- What is dislocation of the knee joint?
- What are the causes and risk factors for knee dislocation?
- Best products for knee dislocation
- Main signs and symptoms that warn us that we have a knee dislocation
- What is the first aid for a dislocated knee?
- What are the most effective prevention methods for dislocated knee joints?
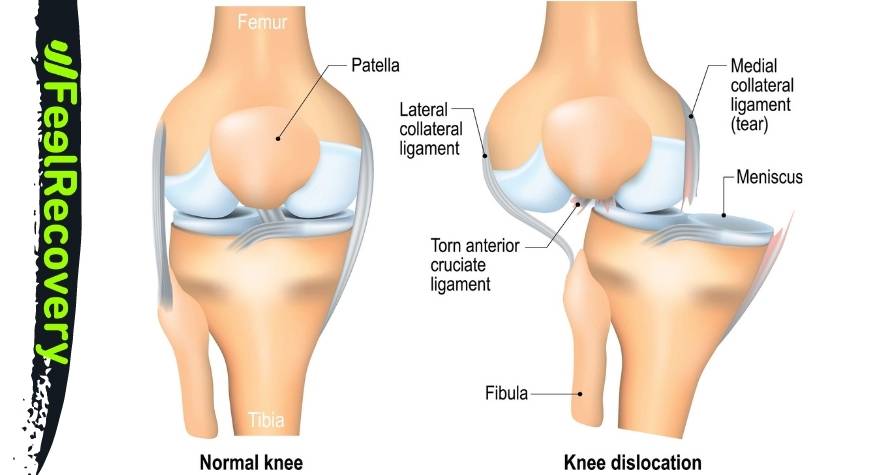
The slippage that occurs between the end condyles of the femur and the head of the tibia causes the glenoid sockets to fail to fully or partially join. This is a major trauma that occurs frequently in athletes, so you need to read about what a dislocated knee is.
To find out if you have this type of trauma, we will show you the main symptoms and the most common causes of this ailment. On the other hand, you will be able to read about the steps you should take to help a person with a dislocated knee. Let's get started.
What is dislocation of the knee joint?
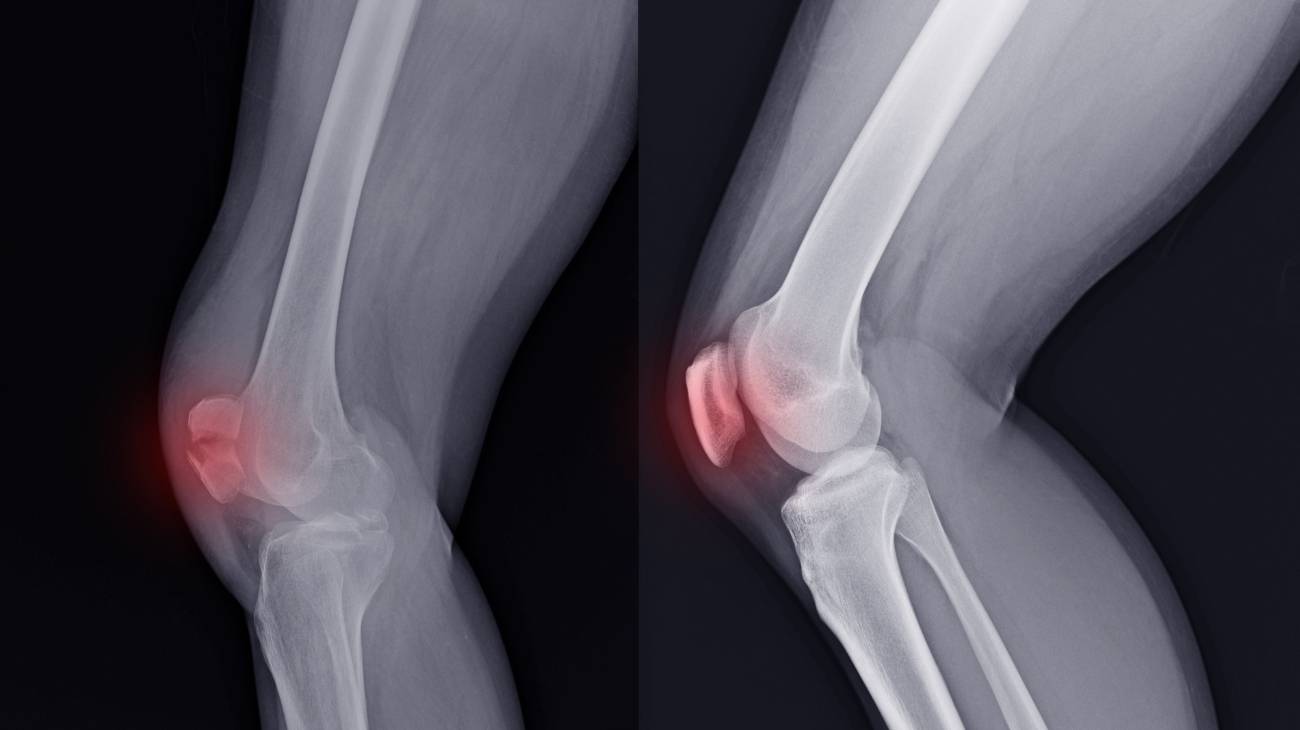
Dislocation of the knee joint is the separation of the lower part of the femur, the condyles, from the upper part of the tibia, the glenoid sockets. This separation of the bones can be complete or partial, the latter being called knee subluxation.
