- What is chondromalacia patella and what grades are there?
- What are the causes and risk factors for chondromalacia patella in the knee?
- Best products for knee tendonitis
- Main symptoms that warn us that we have chondromalacia patellae
- What treatments are available to alleviate pain due to wear and tear of the knee cartilage?
- What prevention methods for chondromalacia patella are the most effective?
Chondromalacia patella is usually cured in most cases. It may take a few days to weeks in milder cases. From this point on, the symptoms should be eradicated and any effort that could lead to a relapse should be avoided. In more severe cases, surgery and cartilage implantation are encouraging for recovery.
For this reason, you should know what chondromalacia of the patella is and why it occurs . You will find this information in the following paragraphs. In addition, you'll read about prevention methods you can use to avoid knee injuries - take a look!
What is chondromalacia patella and what grades are there?
Chondromalacia of the patella is a softening or erosion at the level of the protective cartilage of the joint located in the knee, it is a kind of mild osteoarthritis that attacks the tissue located in the joint body. Since there is a degradation of the tissue, this area withstands less pressure during movement, transmitting it directly to the subchondral bone.
When there is a cartilage lesion, it becomes a chondropathy. Because of this, the patellofemoral joint condition is divided into different degrees of severity up to osteoarthritis.
Let us now look at the different degrees of severity:
- Grade 1: At this point a primary softening of the joint cartilage is observed. On palpation, it tends to be abnormally depressed; however, no cracks are visible, but pain may be milder than in grade 2 or 3, especially when exercising or putting on certain shoes.
- Grade 2: By the time the condition enters stage 2, ulceration or superficial fibrillation is already visible. The lesion does not exceed 1.3 mm in depth, although the pain is more intense given the indentation.
- Grade 3: In grade 3 chondropathy, the ulceration is deeper. In fact, a joint opening of more than 1.3 mm can be seen. In some cases, the pain is more severe and there is evident inflammation due to the localised lesion.
- Grade 4: By this stage the disease is well advanced with a lesion causing an even larger gap. The pain is much more intense than the previous level and there is a risk of ulceration deepening.
- This means that there is a complete opening with loss of cartilage thickness, exposing the subchondral bone. There is usually loss of functional balance, severe and disabling pain. It is known as Eburnation because of the possibility of the bone hypertrophying, just as it would in osteoarthritis.
What are the causes and risk factors for chondromalacia patella in the knee?
There are multiple processes that occur in isolation or together that can lead to the development of a knee injury called chondromalacia patella.
See below what these factors are:
- Age: The ageing process also degenerates cartilage tissues at the cellular level. Due to wear and tear or other diseases linked to old age, older people are much more prone to this condition. In fact, some experts consider it a natural degenerative process.
- Hereditary factors: Sometimes the person has a genetic predisposition defective in some protein responsible for collagen. In other cases, the abnormalities are physical, such as bowleggedness, hip dysplasia (CDD) or joint hyperlaxity (Ehlers-Danlos syndrome), among others. All these factors are potential triggers for chondromalacia.
- Overstimulation: Prolonged repetition of an action on the knee could generate a greater stimulus than it is prepared to receive causing the cartilage to resent, injure or soften. If pain occurs, it is best to stop the movement that triggers it.
- Excessive pressure: Continuous stress on the knee joint can injure the knee tissues. For example, staying in a single position for too long (kneeling, squatting or cross-legged) pushes the pressure it can withstand to the limit, weakening it and increasing the chance of injury.
- Trauma: Blows and bruises directly to the kneecap can also damage the cartilage. This is due to the injury caused to the joint body
- Injuries: If the patient has suffered fractures, lacerations or other injuries to the hip or knee, chondropathy may develop.
- Overweight: Unbalanced body weight leads to progressive joint wear and tear. The greater the mass, the more effort the joint has to make to support and move the body. This is one of the highest risk factors for chondromalacia patella.
- Demanding sports: There are intensive physical activities that expose the joint to sudden movements and constant overloads. These practices often lead to chondromalacia of the patella, even in young athletes. Add to this poor footwear or inadequate practice and the likelihood of the disease increases.
- Muscle atrophy or weakness: If there is an imbalance of muscle strength, it can cause this imbalance to put stress on the patella. For example, when the quadriceps is weaker, the rest of the motor system works in an unbalanced way. This happens because some muscles are being worked more than others, because they are atrophied or because there is a visceral dysfunction. This causes movement in the patella to occur out of alignment and leads to wear and tear.
