Understanding the difference between what is an ailment and what is an illness, which are sometimes not linked, is essential to know what treatment to use to cure you as soon as possible. Often an unfortunate blow causes an ailment, but this does not mean that you are ill.
In this article you will learn the difference between the concepts of illness and disease, as well as the most common types of injuries and ailments that exist when performing a daily physical activity or sporting discipline.
Definition: What is an illness, conditions or disease?
If we stick to clinical terms, both concepts are different in their origin. Diseases are alterations in body functioning that will cause symptoms describing the intensity of the disease at that moment.
When we talk about "alterations in bodily functioning" it is because we use clinical tools that allow us to have a clear diagnosis of what is the difficulty that afflicts the patient, then we proceed to address the problem with the use of complementary therapies, recovery techniques, products to improve health and if there is no other choice, with the use of drugs.
Throughout this process, the person manifests feelings in a specific way, signs that are more related to the ailments because these symptoms are subjective and will help the medical specialist to have more clarity about the alterations that affect the patient.
An ailment could be defined as a symptom of a disease, as it focuses on a specific sensation that could be indicative of a much worse and complete condition. For example, joint pain is an ailment, which could indicate that the patient may be suffering from osteoarthritis or has ligament damage if this pain follows a sprain.
What is the difference between illness and disease?
As we mentioned, having an ailment is not the same as having a disease. It is necessary to differentiate each concept in detail, as this will be key when making a correct clinical diagnosis.
For example, if during boxing practice a fracture occurs in the fingers of the hand; is it an ailment, an injury or a disease?
Let's see what it is:
- If the fracture is not associated with a previous disease, such as arthritis, it is a sports injury with an ailment.
- It is adisease if there is already a history of arthritis in the athlete and this fracture is a further consequence of that degenerative process.
In order to have an accurate answer, it is not enough to observe the health specialist and to carry out physical examinations. It is also important to have the affected person's perception and to know their medical history, as well as their sporting history if they practice a particular discipline. In this way, their symptoms (associated with the ailment) and clinical indicators (associated with the disease) are related.
Two branches of medicine are curative care and preventive medicine:
In curative medicine the patient arrives with an ailment, which is summarised in the characteristics that the patient perceives and which will give clues to the doctor as to what is going on in his body. This is a perception of the patient, a subjectivity, which is often not linked to the actual cause of the disease, but this perception should not be dismissed, as one person can have several complaints associated with several diseases.
In sports medicine, the specialist studies the effects of sport and physical activity in general on the human organism from the point of view of prevention and treatment of injuries caused by physical activity.
As a patient, you must have a good command of the concepts of ailment and illness, so that you can give the specialist doctor the right advice to help you recover your health and your sporting activity.
Best conditions products
Bestseller
What are the most common types of ailments or conditions?
In the medical field, there is a formal classification of illnesses and health problems: epidemic, constitutional or general illnesses, localised and ordered by body area, developmental disorders and trauma.
Arthritis
Arthrosis and rheumatoid arthritis are the two most common types of arthritis that can affect anyone. It is a pathology caused by wear and tear of the cartilage in the joints. It is a degenerative disease and its progression is gradual and progressive.
Its appearance is closely related to genetic factors, although it also has to do with the patient's lifestyle, with sportsmen and women being very affected who for many years of their lives have intensely practised a sport that makes excessive demands on their joints. On the other hand, a sedentary lifestyle can also be a risk factor.
Bursitis
In every joint there are bursae, small sacs with fluid inside them that serve as shock absorbers for shocks and friction between the bones. Bursitis is the inflammation of synovial bursae, and can commonly occur in the shoulder, elbow, hip, knee and ankle.
As mentioned above, bursae are small fluid-filled sacs that become inflamed when muscles, tendons and ligaments put pressure on them. For example, in football, bursitis is most common in the knees and ankle. In boxing, bursitis usually occurs in the shoulder. One treatment option is to drain excess fluid from the bursa to relieve the pain, but as a preventive measure , rest is recommended to reduce the inflammation.
Cramps
These are small muscle contractures caused by both excessive tension of the muscle fibres and nerve compression. Whenever there is a cramp there should be rest. They are most common in the thighs, arms, abdomen and rib cage.
Many of these cramps are also caused by an electrolyte imbalance in our body, often due to extreme dehydration, it is enough to replenish the fluids lost during physical activities in high temperature or long duration conditions. Deficiency of micronutrients such as certain minerals, such as magnesium or potassium, lack of B vitamins such as B1 and B3 are also the cause of cramps.
