- What is subacromial bursitis of the shoulder?
- What are the causes and risk factors for shoulder bursitis?
- Best products for shoulder bursitis
- Main symptoms that warn us that we have bursitis of the shoulder
- What treatments are there to improve the symptoms of shoulder bursitis?
- Which methods of prevention for shoulder bursitis are the most effective?
Inflammation occurring in the subacromial bursa can lead to limitations in shoulder movement. This is caused by a number of factors, the most common being strain on the affected area and overload on the body of the joint, leading to acute pain and muscle stiffness.
If you want to know more about shoulder bursitis, read on. We will explain each risk factor and the symptoms of shoulder bursitis in detail. But that's not all, you'll also find information on treatments that improve symptoms.
What is subacromial bursitis of the shoulder?
The shoulder joint is made up of the clavicle, acromion, scapula and humerus. These bones are connected by tendons that run to the deltoid, supraspinatus and biceps muscles. Below the acromion, over the supraspinatus and next to the deltoid is the subacromial bursa. This is a bursa that contains synovial fluid to cushion and soften shoulder movements.
For various reasons, this bursa can receive more fluid than the correct amount from the autoimmune system. This causes inflammation in the bursa, known as subacromial bursitis. This condition, when treated in time, can disappear within weeks without serious consequences. But until the condition goes into remission, the patient will suffer from pain, swelling and stiffness in the joint.
What are the causes and risk factors for shoulder bursitis?
The reasons that can increase the chances of developing subacromial bursitis are as follows
- Stressing the joint: heavy lifting or repetitive repetitive movements can put the bursa between the deltoid and supraspinatus at risk. This can cause both muscles to swell and thus the bursa has less space to lubricate the movements.
- Bone malformations: Bone spurs in the humerus, acromion, clavicle or scapula can cause the joint to become misaligned. This will cause the synovial bursa to stretch and accumulate fluid.
- Congenital deformities: it is common to find patients who were born with malformations in the affected area. This leads to frequent osteophytes and causes the joint to open poorly.
- Rheumatoid arthritis and osteoporosis: these types of degenerative diseases cause alterations in the tissues surrounding the synovial bursa. As time goes by, the bones erode causing the bursa located in the shoulder to suffer great pressure.
- Gout: this disease, caused by excess uric acid, causes microcrystals to appear in the joint body. Thus, it is common to find patients with joint malformations that cause inflammation in the bursa.
- Trauma and infections: this type of injury can cause blows to squeeze the synovial bursa, causing the immune system itself to generate more synovial fluid than necessary. On the other hand, when there are injuries caused by the same trauma, the likelihood of micro-organisms entering the bloodstream and lodging in this part of the body is high.
- Sedentary lifestyle: lack of activity in the shoulder means that the muscle-tendon structure does not stretch and remains stiff for a long time. When making sudden movements, both the deltoid and supraspinatus can be affected, leading to complications in the shoulder bursa.
- Poor nutrition: lack of vitamins and minerals in the body are risk factors that can lead to shoulder bursitis.
Best products for shoulder bursitis
Bestseller
-
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Hearts)
£24,95 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Oxford)
£24,95 -
Microwave Wheat Bag for Neck & Shoulder Pain Relief (Sport)
£24,95 -
Microwave Wheat Bag for Neck Pain Relief (Hearts)
£20,95 -
Microwave Wheat Bag for Neck Pain Relief (Oxford)
£20,95 -
Microwave Wheat Bag for Neck Pain Relief (Sport)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£20,95
Main symptoms that warn us that we have bursitis of the shoulder
To deal with this type of ailment, it is necessary to see a doctor as soon as possible. But to do so, you should know what are the symptoms and signs that will warn of the presence of an inflammation of the subacromial bursa located in the shoulder.
See below for the following signs
- Limited movement: one of the characteristic symptoms of this ailment is the inability to move the shoulder, especially when lifting the arm longitudinally to the body. This is due to inflammation in the affected area.