- Rheumatoid arthritis and other diseases: The autoimmune nature of arthritis causes damage to cartilage structures. The same is true for osteoarthritis and osteoporosis. In itself, any disease that negatively affects the joints is a potential risk.
- Patellar dislocations or dislocations: Often, when exposed to pressure, the kneecap bone will move out of place or shift outwards. This will cause the knee to deform, pain and tenderness. When this happens, it is very likely that chondromalacia patellae or chondropathy will develop over time.
- Hip disruption: When the structures that make up the joint rub together or do not move as they should, wear and tear of the cartilage occurs. This can come from bone deformities, fibrous tissue or gait disturbances. Any misalignment makes it prone to the development of the disease.
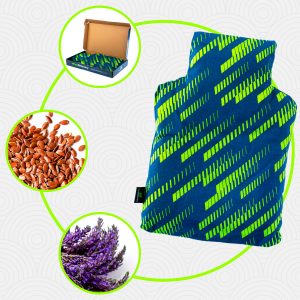
Best products for knee tendonitis
Bestseller
-
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Hearts)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Oxford)
£24,95 -
Microwave Wheat Bag for Back Pain Relief (Extra Large) (Sport)
£24,95 -
Microwaveable Wheat Bag for Pain Relief (Hearts)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Oxford)
£20,95 -
Microwaveable Wheat Bag for Pain Relief (Sport)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Hearts)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Oxford)
£20,95 -
Wheat Bag for Microwave Classic Bottle Shaped (Sport)
£20,95
Main symptoms that warn us that we have chondromalacia patellae
Learn about the symptoms that will help you detect the presence of chondromalacia patellae in time:
- Pain: Due to the overexcitation of the cartilage tissue and the overloading of the bones, there is an increased nerve sensation in this area. This is often perceived as pain, which is reflected on the sides, under and behind the kneecap. It increases when the leg is moved and rubbed.
- Swelling: As a result of cartilage damage and subsequent bone injury, the surrounding tissue swells. The stress on the area inflames the tendons, bursae and muscles. This action of the immune system is normal initially, but over the long term can lead to further damage to the structures.
- Clicking: A characteristic feature of this condition is a crackling or popping sound when carrying out movements. For example, when bending the knee, descending stairs, running or changing position, the noise heard from the joint is noticeable.
- Difficulty or stiffness of movement: Pain and swelling make it difficult to move the knee. If the person has difficulty with even slight stretching, it is possible that a previous pain has been ignored.
What treatments are available to alleviate pain due to wear and tear of the knee cartilage?
The symptoms generated by chondromalacia can be alleviated by following a logical line of treatments. At a certain point in the syndrome, cartilage cells cannot be regenerated. However, a patient with this condition can live a normal life following medical and physiotherapeutic recommendations. The important thing is that the tissue does not degrade further.
For this reason, we will show you below a list of all the treatments that are currently being applied:
Alternative and complementary therapies
Take a look at the different therapies that can be applied in an auxiliary way:
- Heat and cold therapy: The initial joint improvement is given a boost by applying heat and then cold (ending with heat again). Although in knee cases bathing is a bit uncomfortable, it can be contrasted with bags, cloths, compresses and gels. The important thing is to maintain the cold or hot temperature for an adequate time not exceeding 5 minutes of each.
- Compression therapy: Patellar tapes for chondropathy may be helpful. However, the physician should evaluate their long-term disadvantages, such as muscle weakness.
- Massage therapy: After the physician is able to reduce the initial inflammation, guided self-massage is possible, from rubbing and rubbing to defibrillate tendons to working on muscle contractures.
- Acupressure therapy: If it is necessary for the patient to find mental harmony to cope with this disease, then this oriental medicine is recommended. Acupressure helps relaxation by stimulating the nerves by pressing on different strategic parts of the body.
- Thermotherapy: Some types of thermotherapy such as infrared, moist heat, paraffin and others have analgesic effects. This is because they have a vasodilator effect on the area, and can be beneficial in chronic conditions. It should be used in moderation and under the supervision of a therapist. Above all, since it has contraindicated effects in patients with coagulation disorders.
- Natural remedies using plants: It is possible to use the relaxing and anti-inflammatory properties of plants. For this reason, ginger, peppermint, linden, chamomile and other herbs are used in this treatment. Infusion is the most commonly used method.
