- What is patellar tendinopathy of the knee?
- What are the causes and risk factors for patellar tendonitis?
- Best products for patellar tendonitis
- Main symptoms that warn us that we have knee tendonitis
- What treatments are there to improve and cure patellar tendonitis?
- Prevention for knee tendon inflammation
Take a look at the following paragraphs if you want to know what patellar tendonitis of the knee is and what are the risk factors that cause this injury to the tendon fibres. To do so, you will have to read carefully all the information that we will show you in a simple way about the symptoms that will warn you of the presence of a micro rupture in the patellar tendons.
But this is not all you will find, we will also mention the different therapies and treatments that are currently used to reduce the symptoms of knee tendinopathy. We invite you to continue reading this article to the end.
What is patellar tendinopathy of the knee?
Inflammation that occurs in the patellar tendon located in the knee to join the kneecap and tibia is known as patellar tendinopathy of the knee. This injury causes the tendon tissue fibres to rupture, which can be extremely small or, in severe cases, a few millimetres.
Tendinitis is caused by overuse of the knee and a lack of blood supply to the affected area. This leads to the accumulation of microparticles with toxic substances that cause pain and the inability to move the joint properly.
What are the causes and risk factors for patellar tendonitis?
We will show you in the following points what are the most common causes that can lead to the appearance of patellar tendonitis of the knee
- Demanding sports practices: It is common to find athletes with this type of ailment due to the demands placed on the joint when running or jumping. This is also related to those jobs in which this type of action is required to perform the task. On the other hand, lack of warming up beforehand can also lead to patellar tendinopathy.
- Overweight of the patient: Maintaining excessive body weight can lead to micro-tears in the tendon fibres, which will cause inflammation in the patellar tendons. In addition, unprotected lifting of heavy objects also puts excessive pressure on the joint, leading to future tendonitis.
- Previous trauma: Both blows and fractures can lead to the development of patellar tendonitis. This is due to the exposure the tendons have within the joint structure, which can affect or tear the tendon fibres.
- Lack of exercise: A sedentary lifestyle is a factor in this type of tendon injury. This is due to the fact that muscles and tendons are not used to maintaining activity, so that, at the slightest demand, they suffer and cause an excess of lactic acid, which cannot be completely eliminated by the blood.
- Rheumatoid diseases: Arthritis and osteoporosis can cause tendonitis due to corrosion of the bones that form the knee. This results in defective joint amplitude, which leads to tendonitis.
- Advanced age: People over 50 years of age lose elasticity and collagen in the muscles, which makes tendonitis more likely to appear.
- Inadequate diet: Lack of potassium and selenium, among others, leads to the tendon fibre structure not working properly. This will lead to the appearance of patellar tendonitis caused by the appearance of debris in the fibres of the tendon tissues.
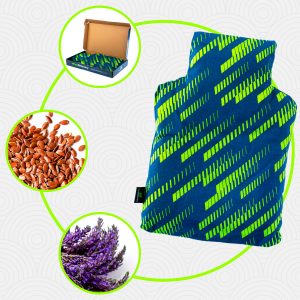
Best products for patellar tendonitis
Bestseller
-
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Hearts)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Oxford)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Sport)
£24,95 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Hearts)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Oxford)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Sport)
£20,95
Main symptoms that warn us that we have knee tendonitis
As with all illnesses, the body warns of an abnormality in the organism, so tendonitis also has characteristic signs.
See below all the symptoms that will warn you of the presence of knee tendonitis:
- Creaking noises in the affected area: The inflammation causes the joint body space to not work properly, so that when the patient moves the knee, he/she makes clicking noises.
- Swelling in the joint: This is one of the most characteristic symptoms of patellar tendonitis and is generated by the accumulation of toxic substances that are deposited in the tendon fibres. This arises because of the inability of the blood flow to eliminate them.
- Penetrating pain in the area around the patellar tendon: A sharp pain occurs when bending the knee, standing, walking or touching the affected area. This symptom is caused by the large number of nerve roots that are being pressed by the inflammation.