Sciatica
The sciatic nerve (or sciatica) is the largest nerve in the human body and is made up of several nerve endings coming from the spinal column. Sciatic pain starts at the end of the spine, runs down the buttocks, through the back of the thigh and into the knee, even up to the ankle.
It starts with irregular pain in the legs and arms. It is more common in people who practice sports such as weightlifting and golf where there is a high physical demand on the back and it is normal for there to be pain due to the displacement of discs which causes the pinching of the sciatic nerve. It is also very common in people who spend many hours sitting at work or in postures where the sciatic nerve suffers pressure.
Muscle strains
This is a mild injury if it is treated in time and the necessary rest is taken to allow the muscle to regenerate completely. It is a contracture of the muscle fibres that occurs due to overworking the muscle fibres. A muscle contracture originates during physical work, after an intense sporting effort or as a residual form associated with a more serious injury. It is a fairly common ailment among sportsmen and women.
They can also arise suddenly while performing an intense physical activity for which our muscle fibres are not prepared or are previously overloaded due to fatigue, excessive training or poor execution technique. When we sprint at high speed or lift a heavy weight, our muscles can suffer a muscle strain due to various factors, such as overload, weakness, stress, micronutrient deficiency, poor hydration, etc.
Sprains
Sprains are very common injuries in the sporting world caused by overstretching of the ligaments in the joints. A sprain has three possible degrees of severity, in the third degree there is a complete rupture of the ligament and will require surgery by arthroscopy.
Common symptoms when a sprain occurs are severe localised pain, swelling of the entire joint, deformity in the area, change in skin colour and difficulty in moving freely. If a sprain is a first degree sprain, recovery is quicker because the ligament is not torn and regenerates better, although a poorly healed sprain can become chronic or reproduce more easily.
Plantar fasciitis
Fascia is a tissue on the sole of the foot that runs from the heel to the metatarsals. It is responsible for maintaining the plantar arch and connecting the heel to the toes. When injured, this fascia becomes inflamed and causes a sharp pain when walking.
It has the characteristic of causing pain in the morning after waking up or when resting after physical activity. It is more common in athletes, but anyone else can suffer from it without playing sport.
Bone fractures
A fracture is a partial or total breakage of a bone caused by trauma, or by weakening of the bones due to wear and tear of the cartilage. This can occur as a result of an occasional fall during physical activity, or in people with fragile bone structure such as osteoporosis or arthritis patients.
The most extreme cases are open fractures, where pieces of bone affect soft tissues such as muscles, tendons and ligaments. In this type of fracture, surgery is necessary to fuse the pieces of bone together and repair the damaged tissues.
Tendonitis
Tendonitis is another of the most common ailments in sports or jobs that require repetitive movements. It occurs when a tendon becomes irritated and inflamed from the overload of strain in training and daily activities. Poor technique and under-warming the body will cause tendons to suffer more. However, another common cause is the loss of tendon elasticity that occurs over the years.
Tendons can suffer partial micro ruptures or total ruptures, so in the event of discomfort, it is important to take proper rest to allow our tendons to fully recover. A recurrence of injury to the same tissue will make full recovery more complex and can lead to chronic tendonitis.
Herniated disc
One of the most common ailments in elderly people or athletes who perform strength sports such as weightlifting. It occurs when a vertebra is out of position or when the disc of the vertebra fractures and lets part of its nucleus come out, pressing on a nerve that in turn will generate severe pain.
When it is detected in its early stages, it can be solved with the application of physiotherapy exercises, or other therapies such as cryotherapy and the use of compression garments.