- Healthy lifestyle habits: A healthy lifestyle postpones the onset of chondromalacia patella. A balanced diet to maintain the ideal weight, cardiovascular and total body exercises worked in a balanced way also contribute. But more than anything else, this therapy seeks to educate the patient about the use they make of their joints.
Nutritional supplements
The following are nutrients that can be incorporated into the treatment of chondromalacia patella:
- Glucosamine sulphate: This dietary supplement can work to relieve pain. This compound is present in synovial fluid, which is a joint facilitator. The quality of the supplement and efficacy varies greatly from patient to patient. It is appropriate to seek the opinion of a health expert before deciding to take it.
- Chondroitin sulphate: Such a supplement acts as a protector. Together with glucosamine, chondroitin sulphate can be effective for patellar wear and tear. It is a relatively safe supplement to take on prescription. It is used on the premise of having antioxidant, anti-inflammatory, anabolic and anti-catabolic effects. As with other supplements, it is recommended that you consult your doctor or nutritionist before taking these products.
Physiotherapy treatments
The following therapeutic techniques can be applied in this complementary treatment:
- Electrotherapy with TENS: By means of electro-stimulators, this therapy has sedative effects. It is a type of low intensity, non-invasive nerve stimulation.
- Electrotherapy with magnotherapy: Another type of electrotherapy widely used in chondromalacia patella is magnotherapy. The specialist uses low-frequency magnetic fields to regenerate, relieve and eliminate swelling. Its aim is more focused on achieving gradual anti-inflammatory results.
- Myofascial release: Also used by physiotherapists as a means of relaxing the fascia, although in its natural state it is relaxed, it can become tense due to inflammation, stress or injury. It is performed by manual movements.
- Osteopathy: Osteopathic techniques use gentle massage directed at muscles, ligaments and joints. It is also closely related to healthy lifestyle habits, its ultimate goal being the holistic treatment to use the body properly. It can even be useful for the post-operative recovery process.
- Stretching exercises: One of the most important therapies to maintain the patient's quality of life is muscle rehabilitation. Through stretching, repetitions and gradual movements, the balance and strength of the knee is recovered.
- Global postural re-education: With regard to stretching exercises, a more advanced technique is RPG. This is based on a global or holistic treatment focused on stretching the muscles of the body gradually and decompressing them. Of course, posture education and elasticity are intimately involved.
- Proprioception training: By receiving proprioception retraining the brain becomes more aware of the position of the parts. This prevents imbalances and injuries, as well as improving muscular and articulatory ability.
Medications
This therapy must be directed and advised by the doctor in order to avoid injuries and side effects of the drugs. For this reason, self-medication is not recommended in any way, as this will aggravate the injury.
Find out which medications are commonly prescribed by doctors:
- Analgesics: These drugs are aimed at relieving the intense sensation of pain. Diclofenac, Acetylsalicylic acid, Tenoxicam and Celecoxib fall into this group.
- Topical analgesics: Because pain relief is desired, the physician may recommend another class of analgesics. These come in the form of creams, gels or patches, which are used topically directly behind the knee. That is, they are placed superficially on the skin.
- Anti-inflammatory drugs: As with other connective tissue disorders, these drugs are intended to reduce inflammation in the affected area. NSAIDS such as aspirin, naproxen and ibuprofen are the most commonly used for this purpose.
- Hyaluronic acid by means of intra-articular injections: Hyaluronic acid is a naturally occurring component of the body and is therefore part of the connective tissue, synovial fluid and skin. In addition to physiotherapeutic treatment, infiltrations with this substance balance the cellular reconstructive elements.
- Collagen infiltration: This is performed by direct application of collagen around the injured area. It is painless and is applied by injection.
- PRGF growth factors: This is a therapy based on regenerative medicine where a sample of the patient's blood is extracted to isolate certain proteins. These proteins promote tissue recovery in various ways. They provide analgesic effects and reduce inflammation. It is carried out by inserting plasma enriched in growth factors directly into the affected area.
Surgery
Arthroscopy and chondrocyte extraction and implantation are the most common surgical techniques used in more advanced cases of the disease. It must be accompanied by rest to produce the desired effects more quickly. Although it should be noted that in the vast majority of cases, this ailment does not require any surgical intervention.
What prevention methods for chondromalacia patella are the most effective?