For the joint to be reduced or aligned, it is necessary to treat the trauma patient with medical protocols, which can last up to 8 weeks of treatment. But in more severe cases, remission of the trauma usually comes after 6 months of treatment.
What are the causes and risk factors for knee dislocation?
Among the causes that increase the occurrence of a knee dislocation are the following:
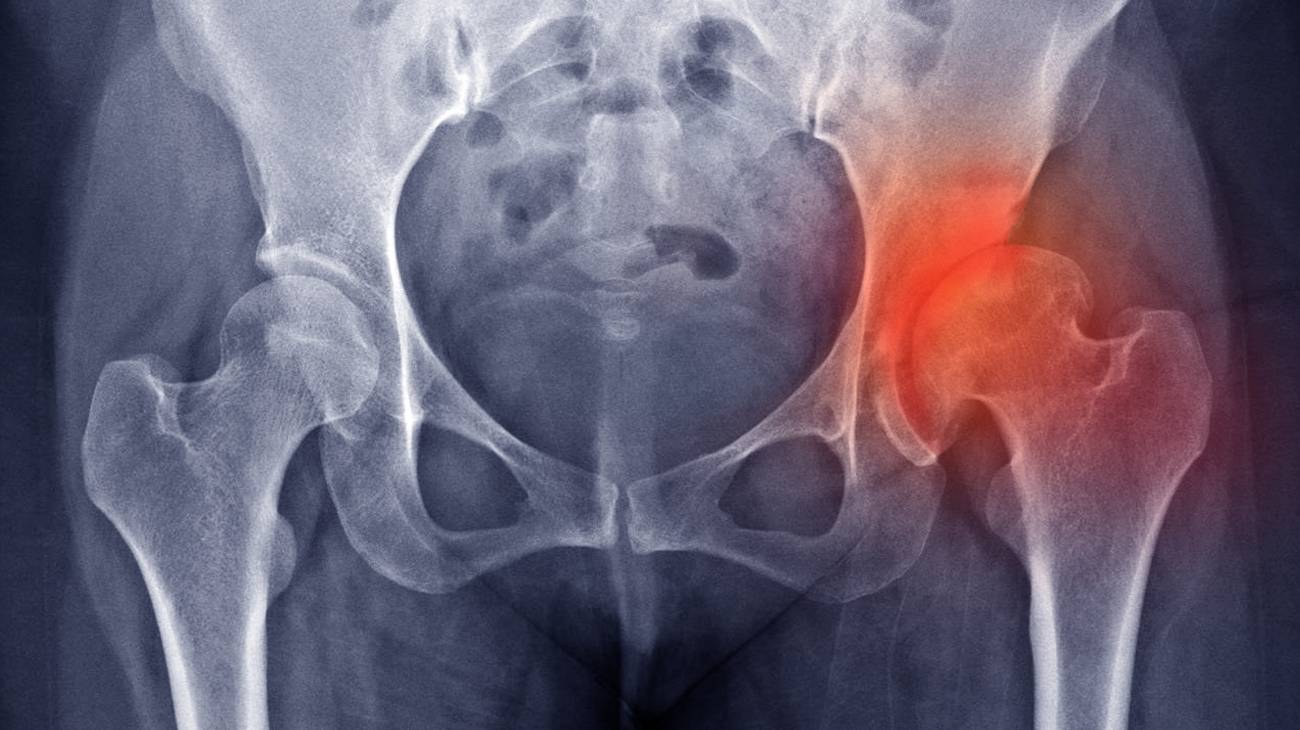
- Body overweight: Maintaining excessive weight leads to a reduction in knee cartilage space, which wears down over time. This will result in unrestricted movement in the joint area, leading to separation of the femur and tibia.