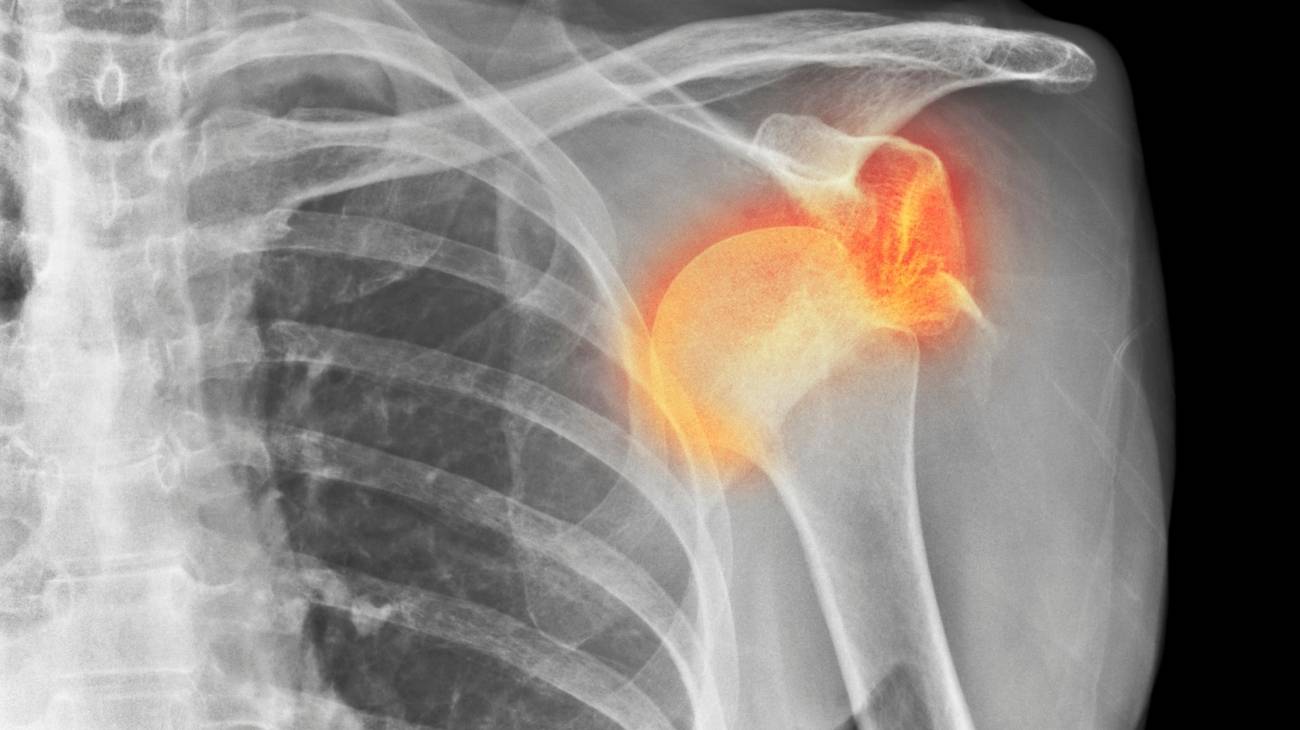
Dislocations
This is the term used to describe when a bone slips out of position in a joint, causing pressure and damage to the ligaments and muscles in the joint, limiting the mobility and function of the limb involved. It usually occurs when a joint is hit by a strong blow that, although it does not cause fractures, does cause the bone to move.
The most common dislocations usually occur in the shoulder, when the head of the humerus protrudes from the glenoid cavity of the scapula; in the knee by a movement that removes the femur from its position; or at the elbow, if the radius or ulna loses its natural position. Although basically any bone that participates in a joint can dislocate.
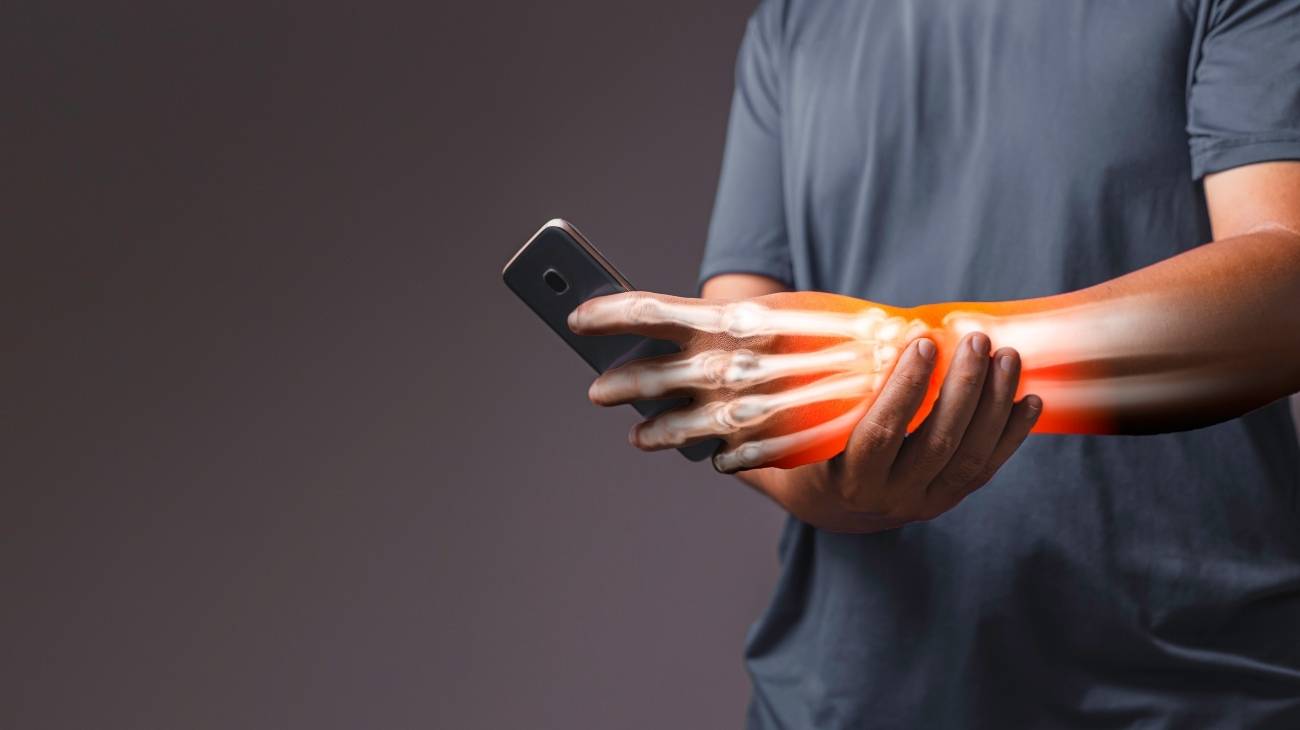
Carpal tunnel syndrome
This ailment occurs due to compression or tension in the tunnel through which the transverse carpal ligament passes, which in turn directly affects the radial nerve that crosses the same area, thus generating a discomfort that in its early stages begins as a simple tingling, but over the years it evolves into severe pain in the wrist and thumb.
References
- Zwar, N., Harris, M., Griffiths, R., Roland, M., Dennis, S., Powell Davies, G., & Hasan, I. (2006). A systematic review of chronic disease management. https://openresearch-repository.anu.edu.au/bitstream/1885/119226/3/final_25_zwar_pdf_85791.pdf
- Hunter, D. J., & Fairfield, G. (1997). Managed care: disease management. Bmj, 315(7099), 50-53. https://www.bmj.com/content/315/7099/50.short
- Ellrodt, G., Cook, D. J., Lee, J., Cho, M., Hunt, D., & Weingarten, S. (1997). Evidence-based disease management. Jama, 278(20), 1687-1692. https://jamanetwork.com/journals/jama/article-abstract/419018