Preventive measures are important to avoid wear and tear of the cartilage. You can take care of your knee joint by taking the following tips into account:
- Warming up beforehand: Going into intensive activity without warming up the joints first is a mistake. This increases the likelihood of injuries such as chondromalacia patella. So, whether you have suffered from this condition or not, try to warm up for half an hour to 15 minutes before training.
- Controlled exercise: Mild physical activity prevents this painful condition, as the locomotor system will be active at all times. Swimming, walking and all-round sports are a good preventive measure.
- Strengthening of the musculature: Having the muscles of the legs, whether the quadriceps or the femoral muscles, in good shape and with good muscle tone helps to relieve the pressure on the kneecap and prevents wear and tear on the kneecap.
- Avoid being overweight and sedentary: You must remember that being overweight is one of the causes of patellofemoral pain syndrome. Therefore, in order not to make continuous and exaggerated demands on the knee joint, it is necessary to find and maintain the ideal weight through recreational activities.
- Be careful when walking: The knee supports all the impacts made when walking, running or jumping. Therefore, if the feet are not fulfilling their function of supporting the body correctly, the knee will suffer.
- Wear the right footwear: You should take care of your feet by wearing the right footwear and correcting, if possible, walking faults. Shoes with high heels and excessive pressure on the heel are the least recommended for maintaining joint health.
- Maintain correct posture: While walking, standing or doing physical activities, posture is essential. Any slight imbalance in biomechanics that is constant is detrimental and can lead to chondropathy.
- Do not cross your legs frequently: This action tends to overpress the joints and twist the femur, which will lead to knee injuries in the short term.
- Avoid high-impact workouts or training: Sports or jobs that require more physical power, jumping and intensive training routines are not recommended. This is especially true for older people or those with other triggering pathologies.
References
- BENTLEY, G. (1970). Chondromalacia patellae. JBJS, 52(2), 221-232. https://journals.lww.com/jbjsjournal/Abstract/1970/52020/Chondromalacia_Patellae.2.aspx
- Levine, J. (1979). Chondromalacia patellae. The Physician and Sportsmedicine, 7(8), 39-54. https://www.tandfonline.com/doi/abs/10.1080/00913847.1979.11948468
- Warden, S. J., & Brukner, P. (2003). Patellar tendinopathy. Clinics in sports medicine, 22(4), 743-759. https://www.sportsmed.theclinics.com/article/S0278-5919(03)00068-1/fulltext
- Visnes, H., & Bahr, R. (2007). The evolution of eccentric training as treatment for patellar tendinopathy (jumper’s knee): a critical review of exercise programmes. British journal of sports medicine, 41(4), 217-223. https://bjsm.bmj.com/content/41/4/217.short
- Blazina, M. E., Kerlan, R. K., Jobe, F. W., Carter, V. S., & Carlson, G. J. (1973). Jumper's knee. Orthopedic Clinics of North America, 4(3), 665-678. https://www.sciencedirect.com/science/article/abs/pii/S0030589820323439
- Almekinders, L. C., & Temple, J. D. (1998). Etiology, diagnosis, and treatment of tendonitis: an analysis of the literature. Medicine and science in sports and exercise, 30(8), 1183-1190. https://europepmc.org/article/med/9710855
- Kainberger, F. M., Engel, A., Barton, P., Huebsch, P., Neuhold, A., & Salomonowitz, E. (1990). Injury of the Achilles tendon: diagnosis with sonography. AJR. American journal of roentgenology, 155(5), 1031-1036. https://radnuk.meduniwien.ac.at/fileadmin/radiodiagnostik/pdf/1_Kainberer_et_al_1990.pdf
- Sandmeier, R., & Renström, P. A. F. H. (1997). Diagnosis and treatment of chronic tendon disorders in sports. Scandinavian journal of medicine & science in sports, 7(2), 96-106. https://onlinelibrary.wiley.com/doi/abs/10.1111/j.1600-0838.1997.tb00125.x
- Alfredson, H., & Lorentzon, R. (2002). Chronic tendon pain: no signs of chemical inflammation but high concentrations of the neurotransmitter glutamate. Implications for treatment?. Current drug targets, 3(1), 43-54. https://www.ingentaconnect.com/content/ben/cdt/2002/00000003/00000001/art00004
- Williams, J. G. P. (1986). Achilles tendon lesions in sport. Sports Medicine, 3, 114-135. https://link.springer.com/article/10.2165/00007256-198603020-00003