- Shoulder pain: this is another recurring sign in patients with shoulder bursitis. The subacromial bursa becomes so inflamed that it is pressed by the acromion, supraspinatus, deltoid and even the humerus. This causes the nerve roots in the area to send pain signals to the brain due to the malfunctioning of the joint.
- Inflammation: swelling in the shoulder may be found based on the amount of blood that is lodged in the area.
- Loss of sensation: lack of sensation and tingling in the shoulder are common symptoms that appear frequently in patients. This is also related to the central nervous system and lack of blood supply to the blood vessels.
- Fever: it is likely if the accumulation of blood in the affected area causes a rise in temperature in the shoulder.
- Muscle stiffness: both the supraspinatus and deltoid muscles, and in some cases the biceps, can be affected by self-generated tension. This is because the patient unconsciously stresses to avoid pain, causing contractions that can lead to acute pain.
- Lossof strength: the sensation of weakness is frequent in patients with this pathology, due to the malfunctioning of the muscles and the bursa located in the shoulder.
What treatments are there to improve the symptoms of shoulder bursitis?
There are different therapies and treatments that can be used to help bursitis go into remission. For this reason, we will show you below the techniques most recommended by doctors who specialise in these ailments. Take a look
Alternative and complementary therapies
Different variants of therapies can be applied to help complement the treatments used to reduce the symptoms of bursitis.
These include:
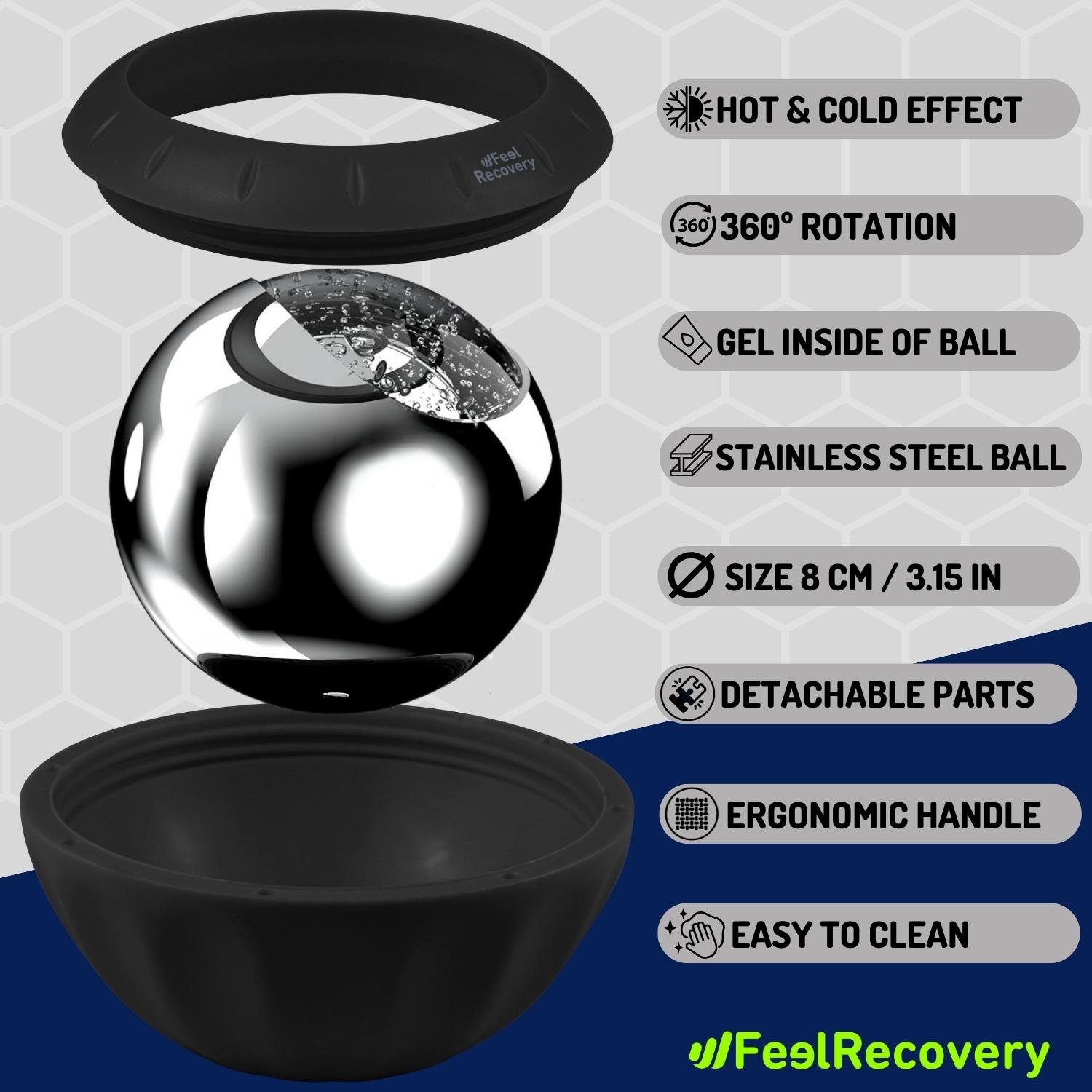
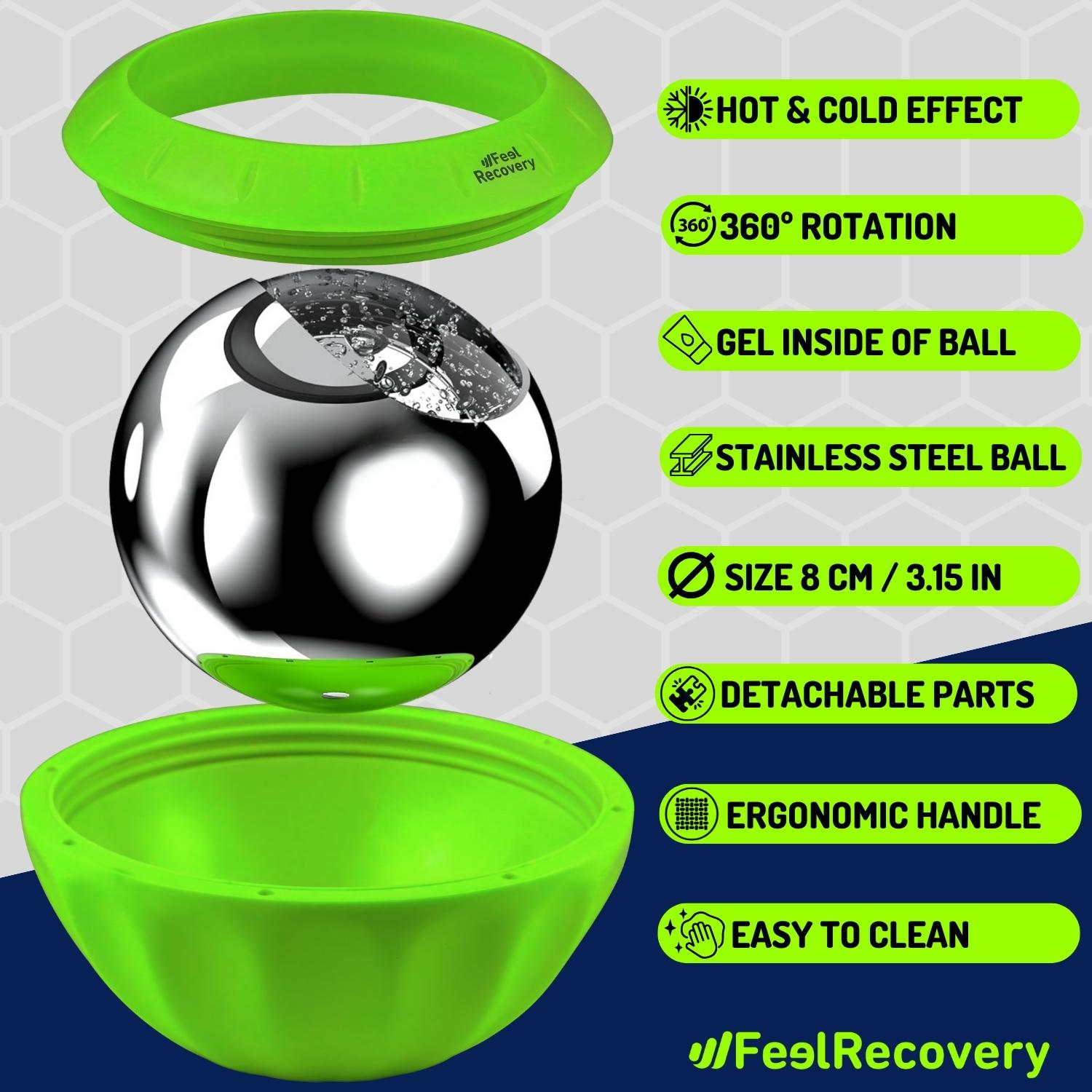
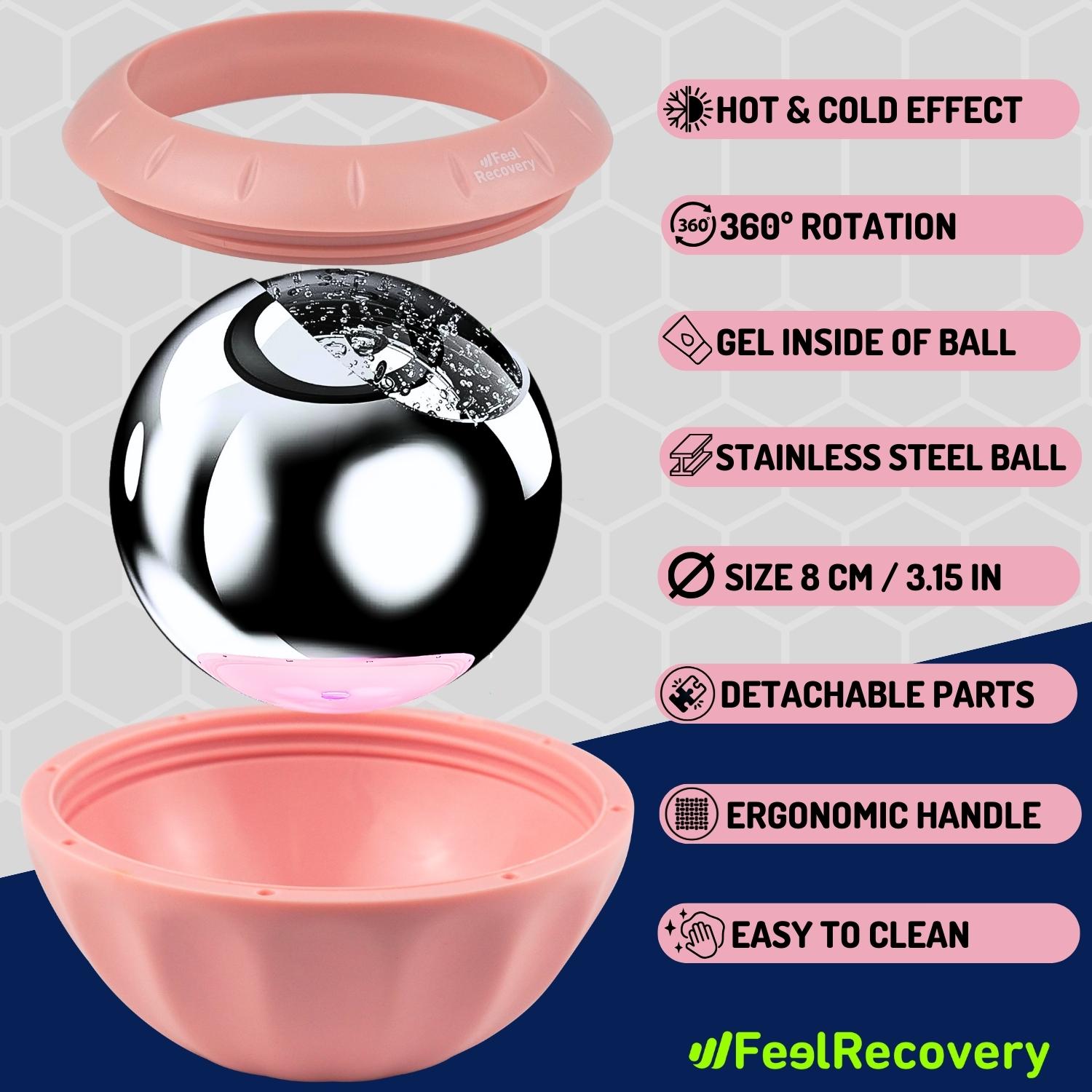
- Cold and heat therapy: this therapy consists of applying different elements that emit heat and cold, thus achieving the advantages of both thermal extremes. Its use cannot exceed 15 to 20 minutes and it starts with heat, continues with cold and ends again with a warm application. The electric blankets and hot water bags improve blood circulation, causing the pain to diminish, while the cold acts as a natural anti-inflammatory. The application of this treatment should be supervised by a professional to avoid epidermal burns.