- Loss of joint movement: Inability to bend the knee or walk is a characteristic symptom of this tendon injury. Numbness is generated in the muscles and tendons due to lack of blood supply to the affected area.
- Tingling sensation: Paresthesia and loss of sensation are frequent signs of this type of tendonitis caused by overexposure of the nerves in this area.
- Muscle weakness: Patients may have trouble walking or getting up from a chair. This is due to a lack of blood supply to the tendons, which are responsible for moving the muscle structure.
What treatments are there to improve and cure patellar tendonitis?
The symptoms of patellar tendonitis can be controlled and even made to disappear through the implementation of different treatments and therapies.
Find out which are the most important ones:
Alternative and complementary therapies
Among the different complementary and alternative treatments that are applied to improve and heal patellar tendonitis are the following:
- Hot and cold therapy: The properties of cold help to reduce inflammation and pain by stimulating the release of endorphins, which act as a natural painkiller. While heat contributes to the dilation of the capillary walls found in the tendon fibres, causing better blood circulation. In this way, metabolic waste products in the tendons are eliminated, improving the feeling of well-being and increasing the likelihood of the disease going into remission.
- Compression therapy: Patellar tendinitis of the knee can be treated with knee braces, elastic compression bandages or patellar tapes. This helps to keep the joint in a correct position, which will stimulate the dilation of the capillaries and allow the blood to circulate better. In this way it is possible to reduce swelling and pain. In addition, with this treatment the tendons lose the constant pressure they are under due to the injury and can recover in a shorter time.
- Massage therapy: The symptoms caused by tendinitis in the knee can be reduced by means of massage therapy. This consists of rubbing and rubbing the affected area to stimulate the venules and arterioles in this part of the body. In this way, a better blood circulation is obtained, generating a better exchange of nutrients and oxygen between the blood and the affected fibres.
- Acupressure therapy: This type of oriental medical treatment aims to stimulate the central nervous system and blood circulation. This is done by strategically massaging different points of the body using only the fingers and palms of the hands. The physiotherapist applies controlled pressure to the different areas to provoke emotional balance and a feeling of general well-being in the patient.
- Thermotherapy: Symptoms arising from inflammation of the patellar tendons can be improved and treated by applying heat to the affected area. This stimulates the blood supply and optimises the exchange of oxygen and nutrients between the blood and the tendon tissues. The dilation of the capillaries reduces pain and improves joint movements.
- Natural remedies using plants: There are different medicinal plants that provide benefits for the symptoms of patellar tendonitis. This is because the components of these herbs contain analgesics and anti-inflammatories, although it is also possible to find soothing plants. For this reason, a patient who undergoes this type of therapy will see a reduction in pain and inflammation. It is advisable to consult a doctor before ingesting or applying warm baths with these herbs.
- Healthy lifestyle habits: Eating healthy, avoiding excess weight and perfecting posture are some of the objectives of this re-education therapy to improve and combat patellar tendon tendinitis. The treatment focuses on itinerant consultations with the doctor, which helps to cope with everyday tasks and sports in a better way.
Nutritional supplements
The aim of this therapy is to include micronutrients in the patient's diet that may be lacking in the body. In this way it is possible to ingest powders, liquids, tablets or pills in which mineral salts and vitamins predominate; it must not be forgotten that all these elements are necessary for the correct functioning of the tendons of the knee. Before implementing this therapy , it is advisable to consult a doctor to avoid possible intoxication.
Physiotherapy treatments
Physiotherapy consists of the gradual rehabilitation of the patient carried out by means of muscle strengthening exercises and mobility of the knee. This is achieved by the application of internal heat to the affected area, which does not generate pain and side effects in the patient. Different techniques can be applied according to the degree of progression of the injury and the physiotherapist's criteria. Among the most commonly used are laser therapy, ultrasound and joint coaptation manoeuvres.
Medications
Opioid analgesics, anti-inflammatory NSAIDs and in some cases corticosteroids are used in this drug therapy. It should be noted that these medications must be prescribed by a physician who has verified and verified the presence of inflammation in the patellar tendons. For this reason, self-medication is not recommended under any circumstances due to the serious consequences that this can have.
