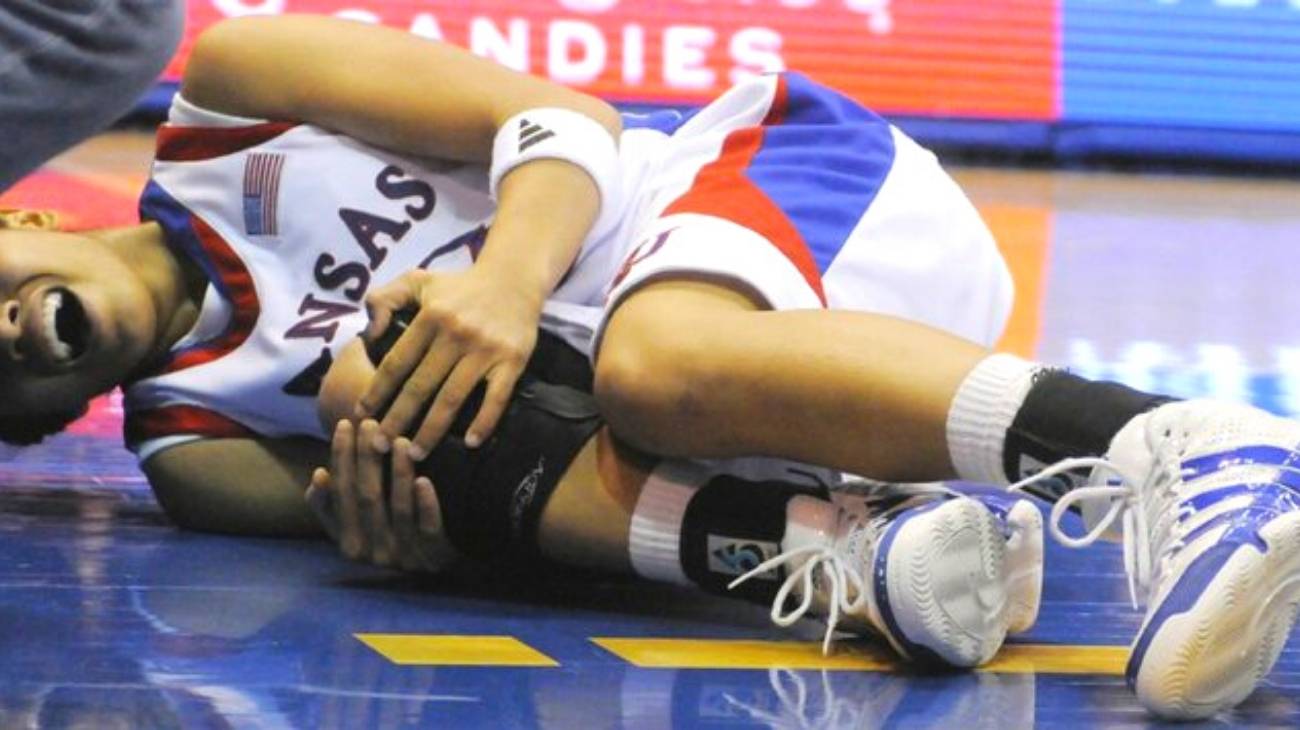
More than 45% of basketball injuries are concentrated between the legs, knees and ankles. It is a reality that we must take into account when training and especially when competing with intensity, whether we do it as professionals or amateurs.
In this article you will learn about the main types of injuries we can suffer in the lower body while playing basketball, as well as how to apply the RICE therapy effectively to minimise the impact of these injuries and alleviate the first symptoms.
What are the most common types of foot, ankle and leg injuries when playing basketball?
In both male and female athletes, there are a number of ailments and injuries that can delay careers and can cause problems. By knowing the most common basketball injuries, you become aware of the possibility of preventing them more effectively and your whole being is focused on being at 100% for the entire season.
Plantar fascia injury
Plantar fasciitis is an inflammation of the tissue that covers the entire sole of the foot, which occurs when the sole of the foot is overstretched or overloaded. It is so painful that it makes the simple act of walking difficult. Confirmation of the condition is given after an x-ray and usually requires non-invasive physiotherapy treatment to control the pain, as it is also characterised as a chronic condition.