- Bodenheimer, T. (1999). Disease management—promises and pitfalls. New England Journal of Medicine, 340(15), 1202-1205. https://www.nejm.org/doi/pdf/10.1056/NEJM199904153401511
- Mueser, K. T., Corrigan, P. W., Hilton, D. W., Tanzman, B., Schaub, A., Gingerich, S., ... & Herz, M. I. (2002). Illness management and recovery: A review of the research. Psychiatric services, 53(10), 1272-1284. https://ps.psychiatryonline.org/doi/full/10.1176/appi.ps.53.10.1272
- Rothman, A. A., & Wagner, E. H. (2003). Chronic illness management: what is the role of primary care?. Annals of Internal Medicine, 138(3), 256-261. https://www.acpjournals.org/doi/abs/10.7326/0003-4819-138-3-200302040-00034
- Wagner, E. H. (1998). Chronic disease management: what will it take to improve care for chronic illness?. Effective clinical practice, 1(1). https://access.portico.org/Portico/auView?auId=ark:%2F27927%2Fphwwtrq3nv
- Hawker, G. A., Mian, S., Kendzerska, T., & French, M. (2011). Measures of adult pain: Visual analog scale for pain (vas pain), numeric rating scale for pain (nrs pain), mcgill pain questionnaire (mpq), short‐form mcgill pain questionnaire (sf‐mpq), chronic pain grade scale (cpgs), short form‐36 bodily pain scale (sf‐36 bps), and measure of intermittent and constant osteoarthritis pain (icoap). Arthritis care & research, 63(S11), S240-S252. https://pubmed.ncbi.nlm.nih.gov/22588748/
- Johnson, C. (2005). Measuring pain. Visual analog scale versus numeric pain scale: what is the difference?. Journal of chiropractic medicine, 4(1), 43. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2647033/
- Ledón Llanes, L. (2011). Enfermedades crónicas y vida cotidiana. Revista cubana de salud pública, 37, 488-499. https://www.scielosp.org/article/ssm/content/raw/?resource_ssm_path=/media/assets/rcsp/v37n4/spu13411.pdf