it is possible to move the leg in front of the other leg in the direction of the other leg by up to 30°. In other words, it is a matter of placing one knee in front of the other, keeping one foot on the floor.
- Adduction: This is the opposite movement to abduction, as in this case the leg is placed on the outside of the trunk and lifted up to 180° with a lot of training. In this movement, the foot remains next to the head.
- Internal rotation: This consists of placing the foot backwards and bending the knee by turning it towards the inside of the body. This opening does not exceed 40°. The sartorius, semitendinosus, semimembranosus, biceps femoris and rectus femoris are the muscles that produce this movement.
- External rotation: By placing the foot backwards and extending the knee to the outer side of the trunk, the biomechanical movement that bears this name is performed. The opening limit is 45°.
Most common leg injuries
The legs are one of the parts of the human body that suffer most from injuries, and for this reason we will show you below what the most common leg injuries are.
Types of leg injuries
Take a look at the different types of leg injuries that can occur:
- Muscle cramps in the legs and calves: This condition occurs due to a lack of calcium, magnesium and potassium in the tissues of the legs and calves. It can also be caused by trauma or severe blows to the affected area. The quadriceps, hamstrings and gastrocnemius are the most affected muscles when repetitive and demanding activities are performed.
- Muscle contractures in the legs and thighs: The involuntary tension caused in the muscular tissues of the gluteal area and legs is produced by the lack of elimination of metabolic molecules that remain lodged in these structures, sedentary lifestyles, sudden movements and demanding tasks.
- Leg sprains: Small cuts and tears in the cruciate, patellar, collateral and meniscofemoral ligaments are the most common leg injuries in the knee area. While in the ankle and hip joint area, the ischiofemoral, lateral and peroneus-astragalis tissues are the most common to suffer sprains.
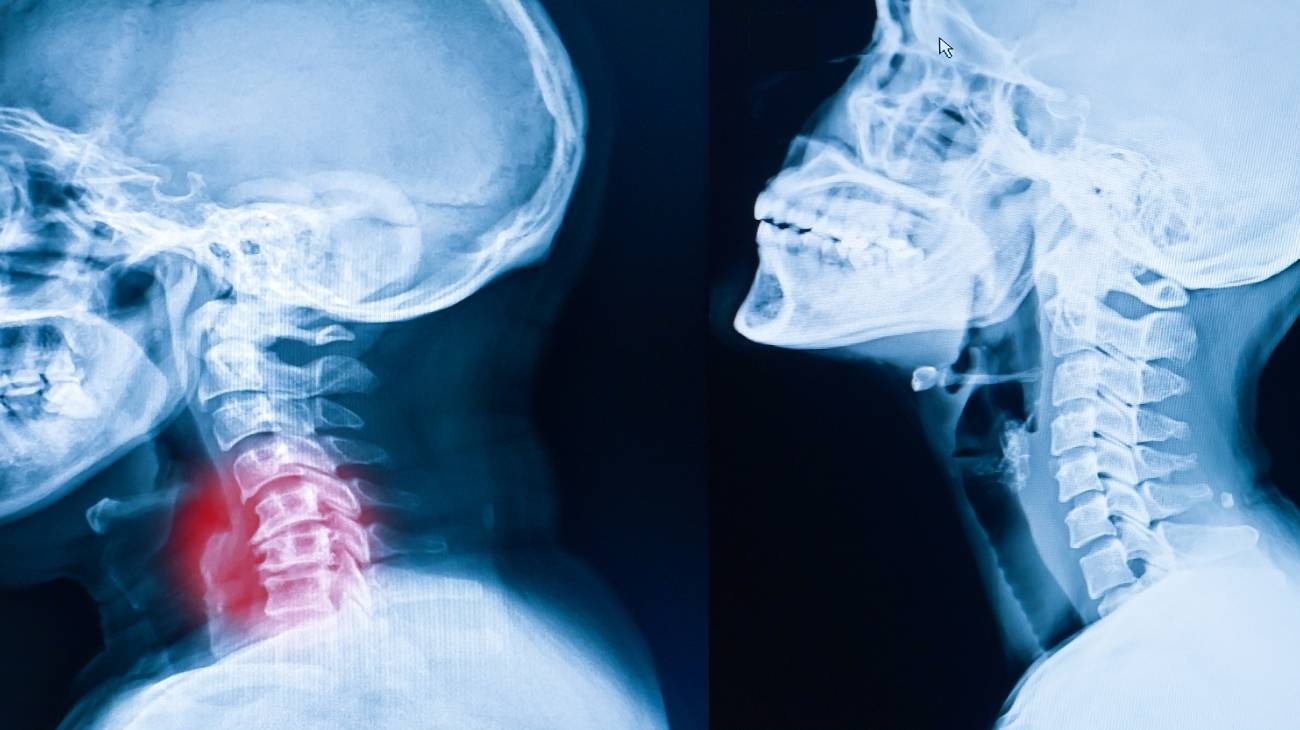
- Fractures of the leg: The leg is an area that is very prone to breakage due to the length of its bones. Therefore, falls and trauma sustained in sporting activities and everyday tasks are the main cause of this condition.