- Compression therapy: Compression bandages, compresses and shoulder braces supports can be used to immobilise the shoulder joint, which will help to reduce inflammation of the bursa as it will not be under constant pressure. This technique will improve joint range of motion, so the patient will be able to return to normal movement within a few weeks. As with the other treatments, this therapy must be supervised by a doctor to avoid injury.
- Thermotherapy: for shoulder bursitis, superficial heat is applied to the affected area for about 20 minutes per session. This decreases chronic inflammation of the muscles due to the activation of the tissues through dilation of the blood vessels. Different methods can be used, ranging from electric blankets, hot water bottles and special creams.
- Natural remedies using plants: through the use of infusions, or through aromatherapy, it is possible to reduce muscle stiffness caused by the patient's stress. The aim of this treatment is for the patient to find a mental balance that allows relaxation in order to decompress the bursa of the shoulder and thus obtain as a result that the joint works with the correct opening. Linden, camomile, mint and citrus fruits are plants widely used in this treatment.
- Healthy lifestyle habits: re-education of the patient is essential not only to avoid new injuries, but also to rest the joint periodically, correct gross movements with the shoulder and adopt different postures whenever the joint body needs to be strained. This should be accompanied by exercise and a healthy diet.
Nutritional supplements
In frequent cases of subacromial bursitis, the treating physician refers the patient to a nutritionist to prescribe supplements to help improve the symptoms of subacromial bursitis. In this way, the person can ingest dosed amounts of hyaluronic acid, minerals, glucosamine and vitamins in the form of powders, tablets or syrups
It should be noted that self-medication can cause severe damage to the liver and gastrointestinal tract. These supplements should never be purchased without medical supervision.
Physiotherapy treatments
Through repetitive and short repetitive exercises, it is possible to improve the opening of the shoulder joint. This will help to decompress the subacromial bursa and thus reduce inflammation and pain.
Different techniques are used in physiotherapy, which will be at the discretion of the practitioner. Among the most common is the use of laser muscle stimulation, which causes a deep heat in the tissues, improving the dilation of the blood vessels. In addition to this it is possible to use ultrasound and electrotherapy.
Medications
As with food supplements, drug therapy must be supervised by a doctor. This means that self-medication can lead to internal bleeding and other serious sequelae. In addition, it is possible that the symptoms of bursitis may increase due to incorrect dosage, frequency or type of medication.
Treatment includes opioid analgesics, non-steroidal anti-inflammatory drugs and, in some cases, antibiotics.
Surgery and fluid removal
Bursectomy is the most commonly used surgical operation in these cases of subacromial bursitis, because it is possible to remove the synovial bursa from the shoulder. This can lead to serious complications if not properly rested.
In less serious cases, the removal of the synovial fluid by means of injectable systems is used. This involves inserting a needle and drawing the excess fluid from the bursa into the syringe. It goes without saying that both cases are applied only when the progression of the disease requires it.
Which methods of prevention for shoulder bursitis are the most effective?