It is not the result of a chance action during a game, but rather the accumulation of wear and tear from the jumping, cutting and punting that every basketball player does on the court over the years. If physiotherapy fails, surgery is often the only alternative to control this problem.
Achilles tendon rupture
When a movement pushes the toes upwards with great force, such as a collision with another player's calf or a sudden stop when cutting the ball, a tear occurs in the Achilles tendon. This can be partial, when only part of the ligament is torn, or complete if it separates completely. When the tear is complete, it makes walking impossible and requires the use of a splint to cover the entire ankle and may even require open surgery to stitch the cord together.
Another reason for this injury is a severe blow to the base of the heel, which is uncommon in basketball but always a possibility. Immediately there should be a medical evaluation and relative rest as directed by the treating specialist.
Ankle and knee sprains
Both joints take the full weight of the body during jogging, jumping, turning and falling. Sprains come in varying degrees and the pain will tell you how bad the injury is. The problem with them is that when there is no good recovery, there is often a recurrence. That's when you realise that following medical advice and rest is essential.
In the knees, they occur when the knee is fixed and the whole body turns unexpectedly to perform a feint, while in the ankles it happens when there is a fall when returning to the ground after a jump, in which the foot is in a good position to cushion the return of the weight to the surface.
Hamstring injury
The hamstrings are a group of three muscles and any one of them can be injured. Often only prolonged rest and occasional medication can bring a full recovery if the damage is not too deep, but more commonly surgery is required. The sudden starts and unexpected stops that basketball players constantly make are fatal combinations for this muscle group.
Best products for the recovery of ankle, foot and leg injuries in basketball
Bestseller
-
2 Calf Compression Sleeve (Black/Gray)
$19.95 -
2 Calf Compression Sleeve (Green/Navy)
$19.95 -
2 Calf Compression Sleeve (Pink/Bordeaux)
$19.95 -
2 Knee Compression Sleeve (Black/Gray)
$19.95 -
2 Knee Compression Sleeve (Green/Navy)
$19.95 -