Sports leg injuries
Sports also cause bruises and trauma to the legs. Find out which are the most common:
- Foot, ankle and leg injuries in basketball: Lower tibioperoneal, deltoid, collateral, cruciate and patellar sprains are the ligaments that suffer the most from involuntary stretching. On the other hand, Achilles bursitis, Achilles tendonitis, muscle contractures in the sartorius, quadriceps femoris and adductors are also common. Fractures are frequent in the lower tibia and fibula.
- Knee and leg injuries in cycling: Patellar bursitis and inflammation of other bursae of the knee are the most common conditions suffered by these athletes, although calf and quadriceps contractures are also common. Fractures of the femur, tibia and fibula are not common, but can occur in group falls. Cruciate and collateral cruciate sprains can occur.
- Leg injuries in football: Ruptured cruciate and lateral ligaments, together with hamstring, quadriceps and calf contractures are the most common contusions suffered by people who play this sport. Bone cracks are not common, but there are cases of broken tibia and fibula.
- Running leg injuries: The patellar tendon, meniscus and knee ligaments are often sprained. Muscle overload causes the quadriceps, adductors, hamstrings and calf muscles to tighten involuntarily during a run. Fractures of the femur, tibia and patella are the most common fractures.
Diseases and ailments in the legs
Among the most common ailments and diseases of the legs are the following:
Cellulitis
This condition affects the middle layer of the skin, called the dermis. It is caused by the appearance of bacteria that live on the skin, the most common agents being streptococcus and staphylococcus.
Peripheral artery disease
This is a common disease characterised by the accumulation of fatty elements within the arteries, causing narrowing of the arterial channel and arterial stiffness. This can be caused by smoking, a history of coronary heart disease and diabetes.
Varicose veins
This is a chronic venous insufficiency, which dilates and twists the veins in the legs. Their presence can be seen with the naked eye, as varicose veins turn blue or green. And the exact causes are not known, but generally advanced age and obesity are risk factors.
Gout
Uric acid must be eliminated through the blood, so excess uric acid generates microcrystals in the joints causing great pain and inflammation in the legs. This leads to joint malfunction and the development of osteophytes.
Venous thrombosis
The presence of a blood clot within a deep vein in the leg gives rise to this disease. It is a relatively serious condition mainly caused by smoking, surgery, obesity and age of the patient. It is also known as peripheral vascular disease (PVD).
Osteomyelitis
This bone infection is caused by bacteria, fungi and other micro-organisms causing a large infection between the skin, muscles and bones of the leg.
How can we relieve leg pain through complementary and non-invasive therapies?
It is possible to relieve leg pain through complementary and non-invasive therapies, which we mention below.