- Engaging in demanding activities: Playing sports such as football, basketball and tennis causes the knee to be constantly stressed, leading to overload that can lead to dislocation.
- Weak connective tissues: Ligaments can lose strength if they are not stimulated by exercise, although overloading can have the same effect. If these tissues are weak they will not be able to support the attachment of the femoral condyles to the glenoid sockets.
- Age of the patient: Another reason why a muscle or tendon tissue loses strength is because of weakening as the person's age advances. This can create a knee dislocation more often than in a younger patient.
- Knee osteoarthritis: The corrosion to the cartilage, and in some cases the bones, caused by this chronic, degenerative disease causes the cartilage to shift with any movement.
- Previous injuries: If a person has suffered previous dislocations, they are more likely than other patients to suffer this type of injury on more occasions.
- Previous surgical interventions: As with injuries, knee surgeries caused by meniscus tears, fractures and other ailments are also risk factors that increase the possibility of suffering a dislocation.
- Diabetes: This type of disease causes the blood not to exchange nutrients with the muscle and connective tissues in a normal way, which weakens them. This can lead to knee dislocations.
Best products for knee dislocation
Bestseller
-
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Hearts)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Oxford)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Sport)
£24,95 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Hearts)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Oxford)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Sport)
£20,95
Main signs and symptoms that warn us that we have a knee dislocation
It is feasible to know you have a dislocated knee if the following signs and symptoms are present:
- Greater than normal rotation and adduction movements: This occurs due to the lack of superficial connection between the femur and the glenoid cavities of the tibia, which causes the normal biomechanical limit.
- Inflammation: The accumulation of blood causes the knee to swell causing discomfort and in some cases fever.
- Lumpy appearance: When there is a complete dislocation of the knee, it is possible to see the end of the femur or the head of the tibia as a large nodule under the skin.
- Deformity: Subluxation causes disproportion in the knee due to partial displacement of the bones.
- Intense pain: The central nervous system emits symptoms of pain in the affected area due to pressure on the nerve roots in this part of the body.
- Inability to walk: A dislocated knee causes an inability to move the joint, to support the foot and also to sit down.
- Bruising: The large amount of blood that concentrates in the knee causes bruising of the joint.
- Paraesthesia: Numbness of the upper leg, calf and foot is common in these traumas.
What is the first aid for a dislocated knee?
A person with a dislocated knee can be helped by means of a physiotherapeutic protocol that describes in an orderly manner the steps to be performed on a trauma patient. It is important to note that this method can only be used for minor injuries, otherwise the injury can be aggravated.
Take a look at the step-by-step procedure to be performed to help a person with a dislocated knee:
- Protection: The first thing you will need to do is protect the affected area. To do this, you will need to remove the patient from the site of the accident or clear the area where the person is, if they are unable to walk.
- Rest: Next, you will have to make the patient rest. This consists of stopping the person from doing the task that caused the trauma and keeping them in constant rest until you continue with the following steps.
- Ice: Apply cold to the knee as the dislocation generates pain and inflammation immediately, so placing a cold object will help to reduce these symptoms. This should not exceed 15-20 minutes as this may cause skin burns. Different products can be used, but the most recommended for this case are cold gel packs that help to maintain the ideal temperature.
- Compression: Wear compression garments, what you should do now is apply compression products to help keep the joint as firm as possible and improve blood flow. For this you can choose a sports compression knee brace.
- Elevation: For this protocol to generate the expected results it is advisable to raise the knee above the heart line to avoid blood clots and accumulation of blood, reducing blood pressure in the injured area.
Once we have stabilised the patient, they should ideally be taken to the nearest hospital so that the doctor can treat the dislocation between the tibia and femur correctly.
What are the most effective prevention methods for dislocated knee joints?
It is possible to prevent knee dislocation if the following criteria are taken into account:
- Try to exercise daily: This will help improve circulation and keep the knee in working order, which will improve lubrication of the knee joint.