It is possible to avoid shoulder bursitis by taking into account different preventive methods, which are mentioned below
- Avoid picking up heavy objects: excessive force or lifting heavy objects with the shoulder can cause serious injury to the muscles adjacent to the subacromial bursa. This will put pressure on the bursa and cause it to become irritated.
- Always maintain correct posture: Daily activities can cause the shoulder bursa to be affected if you make sudden movements or use excessive force. For this reason, it is important to know how to perform different tasks without straining your shoulder muscles and tendons.
- Choose a healthy diet: don't forget that fatty foods cause uric acid not to be excreted from the body, leading to microcrystals in the joint. This leads to an increased likelihood of bone spurs.
- Protect your shoulder: if you have to do work or physical activity that exposes the shoulder structure, it is advisable to use shoulder protectors that help keep the joint immobile. In this way, the bursa will not suffer pressure, thus avoiding inflammation.
- Be physically active: a sedentary lifestyle is a major risk factor that can lead to inflammation of the subacromial bursa. Therefore, keeping the joint moving will help to stretch the shoulder muscles.
- Warm up the shoulder area before working or playing sports: don't forget that you will need to warm up beforehand to activate the muscular system and adapt the brain to the new activity you are about to do. In addition to this, it is necessary to stretch the muscles before and after exercise.
- See a doctor at the first sign of bursitis in the shoulder: see a doctor as soon as possible. This will help to avoid a large accumulation of synovial fluid in the bursa, as the professional will diagnose and prescribe medication correctly.
References
- Arias, L. M., Fadrique, R. S., Gil, M. S., & Salgueiro-Vazquez, M. E. (2017). Risk of bursitis and other injuries and dysfunctions of the shoulder following vaccinations. Vaccine, 35(37), 4870-4876. https://www.sciencedirect.com/science/article/pii/S0264410X17309635
- Umer, M., Qadir, I., & Azam, M. (2012). Subacromial impingement syndrome. Orthopedic reviews, 4(2). https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3395987/
- Blaine, T. A., Kim, Y. S., Voloshin, I., Chen, D., Murakami, K., Chang, S. S., ... & Bigliani, L. U. (2005). The molecular pathophysiology of subacromial bursitis in rotator cuff disease. Journal of Shoulder and Elbow Surgery, 14(1), S84-S89. https://www.sciencedirect.com/science/article/abs/pii/S1058274604002812
- Huston, K. A., Nelson, A. M., & Hunder, G. G. (1978). Shoulder swelling in rheumatoid arthritis secondary to subacromial bursitis. Arthritis & Rheumatism: Official Journal of the American College of Rheumatology, 21(1), 145-147. https://onlinelibrary.wiley.com/doi/abs/10.1002/art.1780210123
- Santavirta, S., Konttinen, Y. T., Antti-Poika, I., & Nordström, D. (1992). Inflammation of the subacromial bursa in chronic shoulder pain. Archives of orthopaedic and trauma surgery, 111, 336-340. https://link.springer.com/article/10.1007/BF00420062
- McAfee, J. H., & Smith, D. L. (1988). Olecranon and prepatellar bursitis. Diagnosis and treatment. Western Journal of Medicine, 149(5), 607. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1026560/
- Reilly, D., & Kamineni, S. (2016). Olecranon bursitis. Journal of shoulder and elbow surgery, 25(1), 158-167. https://www.sciencedirect.com/science/article/abs/pii/S1058274615004693
- Khodaee, M. (2017). Common superficial bursitis. American family physician, 95(4), 224-231. https://www.aafp.org/pubs/afp/issues/2017/0215/p224.html
- Rasmussen, K. J. E., & Fanø, N. (1985). Trochanteric bursitis: treatment by corticosteroid injection. Scandinavian journal of rheumatology, 14(4), 417-420. https://www.tandfonline.com/doi/abs/10.3109/03009748509102047
- Sayegh, E. T., & Strauch, R. J. (2014). Treatment of olecranon bursitis: a systematic review. Archives of orthopaedic and trauma surgery, 134, 1517-1536. https://link.springer.com/article/10.1007/s00402-014-2088-3