Heat and cold therapy
The sensation of pain, stiffness and swelling in the legs can be reduced by means of heat and cold therapy. This treatment consists of applying each temperature for no more than 5 minutes to obtain the benefits of both. In this way, the area is deflated and the capillaries are dilated without risk of injury to the skin. Cold gel packs and thermal pillows are used for this treatment, although ice and warm water can also be used.
Compression therapy
Compression therapy helps to keep the skin in one place to improve joint movements and to rest the tissues. It also allows better blood flow, which reduces swelling and redness. There are different techniques that can be applied, the most recommended being those that include knee braces, calf sleeves, compression socks and stockings and patella knee strap. Although it is also possible to find patients who have been advised by their doctors to use elastic bandages and thigh braces.
Massage therapy
This therapy can be applied by a professional or by using products that help with self-massage. Electric cushions, massage chairs, electric guns to massage the muscles or massage rollers are used for this task. This treatment stimulates the muscle and tendon tissues, which helps to decompress the involuntary tensions present by dilating the blood flow. This process results in the exchange of oxygen with the affected fibres.
Acupressure therapy
Acupressure is a technique based on the controlled pressing of different points on the body in order to develop emotional and mental balance in the patient. This results in the relaxation of muscles and tendons, which significantly improves the overall well-being of the patient. This can be done by using articles that help with this therapy or by choosing a therapist to perform the task, the first option being much more economical. This is why the use of acupressure mats and cushions are the most recommended products in this non-invasive therapy.
Thermotherapy
The use of heat in a treatment helps the arterioles and venules of the leg to dilate to cause a better exchange of nutrients and gases between the blood and the fibres of the tissues in this part of the body. Thanks to this complementary and non-invasive therapy it is possible to reduce inflammation and pain in a short time. For this purpose, thermal pillows are used which are heated in the microwave to achieve the ideal temperature. The 3 or 4 daily sessions should not exceed 15-20 minutes in order to obtain the best results.
Cryotherapy
The anti-inflammatory and relaxing effects of cold can be achieved by cryotherapy. This complementary treatment consists of using cold gel pads, ice packs or ice water on the affected area for 15 minutes. It is necessary to consult a doctor before choosing this therapy to find out if it is applicable in each case.
Electrical muscle stimulation (EMS)
Muscle electrostimulation, or EMS, is a therapy that consists of stimulating muscle contractions through the use of electricity, so as to achieve an effect of activity and hypertrophy as in the gym, but without the need to go to any sports center. This means that you can put your muscles to work without leaving home.
Electrotherapy
This is a technique that seeks relief from pain and some physical ailments through the application of electrical and electromagnetic energy, among other variants, through the skin with the use of conductive pads called electrodes. It is a very safe type of therapy and must be applied by a physical therapist specialized in the manipulation of electricity to treat some kinds of ailments.
Myofascial release therapy
Also known as myofascial induction, this therapy consists of the application of manual massage to treat the shortening and tension generated in the myofascial tissue that connects the muscles to the bones and nerves. For this purpose, various massage techniques are used that focus on the so-called trigger points.
Percussion Massage Therapy
Vibration or percussion massages are precise, rhythmic and energetic strokes on the body to achieve relief from some annoying symptoms when muscle fibers are tightened, often by a high workload on them and that has left trigger points in the muscle fibers.
R.I.C.E Therapy
The R.I.C.E. therapy is the first and simplest of the treatment protocols for minor injuries. It appears in the sports field to deal with accidents involving acute injuries. For many years, it has been considered the most suitable for its speed and results.
Trigger points therapy
Myofascial pain points or trigger points are knots that are created in the deeper muscle tissues, causing intense pain. The pain does not always manifest itself right in the area where the point develops, but rather this pain is referred to nearby areas that seemingly do not appear to be related. In fact, it is estimated that more than 80% of the pain they cause manifests in other parts of the body.
Other effective alternative therapies
In addition to the non-invasive complementary therapies mentioned above, there are other treatments that can also be applied to reduce leg pain.