2 Knee Compression Sleeve (Pink/Bordeaux)
$19.95 -
2 Patella Knee Strap (Black/Gray)
$14.95 -
2 Patella Knee Strap (Green/Navy)
$14.95 -
2 Patella Knee Strap (Pink/Bordeaux)
$14.95 -
2 Thigh Compression Sleeve (Black/Gray)
$19.95 -
2 Thigh Compression Sleeve (Green/Navy)
$19.95 -
2 Thigh Compression Sleeve (Pink/Bordeaux)
$19.95 -
Acupressure Mat and Pillow (Black/Gray)
$49.95 -
Acupressure Mat and Pillow (Green/Navy)
$49.95 -
Acupressure Mat and Pillow (Pink/Bordeaux)
$49.95 -
Acupressure Pillow (Black/Gray)
$29.46 -
Acupressure Pillow (Green/Navy)
$29.46 -
Acupressure Pillow (Pink/Bordeaux)
$29.46 -
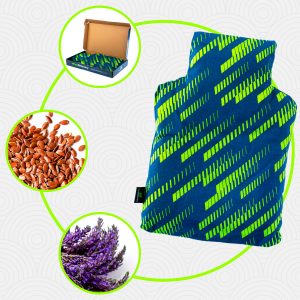
Heating Pad for Microwave Classic Bottle Shaped (Hearts)
$19.95 -
Heating Pad for Microwave Classic Bottle Shaped (Oxford)
$19.95 -
Heating Pad for Microwave Classic Bottle Shaped (Sport)
$19.95 -
High Density Foam Roller for Muscle (Black/Gray)
$24.95 -
High Density Foam Roller for Muscle (Green/Navy)
$24.95 -
High Density Foam Roller for Muscle (Pink/Bordeaux)
$24.95 -
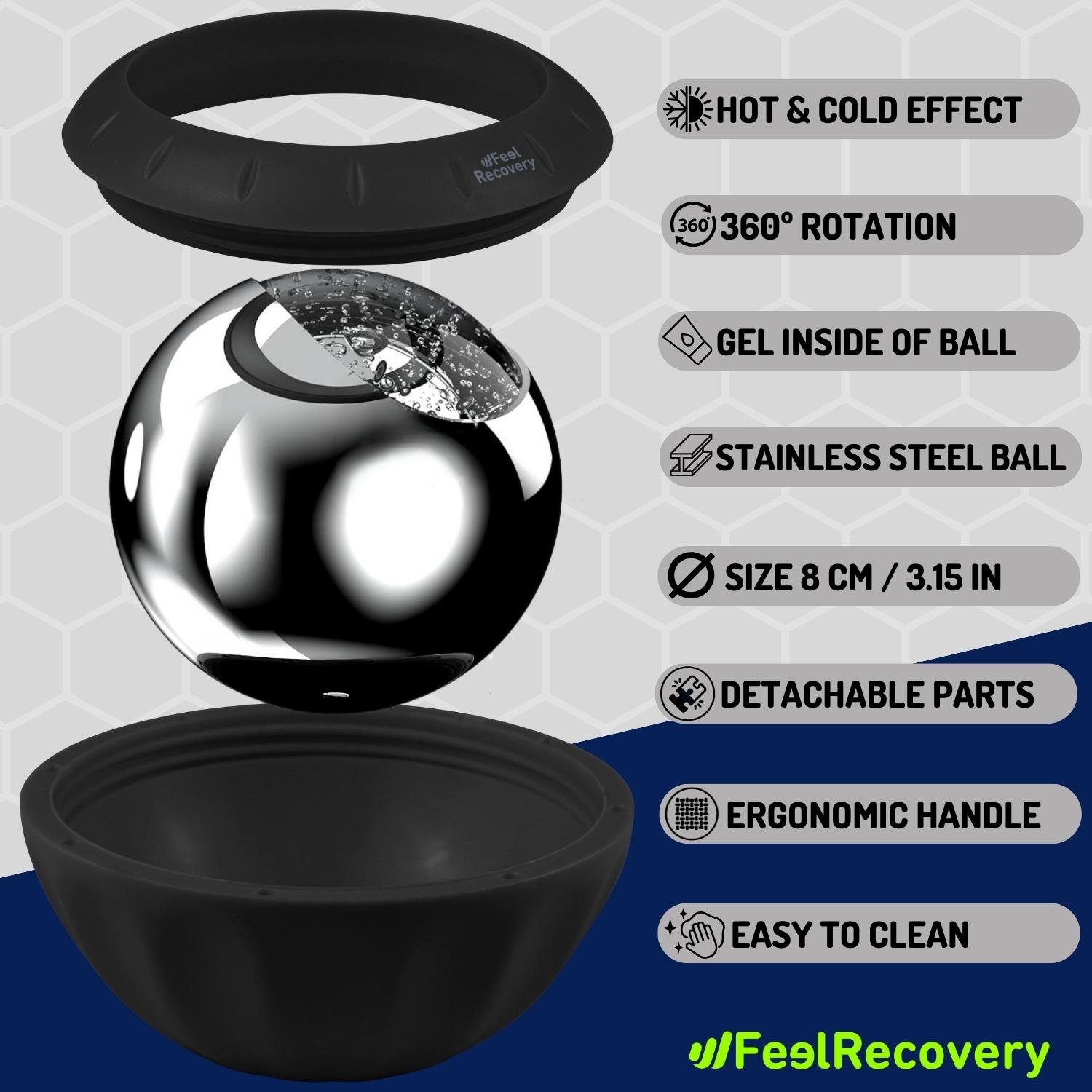
Ice Massage Roller Ball (Black)
$39.95 -
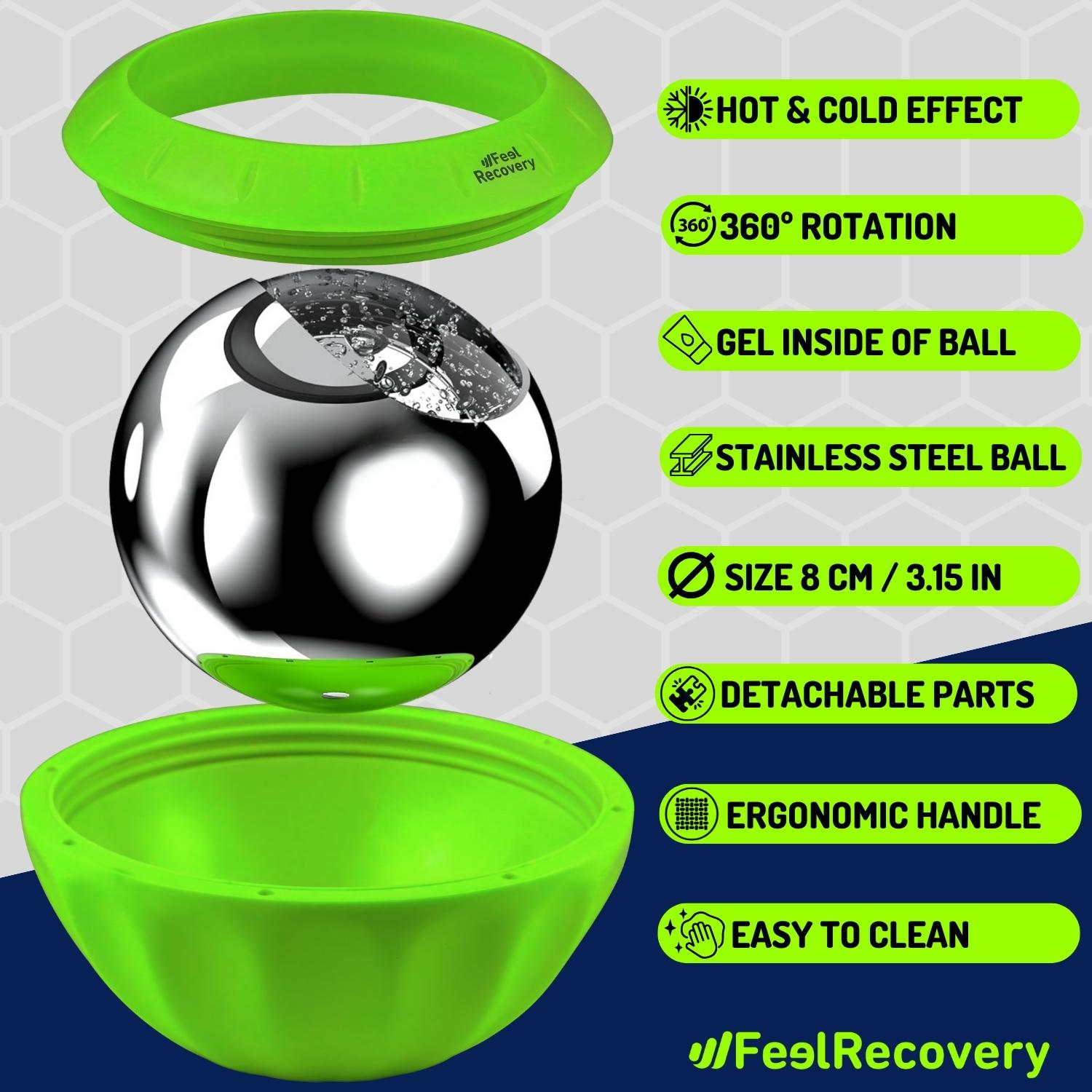
Ice Massage Roller Ball (Green)
$39.95 -