Surgeries
In order to restore the mobility of the knee, the doctor may decide to perform surgery due to the progress and severity of the disease, which cannot be treated with conventional methods. For this reason, local or general anaesthesia is used to repair the tendon structure or replace the joint in very advanced cases. It should be emphasised that before resorting to surgery, all non-invasive or preventive treatments and remedies must be exhausted.
Prevention for knee tendon inflammation
Learn about all the methods that will help you prevent knee tendonitis
- Control sedentary lifestyle: Daily exercise will help to keep the patellar tendons in the knee in good condition. This way the tendon tissues will be accustomed to the activities, which will help you avoid tendon injuries.
- Avoid excess body weight: Don't forget that obesity causes excessive stress on the knee, which causes the patellar tendons to work improperly. For this reason, maintaining your ideal weight will help you avoid knee tendonitis.
- Visit your doctor regularly: Clinical and radiological studies will help you detect the existence of tendon fibre ruptures. Therefore, it is advisable to visit the doctor for a series of preventive tests.
- Do not practice dangerous activities: This group includes sports or jobs that place excessive demands on the tendons located in the knee. Although, if for some reason you wish to continue with these tasks, it is advisable to warm up the muscle-tendon structure beforehand and use knee pads or any compressive clothing to protect the joint.
- Include protein-rich foods: Dietary nutrients will help to keep your knee tendons in good condition.
- Always seek to improve proprioception: It is essential to maintain correct posture so that biometric movements do not affect the exposure of the patellar tendons. To do this, it is necessary to know how to stand or sit, walk and even lift objects from the ground.
References
- BENTLEY, G. (1970). Chondromalacia patellae. JBJS, 52(2), 221-232. https://journals.lww.com/jbjsjournal/Abstract/1970/52020/Chondromalacia_Patellae.2.aspx
- Levine, J. (1979). Chondromalacia patellae. The Physician and Sportsmedicine, 7(8), 39-54. https://www.tandfonline.com/doi/abs/10.1080/00913847.1979.11948468
- Warden, S. J., & Brukner, P. (2003). Patellar tendinopathy. Clinics in sports medicine, 22(4), 743-759. https://www.sportsmed.theclinics.com/article/S0278-5919(03)00068-1/fulltext
- Visnes, H., & Bahr, R. (2007). The evolution of eccentric training as treatment for patellar tendinopathy (jumper’s knee): a critical review of exercise programmes. British journal of sports medicine, 41(4), 217-223. https://bjsm.bmj.com/content/41/4/217.short
- Blazina, M. E., Kerlan, R. K., Jobe, F. W., Carter, V. S., & Carlson, G. J. (1973). Jumper's knee. Orthopedic Clinics of North America, 4(3), 665-678. https://www.sciencedirect.com/science/article/abs/pii/S0030589820323439
- Millar, N. L., Silbernagel, K. G., Thorborg, K., Kirwan, P. D., Galatz, L. M., Abrams, G. D., … & Rodeo, S. A. (2021). Tendinopathy. Nature reviews Disease primers, 7(1), 1. https://www.nature.com/articles/s41572-020-00234-1
- Rees, J. D., Maffulli, N., & Cook, J. (2009). Management of tendinopathy. The American journal of sports medicine, 37(9), 1855-1867. https://journals.sagepub.com/doi/abs/10.1177/0363546508324283
- Maffulli, N., Wong, J., & Almekinders, L. C. (2003). Types and epidemiology of tendinopathy. Clinics in sports medicine, 22(4), 675-692. https://www.sportsmed.theclinics.com/article/S0278-5919(03)00004-8/fulltext
- Riley, G. (2008). Tendinopathy—from basic science to treatment. Nature clinical practice Rheumatology, 4(2), 82-89. https://www.nature.com/articles/ncprheum0700
- Xu, Y., & Murrell, G. A. (2008). The basic science of tendinopathy. Clinical orthopaedics and related research, 466, 1528-1538. https://link.springer.com/article/10.1007/s11999-008-0286-4