- Natural remedies using plants: This is a non-invasive treatment that consists of choosing natural herbs and plants that contain anti-inflammatory and sedative chemical components. In this way it is possible to apply baths with warm water or prepare infusions of linden, chamomile, willow bark and lemon balm, among others. It can also be applied externally by means of ointments, as is the case with the use of aloe vera.
- Acupuncture: By means of the insertion of special needles in different parts of the body, the patient's relaxation can be achieved to reduce the involuntary tension of the tissues in the affected area. This will help to reduce pain and inflammation.
- Kinesiotherapy: This therapy is widely used to bring the pain in the legs into remission. This is achieved through exercises, massages and controlled movements of the limbs by the kinesiologist. This stimulates the exchange of nutrients between the tissues and the blood.
- Aromatherapy: The generation of aromas by means of oils or mixtures of different fluids helps people with leg injuries to improve their mental attitude towards the symptoms they suffer from. Its use is very simple, the liquids are applied in handkerchiefs, in candles or by means of electrical products that pressurise the aromatic combination. Citrus fruits, mint and ginger are often chosen for this treatment.
- Osteopathy: This medicinal technique, which has not been scientifically proven, consists of generating movements and massaging the affected area to stimulate the muscle and bone structure. This therapy naturally reduces pain and numbness. For this reason, it cannot be used if the injuries occur in the bursae or ligaments. It is advisable to consult a doctor before choosing a treatment.
References
- Fukunaga, T., Roy, R. R., Shellock, F. G., Hodgson, J. A., Day, M. K., Lee, P. L., ... & Edgerton, V. R. (1992). Physiological cross‐sectional area of human leg muscles based on magnetic resonance imaging. Journal of orthopaedic research, 10(6), 926-934. https://onlinelibrary.wiley.com/doi/abs/10.1002/jor.1100100623
- Marieb, E. N., & Hoehn, K. (2007). Human anatomy & physiology. Pearson education. https://books.google.es/books?hl=en&lr=&id=x1uEB68iitwC
- Edgerton, V. R., Smith, J. L., & Simpson, D. R. (1975). Muscle fibre type populations of human leg muscles. The Histochemical Journal, 7(3), 259-266. https://link.springer.com/article/10.1007/BF01003594
- Behrman, A. L., & Harkema, S. J. (2000). Locomotor training after human spinal cord injury: a series of case studies. Physical therapy, 80(7), 688-700. https://academic.oup.com/ptj/article/80/7/688/2842518
- Blue, J. M., & Matthews, L. S. (1997). Leg injuries. Clinics in sports medicine, 16(3), 467-478. https://www.sciencedirect.com/science/article/abs/pii/S0278591905700351
- Gallo, R. A., Plakke, M., & Silvis, M. L. (2012). Common leg injuries of long-distance runners: anatomical and biomechanical approach. Sports health, 4(6), 485-495. https://journals.sagepub.com/doi/abs/10.1177/1941738112445871
- Söderman, K., Alfredson, H., Pietilä, T., & Werner, S. (2001). Risk factors for leg injuries in female soccer players: a prospective investigation during one out-door season. Knee Surgery, Sports Traumatology, Arthroscopy, 9(5), 313-321. https://link.springer.com/article/10.1007/s001670100228
- Clanton, T. O., & Solcher, B. W. (1994). Chronic leg pain in the athlete. Clinics in sports medicine, 13(4), 743-759. https://europepmc.org/article/med/7805104
- Willems, T. M., De Clercq, D., Delbaere, K., Vanderstraeten, G., De Cock, A., & Witvrouw, E. (2006). A prospective study of gait related risk factors for exercise-related lower leg pain. Gait & posture, 23(1), 91-98. https://www.sciencedirect.com/science/article/abs/pii/S0966636204002747
- Edwards Jr, P. H., Wright, M. L., & Hartman, J. F. (2005). A practical approach for the differential diagnosis of chronic leg pain in the athlete. The American Journal of Sports Medicine, 33(8), 1241-1249. https://journals.sagepub.com/doi/abs/10.1177/0363546505278305