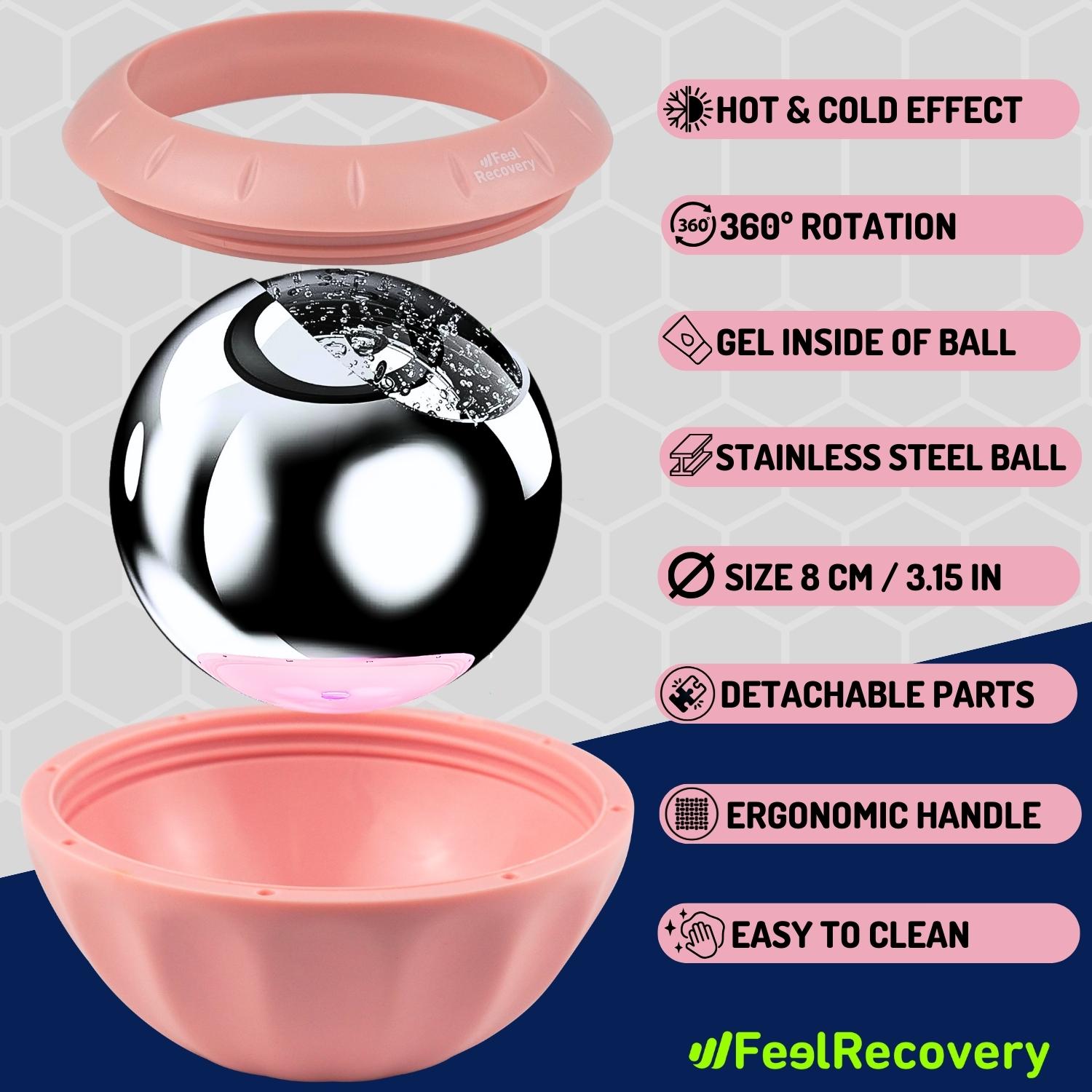
Ice Massage Roller Ball (Pink)
$39.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Hearts)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Oxford)
$29.95 -
Microwave Heating Pad for Back Pain Relief (Extra Large) (Sport)
$29.95 -
Microwaveable Heating Pad for Pain Relief (Hearts)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Oxford)
$19.95 -
Microwaveable Heating Pad for Pain Relief (Sport)
$19.95 -
Pack 2 In 1 Foam Roller High + Soft Density (Black/Gray)
$29.95 -
Pack 2 In 1 Foam Roller High + Soft Density (Green/Navy)
$29.95 -
Pack 2 In 1 Foam Roller High + Soft Density (Pink/Bordeaux)
$29.95 -
Soft Density Foam Roller for Recovery (Black)
$24.95 -
Soft Density Foam Roller for Recovery (Green)
$24.95 -
Soft Density Foam Roller for Recovery (Pink)
$24.95 -
Sport Compression Socks (1 Pair) (Black/Gray)
$19.95 -
Sport Compression Socks (1 Pair) (Green/Navy)
$19.95 -
Sport Compression Socks (1 Pair) (Pink/Bordeaux)
$19.95 -
Trigger Point Massage Stick (Black)
$14.95 -
Trigger Point Massage Stick (Green)
$14.95 -
Trigger Point Massage Stick (Pink)
$14.95
How to apply the RICE therapy to treat ankle and foot injuries in basketball?