- Control body weight: Sedentary lifestyles can lead to obesity, which is a major risk factor for knee dislocation. This is due to excessive weight bearing on the knee for those who are overweight.
- Protect the joint: To keep the glenoid cavity of the tibia in contact with the femoral condyles, it is advisable to wear compression garments that help improve the performance and stability of the knee. For this purpose, compression sports knee braces can be used.
- Apply cold to the area: Once you have finished practising sports or any activity that is demanding for the knee, it is recommended to apply cold to rest this part of the body and speed up recovery. This can be done by means of cold gel packs for 20 minutes each application.
- Relax the muscles: The muscle structure can be relaxed by massage. This will help to strengthen the joint and prevent slippage of the tibia with the condyles of the femur. Different techniques can be applied, but the most commonly used are massage rollers and electric back and leg massagers.
- Take vitamin D and calcium: This will help to keep the tissues in good condition, which will prevent knee dislocation. Also, for a better assimilation of vitamin D, sunbathe at least 30 minutes a day.
- Avoid falls: Knocks to the knee are a common cause of joint dislocation. For this reason, it is advisable to avoid all risky situations and make common sense decisions to avoid falling.
- Mobilise the knee: Warming up the muscles, joints and ligaments beforehand helps to prevent a dislocated knee, but it is also advisable to stretch these tissues once the sport is over.
- Keep a responsible training plan: Don't try to move quickly by pushing your knee to meet short-term goals, as this will increase the likelihood of dislocation. Progressive training will help reduce the risk of injury.
References
- Wascher, D. C., Dvirnak, P. C., & DeCoster, T. A. (1997). Knee dislocation: initial assessment and implications for treatment. Journal of orthopaedic trauma, 11(7), 525-529. https://journals.lww.com/jorthotrauma/Abstract/1997/10000/Knee_Dislocation__Initial_Assessment_and.11.aspx
- Howells, N. R., Brunton, L. R., Robinson, J., Porteus, A. J., Eldridge, J. D., & Murray, J. R. (2011). Acute knee dislocation: an evidence based approach to the management of the multiligament injured knee. Injury, 42(11), 1198-1204. https://www.sciencedirect.com/science/article/abs/pii/S0020138310007552
- Yeh, W. L., Tu, Y. K., Su, J. Y., & Hsu, R. W. W. (1999). Knee dislocation: treatment of high-velocity knee dislocation. Journal of Trauma and Acute Care Surgery, 46(4), 693-701. https://journals.lww.com/jtrauma/Abstract/1999/04000/Knee_Dislocation__Treatment_of_High_Velocity_Knee.23.aspx
- Seroyer, S. T., Musahl, V., & Harner, C. D. (2008). Management of the acute knee dislocation: the Pittsburgh experience. Injury, 39(7), 710-718. https://www.sciencedirect.com/science/article/abs/pii/S0020138307004858
- SISTO, D. J., & WARREN, R. F. (1985). Complete knee dislocation: a follow-up study of operative treatment. Clinical Orthopaedics and Related Research®, 198, 94-101. https://journals.lww.com/clinorthop/Abstract/1985/09000/Complete_Knee_Dislocation__A_Follow_up_Study_of.14.aspx
- Shelbourne, K. D., Porter, D. A., Clingman, J. A., McCarroll, J. R., & Rettig, A. (1991). Low-velocity knee dislocation. Orthopaedic review, 20(11), 995-1004. https://europepmc.org/article/med/1749665
- Stayner, L. R., & Coen, M. J. (2000). Historic perspectives of treatment algorithms in knee dislocation. Clinics in sports medicine, 19(3), 399-413. https://www.sciencedirect.com/science/article/abs/pii/S0278591905702143
- Arendt, E. A., Fithian, D. C., & Cohen, E. (2002). Current concepts of lateral patella dislocation. Clinics in sports medicine, 21(3), 499-519. https://www.sportsmed.theclinics.com/article/S0278-5919(02)00031-5/fulltext
- Hawkins, R. J., Bell, R. H., & Anisette, G. (1986). Acute patellar dislocations. The American journal of sports medicine, 14(2), 117-120. https://journals.sagepub.com/doi/abs/10.1177/036354658601400204
- Garth JR, W. P., Pomphrey JR, M., & Merrill, K. (1996). Functional treatment of patellar dislocation in an athletic population. The American Journal of Sports Medicine, 24(6), 785-791. https://journals.sagepub.com/doi/abs/10.1177/036354659602400614