Although this method can be used in the medium term, in this section we will show you how to apply it to minor injuries and treat them in the first few minutes, as a form of first aid. The RICE therapy is known worldwide by this abbreviation, but has been updated to the PRICE therapy which is more effective as it adds an extra step to the process.
- Protection: The affected knee or ankle should be protected either with bandages or splints, or tourniquets if it is a dislocation or fracture. It is important that the affected joint is not accidentally damaged again after the injury.
- Rest: This involves not using the affected knee or ankle, so that the injury is not aggravated by trying to use it with the ligaments or tendons in bad condition.
- Ice: Place an ice pack wrapped in a cloth on the side of the ankle or knee where the swelling is most noticeable. Leave it there for no more than 20 minutes and then remove it.
- Compression: You can use normal bandages, elastic bandages or any other product that serves to put pressure on the affected joint or muscle. Compression garments such as therapeutic knee or ankle braces can also be used so that the swelling does not progress further.
- Elevation: In this case you should lie down and raise the leg of the affected ankle or knee so that it is at a level above the heart.
References
- McKay, G. D., Goldie, P. A., Payne, W. R., & Oakes, B. W. (2001). Ankle injuries in basketball: injury rate and risk factors. British journal of sports medicine, 35(2), 103-108.https://bjsm.bmj.com/content/35/2/103
- McGuine, T. A., Greene, J. J., Best, T., & Leverson, G. (2000). Balance as a predictor of ankle injuries in high school basketball players. Clinical Journal of Sport Medicine, 10(4), 239-244. https://journals.lww.com/cjsportsmed/Abstract/2000/10000/Balance_As_a_Predictor_of_Ankle_Injuries_in_High.3.aspx
- Cumps, E., Verhagen, E., & Meeusen, R. (2007). Prospective epidemiological study of basketball injuries during one competitive season: ankle sprains and overuse knee injuries. Journal of Sports Science and Medicine, 6(2), 204-211. https://www.jssm.org/researchjssm-06-204.xml.xml
- Hosea, T. M., Carey, C. C., & Harrer, M. F. (2000). The gender issue: epidemiology of ankle injuries in athletes who participate in basketball. Clinical Orthopaedics and Related Research (1976-2007), 372, 45-49. https://journals.lww.com/corr/Abstract/2000/03000/The_Gender_Issue__Epidemiology_of_Ankle_Injuries.6.aspx
- Thacker, S. B., Stroup, D. F., Branche, C. M., Gilchrist, J., Goodman, R. A., & Weitman, E. A. (1999). The prevention of ankle sprains in sports. The American journal of sports medicine, 27(6), 753-760. https://journals.sagepub.com/doi/abs/10.1177/03635465990270061201
- Harmer, P. A. (2005). Basketball injuries. Epidemiology of pediatric sports injuries: Team sports, 49, 31-61. https://www.karger.com/Article/Abstract/85341
- Newman, J. S., & Newberg, A. H. (2010). Basketball injuries. Radiologic Clinics, 48(6), 1095-1111. https://www.radiologic.theclinics.com/article/S0033-8389(10)00121-1/fulltext
- Trojian, T. H., Cracco, A., Hall, M., Mascaro, M., Aerni, G., & Ragle, R. (2013). Basketball injuries: caring for a basketball team. Current sports medicine reports, 12(5), 321-328. https://journals.lww.com/acsm-csmr/Fulltext/2013/09000/Basketball_Injuries___Caring_for_a_Basketball.13.aspx
- Borowski, L. A., Yard, E. E., Fields, S. K., & Comstock, R. D. (2008). The epidemiology of US high school basketball injuries, 2005–2007. The American journal of sports medicine, 36(12), 2328-2335. https://journals.sagepub.com/doi/abs/10.1177/0363546508322893
- Zelisko, J. A., Noble, H. B., & Porter, M. (1982). A comparison of men’s and women’s professional basketball injuries. The American journal of sports medicine, 10(5), 297-299. https://journals.sagepub.com/doi/abs/10.1177/036354658201000507